1. What are the MRI findings?
2. How many pulleys are in each finger?
3. Which pulley is most commonly injured?
4. Which pulley is most often affected in a trigger finger?
5. Bowstringing of the tendon is best appreciated on finger extension. True or False?
Pulley injury (climber’s finger) 2308
Case ranking/difficulty: ![]()
![]()
![]() Category: Trauma
Category: Trauma
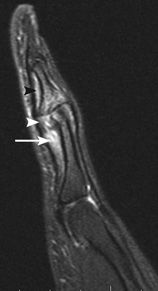
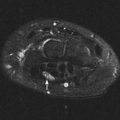
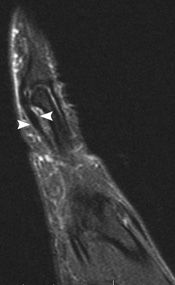
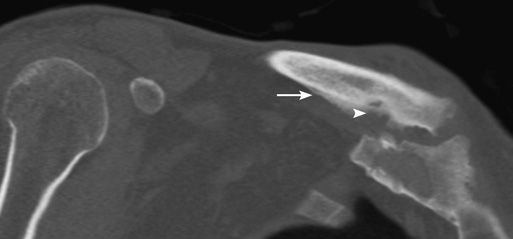
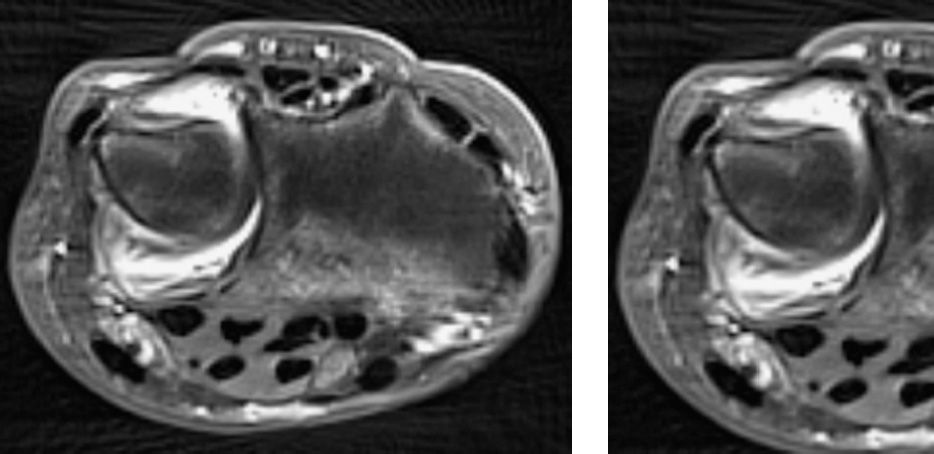
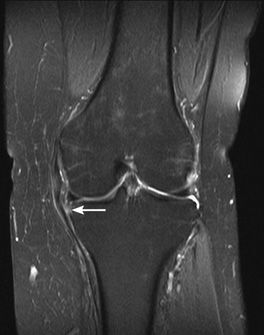
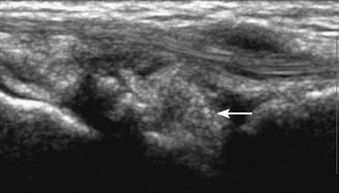
There is edema deep to the flexor tendon at the proximal phalanx, with “bowstringing” of the tendon (arrow). Heterogeneity of the volar plate consistent with injury (arrowhead). Edema deep to the tendon at the middle phalanx without bowstringing suggests low-grade A4 injury (black arrowhead).
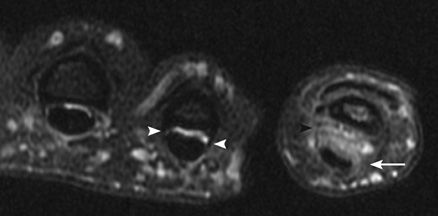
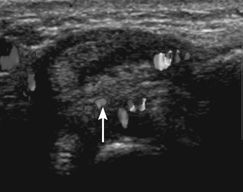
The A2 pulley shows high-grade tear medially (arrow) and intermediate-grade tear laterally (black arrowhead). There is separation of the tendon from bone with edema. Normal pulley seen in the adjacent finger (white arrowheads).

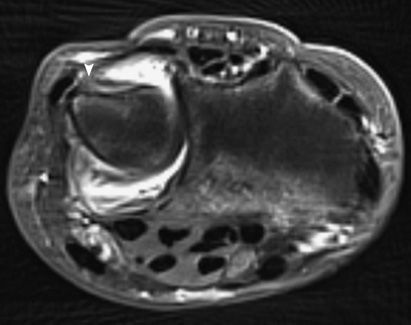
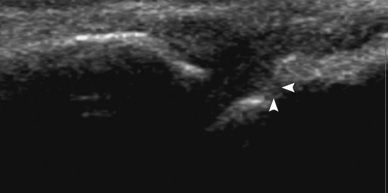
Avulsion fracture at the central slip attachment at the middle phalanx (arrowhead).
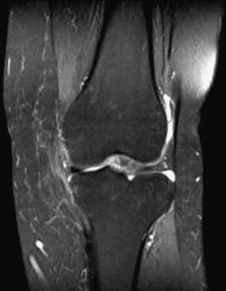
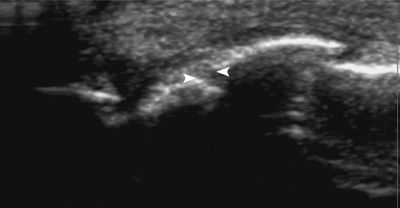
Another patient showing the mild thickening of the flexor tendon sheath consistent with the normal A2 pulley (arrowhead).
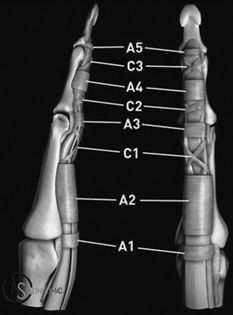
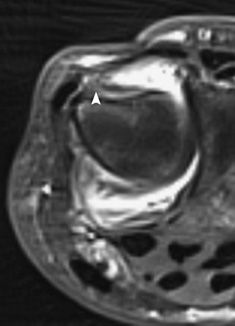
Illustration showing the finger pulleys. (Reprinted with permission from Radsource and Dr. Michael Stadnick.)
Answers
1. There is a high-grade injury to the A2 pulley with bowstringing and mild injury to the A4 pulley. There is also volar plate injury and avulsion fracture of the extensor tendon central slip insertion on the middle phalanx, with post-traumatic osteoarthritis and bone marrow edema.
2. There are 8 pulleys: 5 annular pulleys labelled A1 to A5, and 3 cruciate labelled C1 to C3.
3. The A2 pulley is the most important pulley, but also the most frequently injured. The A3 pulley is the second most injured, followed by A4.
4. The A1 pulley is most often affected in a trigger finger.
5. False. Finger flexion accentuates the bowstringing of the flexor tendon in a pulley injury, but is usually not performed because flexion may result in pain and subsequent motion artifact.
Suggested Readings
Awh MH. Pulley lesion of the fingers. MRI Web Clinic. 2005.
Hauger O, Chung CB, Lektrakul N, et al. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology. 2000;217(1):201–212.
Klauser A, Frauscher F, Bodner G, et al. Finger pulley injuries in extreme rock climbers: depiction with dynamic US. Radiology. 2002;222(3):755–761.
Pain in the hip with snapping symptoms
1. What are the MRI findings?
2. What is the differential diagnosis?
3. What is the most likely diagnosis?
4. What is the anatomy of the affected structure?
5. What leg movements exacerbates the symptoms of this entity?
Ischiofemoral impingement syndrome 1734
Case ranking/difficulty: ![]()
![]()
![]() Category: Developmental abnormalities of the musculoskeletal system
Category: Developmental abnormalities of the musculoskeletal system
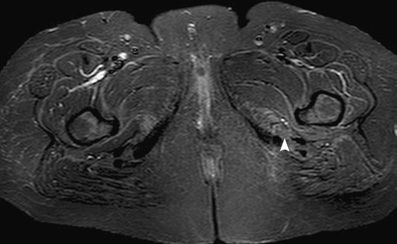
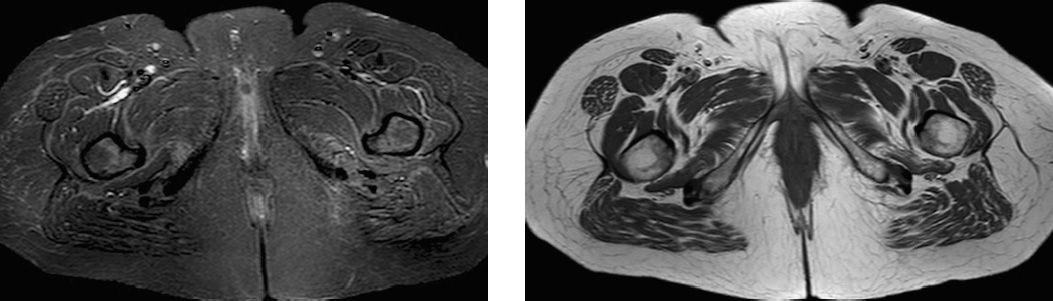
Edema in the left quadratus femoris muscle.
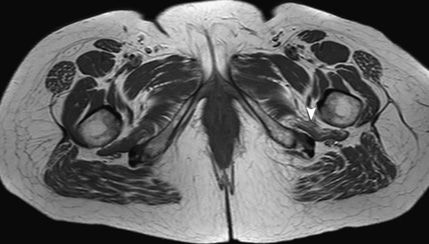
Fatty atrophy of the left quadratus femoris.
Answers
1. STIR image demonstrates edema, and high T1 signal indicates atrophy in the quadratus femoris. The ischiofemoral space is narrowed, and the quadratus femoris is atrophic in comparison to its counterparts.
2. The differential diagnoses include piriformis syndrome, iliopsoas bursitis, ischial bursitis, quadratus sprain, and acute quadratus tear.
3. Given the edema and atrophy of the quadratus femoris muscle, along with a narrowed ischiofemoral space, the diagnosis is ischiofemoral impingement.
4. Quadratus femoris is a quadrangular shape muscle that originates at the lateral margin of the obturator ring above the ischial tuberosity.
It inserts on the posterior medial aspect of the proximal femur along the quadrate tubercle of the posterior intertrochanteric region.
Superiorly the quadratus femoris is surrounded by fat and the inferior gemellus muscle, and inferiorly, it is close to the adductor magnus. The sciatic nerve is posterior and in close proximity.
5. Extension, adduction, and internal rotation are the main movements that lead to ischiofemoral impingement and subsequent pain.
Suggested Readings
Ali AM, Whitwell D, Ostlere SJ. Case report: imaging and surgical treatment of a snapping hip due to ischiofemoral impingement. Skeletal Radiol. 2011;40(5):653–656.
Kassarjian A, Tomas X, Cerezal L, Canga A, Llopis E. MRI of the quadratus femoris muscle: anatomic considerations and pathologic lesions. AJR Am J Roentgenol. 2011;197(1):170–174.
Torriani M, Souto SC, Thomas BJ, Ouellette H, Bredella MA. Ischiofemoral impingement syndrome: an entity with hip pain and abnormalities of the quadratus femoris muscle. AJR Am J Roentgenol. 2009;193(1):186–190.
Painful sternoclavicular joint with swelling and multiple skin pustules
1. What are the radiograph findings?
2. What are the CT findings?
3. What is the differential diagnosis?
4. What is the likely diagnosis?
5. What are the treatment options?
SAPHO (synovitis, acne, palmoplantar pustulosis, hyperostosis and osteitis) syndrome 1545
Case ranking/difficulty: ![]()
![]()
![]() Category: Infections in the musculoskeletal system
Category: Infections in the musculoskeletal system
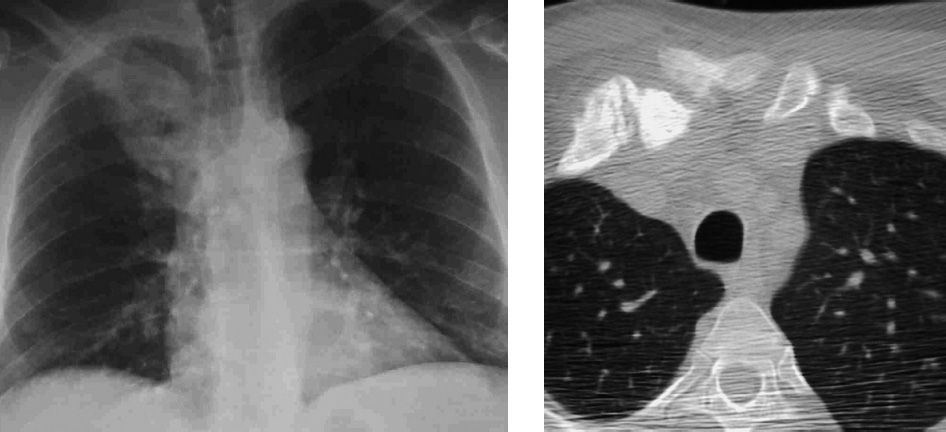
Hyperostosis, sclerosis and expansion of the medial clavicle and sternum.
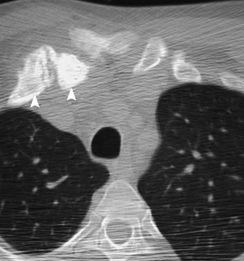
Erosion, sclerosis, hyperostosis, and expansion of the sternum.
Different patient. Extensive sclerosis of the medial clavicle (arrow) and erosions (arrowhead).
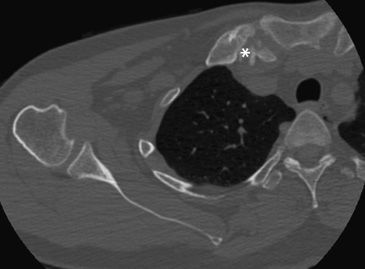
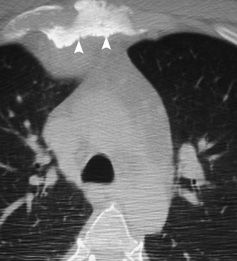
Different patient, less dramatic changes. Hyperostosis, sclerosis, and erosion (asterisk). Soft-tissue swelling is also seen.
Answers
1. Right sternoclavicular joint hyperostosis, sclerosis with erosion and soft-tissue swelling.
2. Hyperostosis, sclerosis, and erosions of the medial end of clavicle. There is also soft-tissue swelling.
3. The differential diagnosis involves bacterial, atypical or viral infection, autoimmune disease, metastasis, Ewing sarcoma, and osteonecrosis.
4. The diagnosis is SAPHO syndrome. SAPHO is an acronym for synovitis, acne, palmoplantar pustulosis, hyperostosis and osteitis.
5. The treatment options include analgesics, anti-inflammatory drugs, bisphosphonates, and immunomodulators.
Suggested Readings
Depasquale R, Kumar N, Lalam RK, et al. SAPHO: What radiologists should know. Clin Radiol. 2012;67(3):195–206.
Sweeney SA, Kumar VA, Tayar J, et al. Case 181: synovitis acne pustulosis hyperostosis osteitis (SAPHO) syndrome. Radiology. 2012;263(2):613–617.
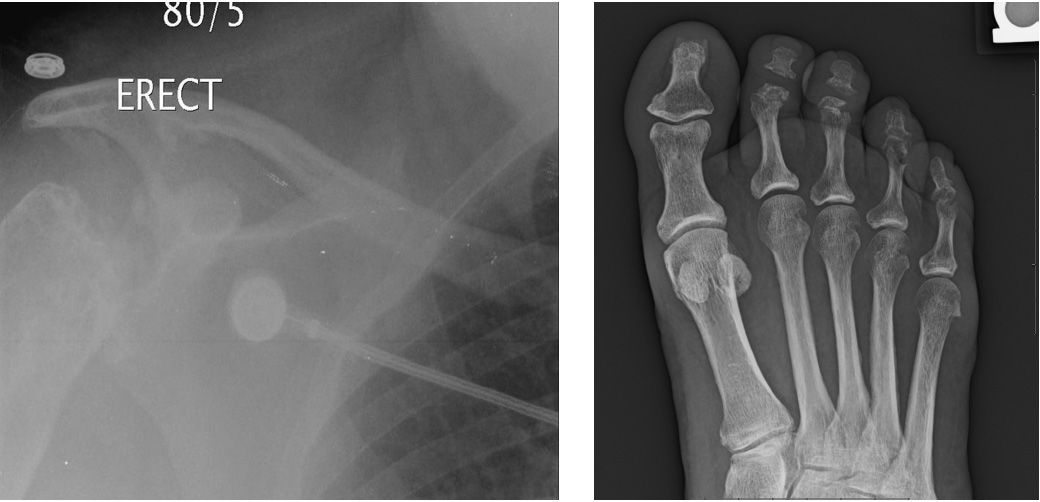
Painful and swollen digit

1. What is the descriptive term used for this entity?
2. In which age group is this condition most prevalent?
3. What is the differential diagnosis?
4. What are the possible treatments for this condition in other bones?
5. What are the most common digital bones to be involved with this condition?
Tuberculous dactylitis 1715
Case ranking/difficulty: ![]()
![]()
![]() Category: Infections in the musculoskeletal system
Category: Infections in the musculoskeletal system

Soft-tissue swelling around fourth and fifth proximal phalanges. Expansion of digits with lucency and destruction of medial cortex.

Corresponding fat-suppressed MRI image demonstrates high T2 weighted signal in the shaft of the third to fifth proximal phalanges with significant edema and cortical destruction.
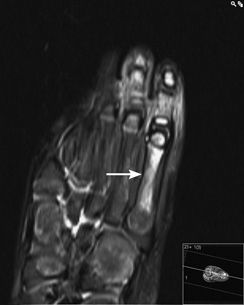
Fat-suppressed MRI demonstrates high signal within the fifth metatarsal in addition consistent with TB osteomyelitis.
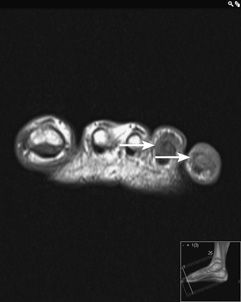
Marrow signal change (low T1) is seen in both fourth and fifth digits, which is typical of osteomyelitis. (Image courtesy of Dr. Denis Remedios.)
Answers
1. Spina “ventosa” means “wind-filled” and is a descriptive term used because of the appearance of expansion and multiple air-like lucencies. It is a typical feature of tuberculous digital osteomyelitis.
2. Eighty-five percent of patients with TB dactylitis are younger than the age of 6 years.
3. Lung cancer metastasis would not be found in the young age group. Sarcoidosis may look very similar, although again is found in a different age group (20 to 40 years of age). In a patient of this age group, however, TB and sarcoid would still both be in the differential. Leukemia may have similar appearances and has a large soft-tissue component.
4. Antituberculous chemotherapy is normally sufficient treatment for TB osteomyelitis. Occasionally, surgical curettage or fixation of a pathological fracture may be required.
5. The most common digits to be involved are the proximal phalanges of the index and middle fingers.
Suggested Readings
Malik S, Joshi S, Tank JS. Cystic bone tuberculosis in children—a case series. Indian J Tuberc. 2009;56(4):220–224.
Ritz N, Connell TG, Tebruegge M, Johnstone BR, Curtis N. Tuberculous dactylitis—an easily missed diagnosis. Eur J Clin Microbiol Infect Dis. 2011;30(11):1303–1310.
Sunderamoorthy D, Gupta V, Bleetman A. TB or not TB: an unusual sore finger. Emerg Med J. 2001;18(6):490–491.
1-day-old male with a history of deformity

1. What are the radiographic findings?
2. What are the presumed etiologies?
3. What are included in the differential, and what is the most likely diagnosis?
4. What are the typical radiological features in this entity?
5. What is the management?
Congenital bowing of the tibia 1437
Case ranking/difficulty: ![]()
![]()
![]() Category: Developmental abnormalities of the musculoskeletal system
Category: Developmental abnormalities of the musculoskeletal system

Comparison case of Blount disease, showing bowing in the medial–lateral plane.
Answers
1. There is posteromedial bowing of the tibia and fibula, with cortical thickening of the tibia. Mild cortical thickening of the femur is also seen.
2. An abnormal intrauterine position is the likely etiology, although fetal vascular insufficiency and localized skeletal dysplasia have also been implicated.
3. Tibial bowing can be seen in fibula hemimelia, neurofibromatosis, Blount disease, and physiological and congenital tibial bowing. The most likely diagnosis, based on age and direction of bowing, is congenital tibial bowing.
4. In congenital bowing, there is posteromedial bowing of the tibia and fibula with diaphyseal broadening and cortical thickening of the concave tibial cortex. Pseudoarthrosis occurs in neurofibromatosis.
5. Gradual remodelling occurs, so management is typically conservative or with bracing. If there is significant leg-length discrepancy, an osteotomy and leg lengthening may be performed, which may be combined with a contralateral epiphysiodesis.
Suggested Readings
Cheema JI, Grissom LE, Harcke HT. Radiographic characteristics of lower-extremity bowing in children. Radiographics. 2003;23(4):871–880.
Hofmann A, Wenger DR. Posteromedial bowing of the tibia. Progression of discrepancy in leg lengths. J Bone Joint Surg Am. 1981;63(3):384–388.
History of rheumatoid arthritis; wrist pain
1. What are the MRI findings?
2. What is the typical mechanism of injury?
3. What are the restraints of the extensor carpi ulnaris (ECU) tendon?
4. Where does the ECU subsheath typically tear?
5. What tears has the worse prognosis, and what is the treatment for that tear?
Extensor carpi ulnaris (ECU) subluxation and subsheath tear 1425
Case ranking/difficulty: ![]()
![]()
![]() Category: Metabolic conditions affecting bone
Category: Metabolic conditions affecting bone
There is ulnar subluxation of the extensor carpi ulnaris (ECU) tendon. The ulnar aspect of the ECU subsheath is torn (arrowhead).
Magnified view shows ECU subluxation and subsheath tear (arrowhead).

Cystic erosions from rheumatoid arthritis, and wrist and DRUJ effusions.
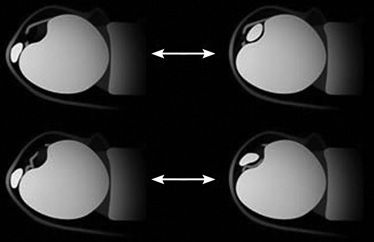
Ulnar-sided subsheath tears (top row) typically result in transient dislocation of the tendon followed by relocation upon pronation, with the tendon returning to a position beneath the subsheath. With radial-sided tears (lower diagrams), the tendon is more likely to lie on top of the torn subsheath following relocation. Outer line is the retinaculum, inner line is the subsheath. (Reprinted with permission from Radsource and Dr. Michael Stadnick.)
Answers
1. Tear of the ulnar attachment of the extensor carpi ulnaris (ECU) subsheath, with ulnar subluxation of the ECU tendon. There are also wrist and distal radioulnar joint effusions with synovitis.
2. Repetitive supination as in golf or tennis, distal radius and Galeazzi fractures, and rheumatoid arthritis have all been implicated in ECU subsheath tears and ECU subluxation.
3. The ECU subsheath is the major restraint of the ECU tendon. The subsheath also attaches near the base of the ulnar styloid process, and fractures of the styloid process result in instability of the ECU.
4. Ulnar attachment tears of the subsheath are most common, followed by radial attachment tears.
5. Radial tears have the worst prognosis. Management is typically conservative with casting in extension and radial deviation. Some authors advocate reconstructing the subsheath acutely.
Suggested Readings
Awh MH. Extensor carpi ulnaris subsheath injury. MRI Web Clin. February 2009.
Inoue G, Tamura Y. Recurrent dislocation of the extensor carpi ulnaris tendon. Br J Sports Med. 1998;32(2):172–174.
Pain following remote knee injury

1. What is the abnormal structure in the radiograph?
2. What is the probable mechanism of injury?
3. What are the common associated soft-tissue injuries?
4. What is the imaging modality of choice for this entity?
5. What is the treatment for this entity?
Reverse segond fracture 1651
Case ranking/difficulty: ![]()
![]()
![]() Category: Trauma
Category: Trauma

Avulsion fracture of medial tibial plateau consistent with a “reverse Segond” fracture.
Avulsion of medial tibial plateau by deep fibers of MCL. There is edema in the MCL consistent with a partial tear.
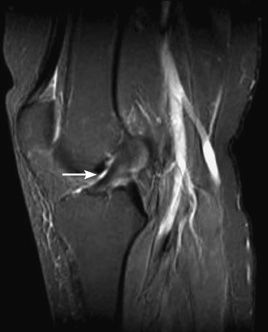
The ACL and PCL are intact in this patient, although they can be damaged with this mechanism of injury and should be carefully evaluated.
The lack of marrow edema, effusion, and other injuries are relatively unusual, although it is possible the injury occurred some time previously and the patient presented late.
Answers
1. The reverse Segond injury describes a medial capsular avulsion.
2. In common with pure MCL injuries, the presence of a medial capsular avulsion is strongly suggestive of a valgus strain injury mechanism. With this injury there is often a component of external rotation associated.
3. The reverse Segond fracture is strongly associated with tears of the deep fibers of the MCL, medial meniscus (especially root), and posterior cruciate ligament.
4. Although plain films are adequate initially to demonstrate the fracture, an MRI is mandatory to assess the extent of internal derangement, which is the more significant finding.
5. The fracture itself needs no treatment per se; however, the extent and grade of soft tissue injuries, in particular medial meniscal and MCL, determines the need for surgery. The PCL is usually not surgically repaired.
Suggested Readings
Escobedo EM, Mills WJ, Hunter JC. The “reverse Segond” fracture: association with a tear of the posterior cruciate ligament and medial meniscus. AJR Am J Roentgenol. 2002;178(4):979–983.
Gottsegen CJ, Eyer BA, White EA, Learch TJ, Forrester D. Avulsion fractures of the knee: imaging findings and clinical significance. Radiographics. 2008;28(6): 1755-1770.
Hall FM, Hochman MG. Medial Segond-type fracture: cortical avulsion off the medial tibial plateau associated with tears of the posterior cruciate ligament and medial meniscus. Skeletal Radiol. 1997;26(9):553–555.
Patient with longstanding chronic condition who is on treatment
1. What are the ultrasound findings?
2. What is the differential diagnosis?
3. What is the role of ultrasound in monitoring the response to therapy?
4. What is the best scanning technique when evaluating the MCP joints?
5. What is the most reliable method of assessing disease activity?
Rheumatoid arthritis of hands (ultrasound) 1378
Case ranking/difficulty: ![]()
![]()
![]() Category: Metabolic conditions affecting bone
Category: Metabolic conditions affecting bone
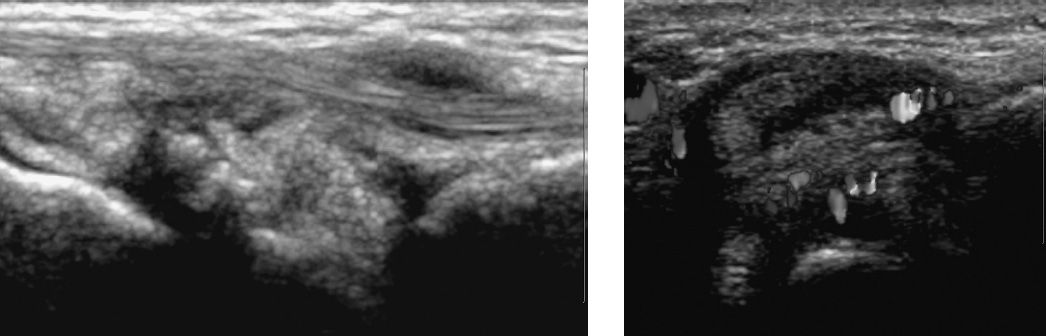
Echogenic pannus in the joint space.
Minimal vascularity in and around the pannus.
Small erosion is seen.
Small erosion is seen.
Answers
1. The ultrasound images show echogenic pannus in the MCP joint spaces with mildly increased vascularity. Minimal joint effusion and small erosions are seen. The increased vascularity is usually more intense, but this patient had been on Disease-Modifying antirheumatic Drugs.
2. Ultrasound is sensitive but nonspecific, so any inflammatory arthritis, including RA, gout, CPPD, and septic arthritis, would be included. The multiplicity of joints in this case excludes septic arthritis. Osteoarthritis would be expected to show osteophytes, but they are not demonstrated here.
3. Ultrasound will show changes in effusion, erosions, pannus size, and vascularity, and is an effective way of monitoring response to treatment.
4. A high-frequency probe (12 to 18 MHz), with power Doppler is used. A volar approach has been said to be superior to dorsal imaging.
5. Both MRI and quantitative power Doppler ultrasonography are effective in measuring the response of rheumatoid arthritis to therapy and to assess disease activity.
Suggested Readings
Lopez-Ben RR. Assessing rheumatoid arthritis with ultrasound of the hands. AJR Am J Roentgenol. 2011;197(3):W422.
Platzgummer H, Schueller-Weidekamm C. Radiological imaging in early diagnosis of rheumatoid arthritis: the role of ultrasound and magnetic resonance imaging [in German]. Radiologe. 2012;52(2):124–131.
History of chronic disease and pain in the bilateral shoulders
1. What are the radiograph findings?
2. What other entities are included in the differential diagnosis?
3. What is the most likely diagnosis?
4. What is the pathophysiology of this condition?
5. Which joints are typically affected in this condition?
Multicentric reticulohistiocytosis 1459
Case ranking/difficulty: ![]()
![]()
![]() Category: Metabolic conditions affecting bone
Category: Metabolic conditions affecting bone

Joint space widening, erosions and cystic change. Changes are bilateral.

Multiple raised skin lesions.
Answers
1. Joint space widening, erosions, cystic change, and no periosteal reaction.
2. Gout, rheumatoid arthritis, psoriatic arthritis, neuropathic shoulder, sarcoid, and multicentric reticulohistiocytosis.
3. Given the presence of raised nodular skin lesions and a destructive arthritis with no periosteal reaction or sclerosis, the most likely diagnosis is multicentric reticulohistiocytosis.
4. Multicentric reticulohistiocytosis is characterized by the deposition of multinucleated giant cells in the skin, joints, and bones.
5. The PIP and DIP joints of the hands are most commonly involved, although any joint may be affected.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree