Chapter Outline
Imaging of the Pediatric Pancreas
Imaging of the Pediatric Pancreas
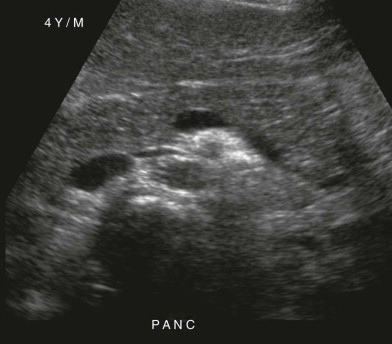
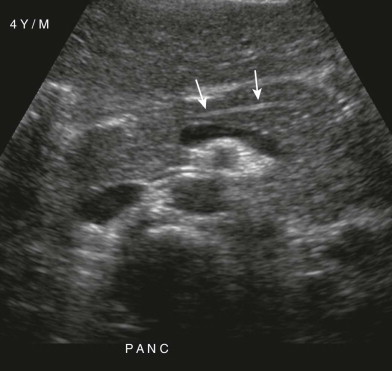
Ultrasound is the initial imaging modality of choice for evaluation of the pediatric pancreas. The relatively large left hepatic lobe serves as an acoustic window and children have a thin body habitus, which makes this possible. Ultrasound is also ideal for imaging of children because it is noninvasive and does not require sedation, along with the lack of ionizing radiation. On sonography, the normal pancreas has a homogeneous echotexture ( Fig. 121-1 ). The pancreas in preterm infants and neonates usually is more echogenic than the liver. As children grow, it usually becomes nearly isoechoic to the liver. The normal pancreatic duct is commonly seen in the body of the gland as an echogenic line or an anechoic lumen with echogenic borders ( Fig. 121-2 ). Relative to body size, the pancreas is larger in children than in adults, although it tends to shrink relatively with age. The head and tail of the pancreas typically are thicker than the body and neck. The usual prominence of the head can sometimes be mistaken for abnormality. The pancreatic duct normally is less than 2 mm in diameter.
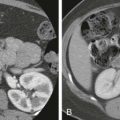
Given the ionizing radiation, the need for intravenous and oral administration of contrast material, and the possible need for sedation of young patients, computed tomography (CT) is usually reserved for when the ultrasound study is nondiagnostic. It is also used to more clearly define anatomic detail (such as pancreatic mass, severe pancreatitis, or the complete extent of disease), to evaluate blunt abdominal trauma, and to assess the distant complications of pancreatic disease. On CT, the normal pediatric pancreas has a generally smooth or slightly lobulated surface and a homogeneous soft tissue attenuation that is usually similar to that of the liver ( Fig. 121-3 ).

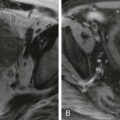
Magnetic resonance imaging (MRI), when it is coupled with magnetic resonance cholangiopancreatography (MRCP), is a powerful, noninvasive tool for imaging of the pancreatic and biliary ductal systems. On fat-saturated T1-weighted images, the pancreas demonstrates intrinsic T1 hyperintensity and is of bright signal compared with other organs. On T2-weighted images, the pancreas should be isointense to the liver. MRCP is useful to evaluate the ductal anatomy in children with acute or recurrent pancreatitis for congenital abnormalities, such as pancreas divisum or an abnormal pancreatobiliary junction. The disadvantages of MRI include its expense, technical difficulty (particularly in younger children, who are unable to cooperate), and poor spatial resolution with regard to peripheral pancreatic and biliary anatomy.
Whereas endoscopic retrograde cholangiopancreatography (ERCP) has been the “gold standard” for evaluating the pancreatic and biliary ductal systems, its utility has decreased with the advent of MRCP. This technique has the disadvantages of being invasive, requiring general anesthesia in children, and having the potential complication of pancreatitis, which occurs in at least 3% of children. Thus, ERCP is now usually reserved for cases that require intervention or for manometry of biliary and pancreatic sphincters.
Trauma
Blunt abdominal trauma accounts for most abdominal injuries in children. Children are more prone to trauma-induced pancreatic injury than adults are because of underdeveloped abdominal musculature. The mechanism of injury most commonly involves compression of the pancreas against the spine, as seen in motor vehicle collisions or nonaccidental trauma, or discrete focal trauma, commonly seen in bicycle handlebar injuries. There is overall approximately 3% to 12% incidence of pancreatic injury in children, with 90% of these patients also concurrently having injuries to other structures, including the liver, spleen, bowel, and adjacent vasculature. The bicycle handlebar type is the most likely to cause isolated injury to the pancreas ( Fig. 121-4 ).

The signs and symptoms of pancreatic injury may be delayed for hours or days after the trauma, particularly if the injury is isolated to the pancreas. Symptoms are often atypical and nonspecific, including abdominal pain, nausea, vomiting, and fever. The initial serum amylase level has a low sensitivity and specificity for detecting pancreatic injury, and it may be normal, even in the setting of significant pancreatic injury.
The utility of ultrasound is limited in the setting of blunt abdominal trauma, with a sensitivity of only 67% for detecting pancreatic injury seen by CT. Contrast-enhanced CT is superior to ultrasound for evaluating pancreatic trauma, with a sensitivity for detecting all pancreatic injuries of 85% within 24 hours of admission. Admission CT findings may be normal in patients later proved to have pancreatic injury by repeated imaging or laparotomy. Early findings of pancreatic injury can be subtle, especially immediately after trauma. Unlike other traumatized abdominal solid organs, the pancreas can have little change in attenuation with lacerations and fractures, making diagnosis difficult, particularly if there is no separation of the parenchymal fragments ( Fig. 121-5 ).

Pancreatic contusions or lacerations tend to occur at the junction of the body and tail of the pancreas. They are manifested as linear areas of low attenuation perpendicular to the long axis of the pancreas ( Fig. 121-6 ), and there may be associated pancreatic edema and enlargement, pancreatic or duodenal hematoma, and pancreatic duct dilation. Peripancreatic fluid or fluid in the lesser sac is a useful marker for pancreatic injury, particularly in the absence of injury to other organs. The failure to visualize a portion of the gland should suggest the diagnosis of pancreatic laceration. Complete pancreatic transection is rare ( Fig. 121-7 ). Blunt trauma is the most common cause of acute pancreatitis in children. In the setting of post-traumatic acute pancreatitis in children, CT imaging can demonstrate the typical findings of acute pancreatitis. Pancreatic pseudocysts develop in approximately 40% of children with traumatic pancreatic injury, and approximately half of these resolve spontaneously.


ERCP, where it is available, can be used to assess for ductal injury if CT findings are equivocal. ERCP has the added benefit of potential intervention as well, with placement of a stent to treat pancreatic duct injury. The routine use of ERCP can also lead to more cases of pancreatic injury being treating nonoperatively.
Once pancreatic injury is diagnosed, management depends on the severity and location of the injury and on the presence of associated intra-abdominal injuries. Most patients are treated nonoperatively with bowel rest and total parenteral nutrition. The decision to intervene surgically is based on hemodynamic instability and the degree of spill of pancreatic fluid into the intraperitoneal or retroperitoneal space. Injury to the proximal pancreatic duct usually is treated conservatively with bowel rest, nasogastric decompression, and hyperalimentation. Transection of the distal pancreatic duct, however, may be treated with distal pancreatectomy with preservation of the spleen.
Abnormal pancreatic enhancement can be seen in the setting of hypoperfusion complex, a rare process seen in young children with hypovolemic shock. This complex tends to occur in those who suffer severe central nervous system or abdominal injury and have evidence of profound acidemia. Imaging findings of hypoperfusion complex include “shock bowel,” with diffusely dilated, fluid-filled bowel with abnormal mural enhancement ; intense enhancement of the pancreas, kidneys, adrenal glands, and mesentery ; moderate to large intraperitoneal hematomas; and diminished caliber of the abdominal aorta and a slitlike inferior vena cava ( Fig. 121-8 ).

Pancreatitis
Acute Pancreatitis
Pancreatitis is an uncommon cause of abdominal pain in children. The clinical diagnosis of acute pancreatitis is based on the presence of upper abdominal pain and tenderness and evaluation of pancreatic enzymes. With a mortality rate for acute pancreatitis in children as high as 21% and protean clinical presentations, a high level of clinical suspicion is essential for prompt diagnosis.
The causes of acute pancreatitis in children differ significantly from those in adults. In adults, pancreatitis is associated with alcoholism and biliary tract disease in 80% of cases. The most common cause of acute pancreatitis in children is blunt abdominal trauma, followed by infection and drug use. Numerous drugs and toxins have been implicated in causing acute pancreatitis. The most commonly associated medication in children is the antiseizure drug valproic acid. Infections causing acute pancreatitis in the pediatric population tend to be viral and include the mumps virus, coxsackievirus B, and varicella-zoster virus. Fifteen percent of cases of acute pancreatitis in children are caused by structural anomalies. These include congenital anomalies (e.g., pancreas divisum), Crohn’s disease, and duodenal ulcers that involve the periampullary region. Multisystemic disease, including vasculitis, lupus, sepsis, sickle cell disease, and hemolytic uremic syndrome, accounts for approximately 14% of cases of acute pancreatitis. In cases of unexplained pancreatitis, diagnostic considerations, particularly in a young child, should include nonaccidental trauma, inborn errors of organic acid metabolism, hereditary pancreatitis, hemolytic uremic syndrome, and biliary tract disease. Other causes of pediatric pancreatitis are listed in Table 121-1 . In up to 25% of cases, no cause is found.
|
Plain radiographs are not sensitive for detection of acute pancreatitis, but some reactive findings can be seen ( Fig. 121-9 ). These include atelectasis, elevation of the hemidiaphragms, left pleural effusion, pericardial effusion, and pulmonary edema on chest radiographs. A sentinel loop in the left upper quadrant or diffuse small bowel ileus (see Fig. 121-9 ), a dilated transverse colon, or paucity of gas within the descending colon can be seen on abdominal radiographs. Additional findings may include mass effect from a pancreatic pseudocyst and peripancreatic extraluminal gas (if it is associated with an abscess).

Ultrasound is usually the first imaging study performed for the evaluation of suspected pediatric pancreatitis. Enlargement of the pancreas can be seen, either diffuse or focal, usually involving the head ( Fig. 121-10 ). However, there is a wide variation in pancreatic size in children, and there can be overlap between healthy patients and those with pancreatitis. The pancreatic echotexture can also become hypoechoic with acute pancreatitis, but increased echogenicity has also been described. The most reliable finding in children appears to be dilation of the pancreatic duct. A dilated duct with poorly defined borders can be seen in acute and chronic pancreatitis, with the duct diameter tending to be greater in patients with chronic pancreatitis. The duct diameter associated with pancreatitis is greater than 1.5 mm in children 1 to 6 years of age, greater than 1.9 mm in children 7 to 12 years of age, and greater than 2.2 mm at 13 to 18 years of age. In mild cases of pancreatitis, the pancreas can appear normal. Other findings that can be seen on ultrasound include gallstones, biliary sludge, and intrahepatic or extrahepatic biliary ductal dilation. Ascites and extrapancreatic fluid collections are frequently observed. Ultrasound is also the modality of choice for follow-up of pancreatitis fluid collections.

CT is more sensitive than ultrasound to detect early findings of pancreatitis and is best for evaluating the severity of pancreatitis and the potential for complications. CT evaluation of acute pancreatitis in pediatric patients demonstrates a spectrum of findings. These include diffuse gland enlargement with heterogeneous attenuation and enhancement; poorly defined pancreatic margins, peripancreatic fluid, and edema; and fat and soft tissue inflammation ( Fig. 121-11 ). Areas of decreased attenuation and poor contrast enhancement indicate pancreatic necrosis and increased severity of pancreatitis. A normal pancreas on initial imaging can be seen in up to one third of patients with acute pancreatitis.