Functional imaging techniques are increasingly being used to monitor response to therapies, often predicting the success of therapy before conventional measurements are changed. This review focuses on magnetic resonance imaging (MRI) depicted water diffusivity as a tumor response parameter. Response assessments are undertaken by noting changes in signal intensity on high b-value images or by using measurements of apparent diffusion coefficient values. The different diffusion-weighted (DW)-MRI appearances in response to treatment of soft tissue disease and bone metastases are discussed. DW-MRI changes observed in response to cytotoxics, radiotherapy, antiangiogenics, embolization, and thermocoagulation are detailed.
Application of morphologic imaging to the evaluation of tumor response to treatment has led to the emergence of response criteria such as those proposed by the Response Evaluation Criteria in Solid Tumors (RECIST) committee. However, there is increasing awareness that anatomic approaches have significant limitations, including tumors that cannot be measured, poor measurement reproducibility, and masses that persist following therapy. Faced with these limitations, more sophisticated measurement criteria (such as tumor volume) and new morphologic approaches (such as changes in tumor computed tomography [CT] density values after contrast medium administration) have been applied to the evaluation of therapy response.
However, with the increasing clinical use of cytostatic therapeutics, there is a recognition that anatomic evaluations are insensitive to changes that may inform on overall therapeutic success. This latter point has been exemplified by:
- 1.
Numerous clinical studies showing survival advantages for antiangiogenic therapies with only modest anatomic responses for glioblastoma and hepatocellular, colorectal, and renal cancers
- 2.
Studies which, in contradistinction, that have shown improvements in progression-free survival (gauged morphologically) but with no subsequent benefits in overall survival, for colorectal and breast cancer patients treated with the antiangiogenic drug bevacizumab
Both of these observations suggest that the value of anatomic imaging as a surrogate marker of clinical efficacy for antiangiogenic therapies may be limited.
To overcome the limitations of anatomic evaluations, functional imaging techniques are increasingly being used to monitor response to therapies with novel mechanisms of action, which can predict the success of therapy before conventional measurements of size are altered. In the latter setting, functional imaging methods are also being used as pharmacodynamic biomarkers of response in early phases of drug development of compounds with novel mechanisms of action, to see whether tumor physiology is correspondingly altered so as to provide confidence to proceed to more expensive efficacy studies.
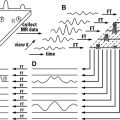
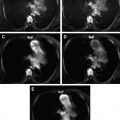
In this article the authors focus on diffusion-weighted magnetic resonance (DW-MR) imaging as a functional response imaging technique. The authors have assumed that readers are already familiar with the DW-MR imaging data acquisition techniques, including apparent diffusion coefficient (ADC) map generation (these aspects are discussed elsewhere in this issue and in the supporting medical literature). For readers interested in imaging parameters used to acquire the illustrative material in this text, refer to Table 1 . The authors begin by demonstrating the link between ADC and tissue cellular density, reflecting tumor proliferation. Key data are then presented on changes in DW-MR imaging in response to therapies that cause tumor cell death and those that affect tumor vascularity. The article focuses on experience gained in extracranial human studies, seeking to use the more extensive animal literature for support and to point out new avenues for data exploration. The authors show that MR imaging–depicted water diffusivity can reflect the interaction between the mechanism of action of therapies and tissue microstructural properties. It will become clear that therapy-induced changes in soft tissues and bone marrow differ when imaged by DW-MR imaging, depending on the mechanism of action of the treatments used; these differences are highlighted.
| Machine Parameters | Free-Breathing Multiple Averaging: Abdomen | Free-Breathing Multiple Averaging: Pelvis | Whole Body DW-MR Imaging |
|---|---|---|---|
| Field of view | 280–400 cm | 260 cm | 380–400 cm |
| Matrix size | 128i | 160–256 | 128i |
| TR | >2500 ms | >3500 ms | >6000 ms Multiple stations as required to the body |
| TE | min | min | min |
| NSA | 4–7 | 6 | 6 |
| Fat suppression | SPAIR/STIR | SPAIR/STIR | STIR |
| EPI factor | 128 | 114 | 47 |
| Parallel imaging factor | 2 | 2 | 2 |
| Section thickness | 5–7 mm/1 mm gap | 6 mm/1 mm gap | 5 mm/0 mm overlap |
| b-values (s/mm 2 ) | 3–4 b-values including 0, 100, 500, and 750 | 0, 100, 800 | 0–50 and 800–1000 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree