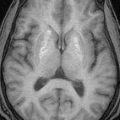
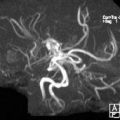
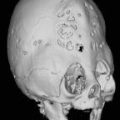
1. The persons performing the procedure should review the patient’s chart and familiarize themselves with his/her problems. Particular attention should be paid to prior noninvasive neurovascular studies (i.e., MRA, CTA, and sonograms).
2. Consent should be obtained before the patient is brought to the angiography suite. Risks and complications include bleeding, infection, damage to nerves and blood vessels, paralysis, dificulty with speech and vision, stroke, allergic reaction, and death.
3. If the patient is on heparin drip, have the drip discontinued approximately 4 hours before the angiogram to allow the patient’s PT and ATT to normalize. If possible, oral anticoagulants should be discontinued ideally 7 days (minimum of 3 days) before procedure and then the PT/PTT checked. If the angiogram needs to be performed on an emergency basis, fresh frozen plasma needs to be administered to the patient. For patients taking aspirin, bleeding time should also be obtained. If possible, discontinue aspirin 7 to 10 days before procedure. Many angiograms need to be done with an anticoagulated patient to avoid ischemic complications; risk of groin hematoma is higher in such patients.
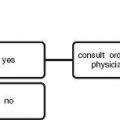
4. If previous allergic reactions have been severe (involving respiratory or cardiovascular system or angioneurotic edema), arrange for anesthesiologist to stand by.
5. Assess the patient’s femoral, popliteal, and dorsalis pedis pulses, and as a rule of thumb, puncture the groin with the strongest pulse. We generally puncture the right side due to the setup of the angiographic equipment. If the patient is hemiplegic, puncture that side as it will be least prone to motion after the angiogram.
6. Always inject first the vessels suspected to best demonstrate the pathology.
7. As a rough rule, most neuroangiographic catheters measure between 90 and 120 cm in length. The use of the following preformed catheters is suggested in the following situations:
a. Aortic arch—5 Fr (French) pigtail (however, any other 5 Fr single end-hole catheter being used usually sufices).
b. Cerebral angiogram in a young adult patient—5 Fr Berenstein, H1H, or JB2.
c. Cerebral angiogram in an older patient—5 Fr Simmons 1, 2, or 3; H1H; or Berenstein.
d. If you cannot get a vessel before switching catheters, try a difierent wire f rst.
e. When having problems with the
i. Left vertebral artery, try using H1H or Berenstein catheters.
ii. Left common carotid artery (CCA), try using a Newton or a Simmons 1 or 2 catheter.
f. In carotid stenoses workup, consider a reverse-curve catheter, such as a Simmons 2 or 3, in order to avoid passage of guide wire to or through the stenotic bifurcation area. Be careful and avoid formation of “knots.”
8. Nonionic contrast media is used for all neuroangiograms. Those with the lowest osmolarity are best for injections of the external carotid artery as they cause less pain.
a. Adults:
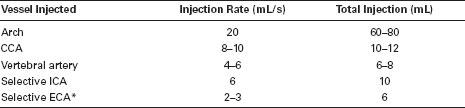
*Filming sequence is 2 to 4 frames per second using digital subtraction equipment. If rotational digital angiography and/or 3-D are used, higher doses of contrast material and longer injections are needed (check manufacturer’s instructions). Vascular malformations and other high-flow lesions may require faster filming rates. Severely stenotic or occluded vessels may require slower filming rates. CCA, common carotid artery, ICA, internal carotid artery, ECA, external carotid artery.
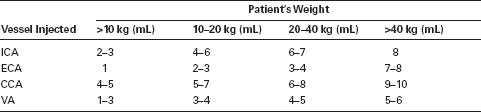
b. Children:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree