Congenital Anomalies of the Esophagus
Overview
Many congenital lesions affect esophageal morphology and function. Duplications may be asymptomatic or may be manifested with respiratory or swallowing problems. Esophageal atresia is a complex anomaly, frequently accompanied by anomalies of other organ systems. These disorders are described in Chapter 113 .
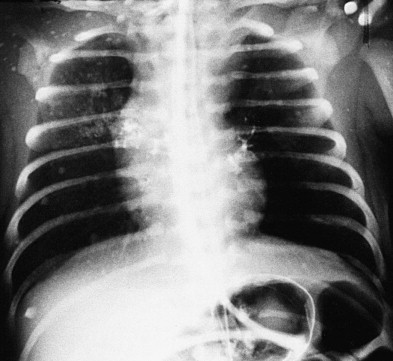
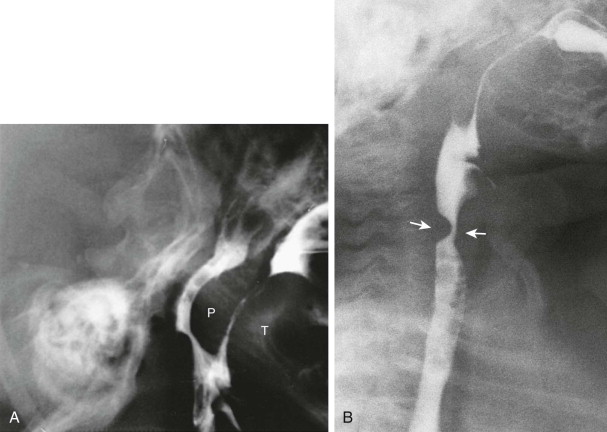
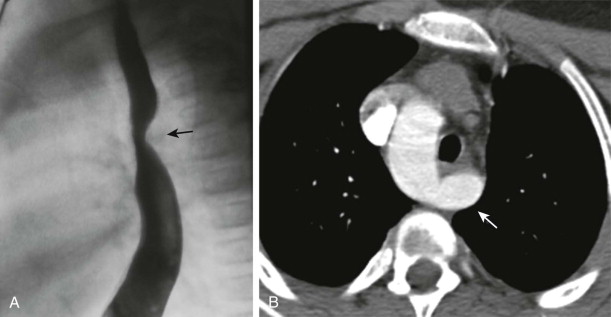
Some congenital bronchopulmonary foregut malformations, such as agenesis and congenital stenosis of the trachea, are rare and may be associated with esophageal atresia ( Fig. 115-1 ). Also included in the spectrum of bronchopulmonary foregut malformations is esophageal bronchus, characterized by communication between an isolated portion of lung and the esophagus ( Fig. 115-2 ).
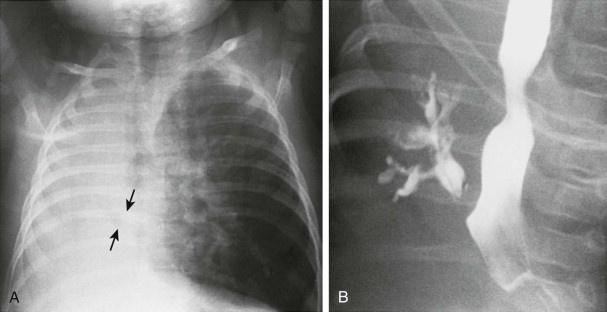
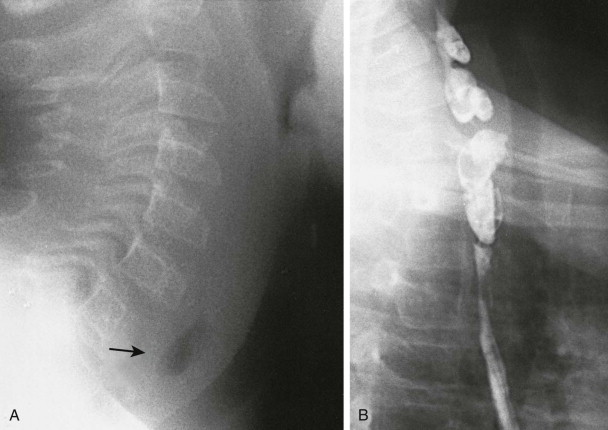
Webs and diverticula are also uncommon and may be manifested in childhood with mucosal inflammation and dysphagia ( Fig. 115-3 ). Esophageal diverticulum may be an isolated finding or a manifestation of Ehlers-Danlos syndrome. In neonates, a posteriorly directed diverticulum should be differentiated from a cavity produced by traumatic passage of a nasogastric or endotracheal tube.
Ectopic gastric or respiratory epithelium and tracheal cartilage in the esophagus are associated with focal narrowing and dysphagia. Although the incidence of ectopic gastric mucosa in the upper esophagus approaches 21% in pediatric autopsy series, these cases are rare clinically.
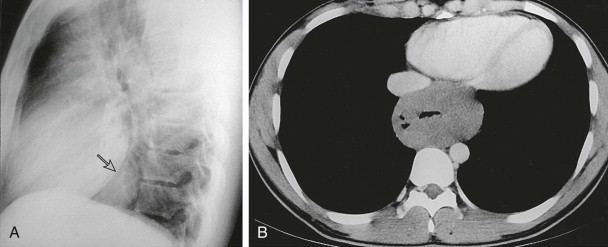
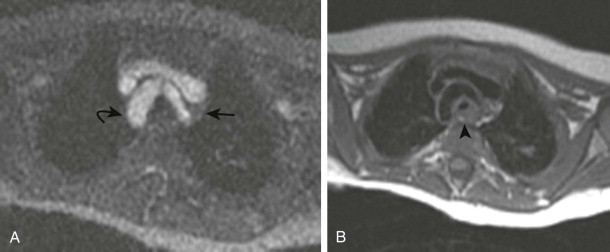
Intramural leiomyomas in children may be familial, syndromic, or isolated. They may produce luminal esophageal narrowing and may be difficult to differentiate from other masses of the middle mediastinum by imaging ( Fig. 115-4 ). Leiomyoblastomas may arise in the esophageal wall in association with other pathologic anomalies, such as pulmonary chondromas.
Swallowing Disorders
Derangement of the oral portion of swallowing may be due to congenital anomalies, such as absence of the tongue, macroglossia, cleft palate, and micrognathia. Acquired swallowing problems often result from neurologic disorders, such as cerebral palsy, cranial trauma, meningomyelocele, or central nervous system tumors.
All stages of the swallowing process (oral, pharyngeal, and esophageal) should be observed as part of a real-time, videofluoroscopic swallowing examination, which is an excellent method for assessing oropharyngeal swallow biomechanics and can be performed with minimal radiation dose. Older children are given age-appropriate foods to assess completeness of mastication and the ability to centralize the food within the oral cavity. Some children swallow liquids and puréed foods well but have difficulty swallowing solids. The modified barium swallow is performed with the child in a supported semiupright position, simulating the way the child usually eats. Maneuvers to augment swallowing (e.g., stroking the cheek, additional chin and head support) are more easily performed in this position as well.
Neuromuscular disorders can affect multiple anatomic locations that disrupt the normal swallowing process. Organs that may be impaired include the tongue, which causes poor bolus formation; the palate, which causes nasopharyngeal reflux ( Fig. 115-5A ); the epiglottis, which causes tracheal penetration or aspiration; the pharynx, which causes poor emptying and premature laryngeal “spillage”; and the cricopharyngeal muscle, which causes obstruction of the passage of the bolus. Failure of cricopharyngeal muscle relaxation is called cricopharyngeal spasm or cricopharyngeal bar and occurs transiently in some normal children ( Fig. 115-5B ).
Swallowing studies should be performed in conjunction with a speech or occupational therapist who can determine the optimal food volume and feeding implements and may perform compensatory maneuvers that assist swallowing. The examination should be recorded on videotape or digital medium to allow subsequent review.
Vascular Rings
Clinical Findings
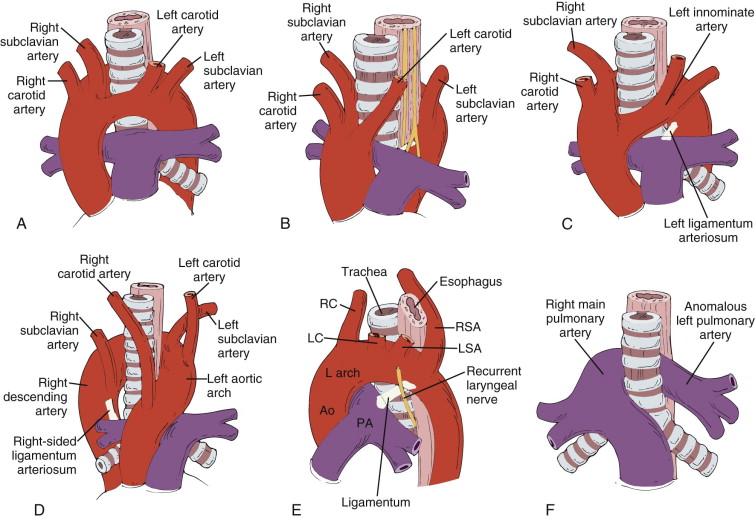
Vascular rings occur when the esophagus and trachea are encircled, displaced, or compressed by the aorta, its branches, or remnants of the fetal circulation. Some rings are incomplete, but others, such as the double aortic arch, completely surround and frequently compress the esophagus and trachea ( Fig. 115-6 ).
Asymptomatic rings are often incidentally discovered on chest radiographs. In childhood, vascular rings commonly are manifested with stridor during feeding because transient esophageal dilation produces additional tracheal compression; adults instead tend to have dysphagia as a presenting symptom. Reflex apnea is another presentation and may prompt urgent surgery. Twenty percent of these children also have congenital heart disease.
The double aortic arch, the most common vascular ring, is usually formed by the larger and more cephalad right aortic arch and the smaller and more caudad left aortic arch. The second most common ring occurs if an aberrant right subclavian artery arises as the last rather than the first branch of a left aortic arch. To reach its normal position, this vessel must pass from left to right in an oblique, cephalad direction, indenting the posterior aspect of the esophagus. If the left subclavian artery arises as the last branch of a right aortic arch, it produces more tracheal and esophageal impingement because the subclavian originates from the usually small but space-occupying diverticulum of Kommerell, and the normal left-sided ligamentum arteriosum persists.
The right innominate artery, the first vessel to arise from the aorta, originates completely or partially to the left of midline in most children. As it crosses from left to right, it may indent the anterior aspect of the trachea. Because many children with this finding are asymptomatic and many symptomatic children outgrow the symptoms, the aberrant right innominate artery is often considered to be a normal variant. Severely symptomatic children may respond to innominopexy, a surgical procedure that elevates and fixes the artery away from the trachea.
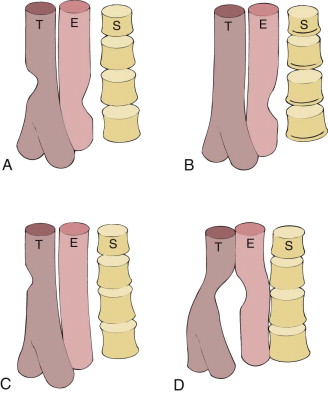
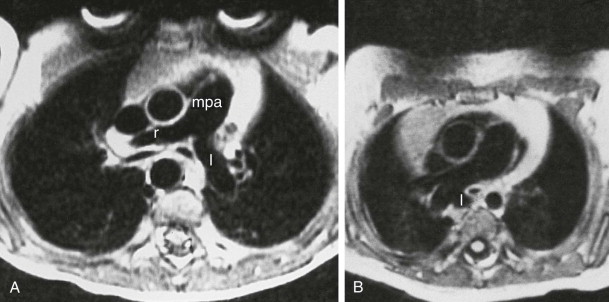
A vascular sling is an anomaly of the pulmonary artery in which the left pulmonary artery arises in an aberrant fashion from the right pulmonary artery, rather than normally from the main pulmonary artery. The anomalous left pulmonary artery courses from the right to the left in the space between the trachea and esophagus. Children with pulmonary sling have an increased incidence of intracardiac and bronchial anomalies, including ventricular septal defects and variations in the normal branching pattern.
Imaging Findings
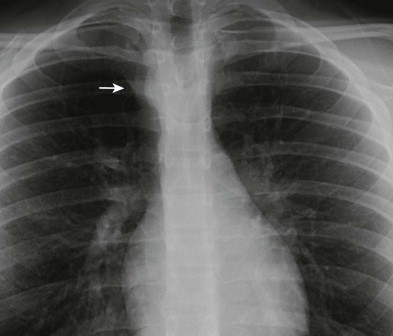
Plain radiographs can often suggest the diagnosis of a vascular ring. On the frontal view of the airway or chest, the position of the aortic arch and trachea should always be carefully evaluated ( Figs. 115-7 and 115-8 ). The presence of a right aortic arch in a child with respiratory symptoms suggests that there may be a double aortic arch or right aortic arch with an aberrant left subclavian artery. A lateral chest radiograph showing anterior displacement of the trachea suggests the presence of a vascular ring.
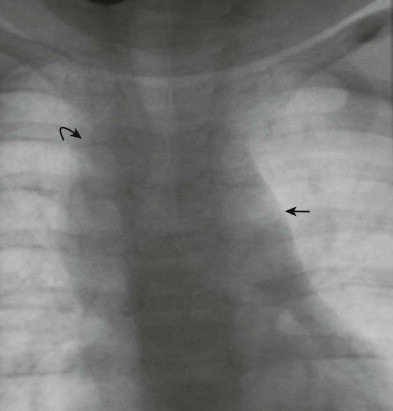
Although it is less frequently performed than in the past, barium esophagography often remains the initial imaging study in patients with symptomatic vascular rings. Therefore, radiologists must be able to recognize the characteristic impression that each type of ring produces on the upper esophagus, especially on the lateral view ( Figs. 115-9 and 115-10 ).
Even after a vascular ring has been detected by plain radiography or esophagography, advanced cross-sectional imaging is recommended for more detailed evaluation. Magnetic resonance (MR) angiography with and without intravenous administration of contrast material and contrast-enhanced multidetector computed tomography (CT) angiography allow production of high-resolution multiplanar reformatted images and three-dimensional reconstructions that assist in detailing the complex anatomic relationships between aortic arch structures, trachea, and esophagus ( Figs. 115-11 and 115-12 ). CT and MR angiography are particularly useful for presurgical planning and postoperative and postendovascular evaluation and have largely supplanted conventional catheter angiography for direct visualization of vascular anatomy. State-of-the-art MR angiography is usually preferred to CT angiography in pediatric patients because it does not require radiation or iodinated contrast material and can provide hemodynamic information. Multidetector CT angiography can be performed when MR angiography is not available, is contraindicated, or is likely to be nondiagnostic.
Acquired Abnormalities of the Esophagus
Gastroesophageal Reflux Disease
Clinical Findings
Gastroesophageal reflux (GER) is a common, almost physiologic process in infants and children. It usually results from the failure of the lower esophageal sphincter to maintain an adequate resting pressure, but approximately 35% of children with GER may have additional disorders of esophageal motility. GER is pathologic when it is associated with hematemesis, failure to thrive, esophageal stricture formation, apnea, and bradycardia. Additional extraesophageal or supraesophageal symptoms of GER, such as otitis media, asthma, recurrent upper respiratory tract infections, and sleep disturbances, are becoming increasingly recognized. GER is also responsible for the development of Barrett’s mucosa in the esophagus.
GER can be an isolated problem, but it occurs with increased frequency in children with neuromuscular disorders; repair of tracheoesophageal fistula, diaphragmatic hernia, or gastroschisis; cystic fibrosis; and collagen-vascular diseases. Medications given to decrease bronchial spasm and to enhance aeration in children with bronchopulmonary dysplasia and asthma may reduce lower esophageal pressure, cause or worsen GER, and conversely exacerbate respiratory symptoms. Secondary GER occurs in infants and children with gastric outlet obstruction and may disappear after the obstruction is corrected. Delayed gastric emptying coexists in 50% of children with primary GER.
Although GER can be suspected on clinical grounds (i.e., infant who vomits after every feeding), some pediatricians prefer to document and quantify the reflux before beginning therapy. Barium esophagography, the most commonly used test, is inexpensive and readily available. The greatest value of barium esophagography may be not in its ability to diagnose GER but in its ability to detect other causes of the child’s symptoms and to exclude gastric or duodenal obstruction. Radionuclide scintigraphy is much less used to diagnose GER than in the past. Esophageal manometry and pH probe monitoring of the esophagus provide additional information about the frequency and duration of reflux. Endoscopy can document the presence and severity of GER-induced esophagitis.
Most children with isolated GER outgrow the process, but those with underlying abnormalities are less likely to do so. Symptomatic GER can be treated by thickening the infant’s formula, giving smaller amounts at each meal, and positioning the infant appropriately after eating. Proton pump inhibitors and antacids are commonly given. Properistaltic agents have debatable success in treatment. Discontinuation of potentially provocative medications or correction of a gastric or duodenal obstruction may also eliminate GER.
Those failing to respond to medical regimens may undergo a fundoplication, which is a surgical augmentation of the lower esophageal sphincter with a gastric wrap around the lower esophagus. In the most common variant of the procedure, the Nissen fundoplication, the gastric fundus is wrapped 360 degrees around the esophagus; however, partial rather than complete wraps may also be performed, especially in children with poor esophageal motility. Antireflux surgery produces less morbidity and is more successful in children with isolated GER than in those with a complex medical or surgical history. Before fundoplication is performed, it is important to exclude a lesion that interferes with gastric emptying. If one is found, the antireflux surgery may be complemented by pyloroplasty or pyloromyotomy. For certain patient populations, laparoscopic fundoplication is favored to an open procedure in many centers. The success rate of laparoscopic fundoplication is equal to that of conventional fundoplication, and benefits include shorter hospital stays, decreased need for pain medication, better cosmetic result, and earlier institution of feeding.
In some children, GER is associated with torticollis and abnormal movements of the trunk, head, and neck simulating a neurologic abnormality. This is called Sandifer’s syndrome. The abnormal movements cease after the GER is corrected and may be the result of the pain caused by the GER or may represent attempts to minimize reflux.
Imaging Findings
Barium Studies.
To optimize detection of GER during barium esophagography, the esophagogastric junction should be challenged by an adequate amount of liquid in the stomach, and intermittent observation should be performed during several minutes. If the child refuses to drink the necessary volume of barium or has neurologic impairment of swallowing, it can be instilled into the stomach through a nasogastric tube. If the child has ingested almost as much barium as necessary then refuses to drink more, formula or juice may be given to supplement the volume. The dilution of barium does not change the ability to detect GER.
Fluoroscopy is used to define the frequency, volume, and cephalad extent of the GER ( Fig. 115-13 ). Aspiration rarely occurs as a result of GER but may be demonstrated during the swallowing portion of esophagography. The rate at which the refluxed barium clears from the esophagus should be evaluated; children with rapid clearing are less likely to aspirate or to develop esophagitis. GER-induced esophagitis is rarely seen on standard contrast studies. After the question of GER has been addressed, the stomach and duodenum should be observed to exclude delayed gastric emptying, gastric outlet obstruction, duodenal obstruction, or malrotation.

Nuclear Scintigraphy.
The radionuclide scan is extremely sensitive in the diagnosis of GER. The child is given formula or juice containing technetium Tc 99m sulfur colloid (or other technetium chelate) and is continuously scanned for 60 minutes, allowing documentation of the number of reflux episodes during this prolonged time. This is a major advantage over fluoroscopy, which must be intermittent to minimize radiation exposure to the child. The radionuclide study compares favorably with the “gold standard” of 24-hour pH probe study for gastroesophageal reflux disease and provides additional information about gastric emptying, aspiration into the lung, and abnormal esophageal contraction.
Ultrasound.
Ultrasound can accurately demonstrate episodes of GER and correlates well with the results of barium studies and esophageal pH monitoring, but it has failed to replace other tests in the primary diagnosis of GER. The anatomy of the gastroesophageal junction is well visualized with ultrasound, which can be used in conjunction with other studies to evaluate reflux. After feeding, GER is seen as retrograde passage of highly echogenic material toward the esophagus. Sonography has also been used to evaluate the length of the intra-abdominal portion of the esophagus, a factor that correlates with the likelihood of GER.
Postsurgical Studies.
Indications for postsurgical studies include dysphagia, which may indicate that the fundoplication is too tight, and continued GER symptoms, which suggest that the gastric wrap is too loose or has become undone. On radiographic examination, the intact wrap produces a mass effect at the gastroesophageal junction ( Fig. 115-14 ). Breakdown of the wrap may be associated with paraesophageal hernia or GER ( Fig. 115-15 ).











