Disorders of the Ankle and Foot
Medial
Tibialis Posterior Tendon
Tendinopathy of the TPT is most common in middle-aged females who complain progressively of pain followed by flat foot deformity. Classically patients describe difficulty with walking on uneven ground, climbing and descending stairs. Clinically, tenderness is found on the medial aspect of the ankle along the line of the tendon. With advancing disease, the patient is unable to carry out a single heel raise.
Flat foot deformity is assessed with the patient standing. Looking from the posterior, more toes are visible lateral to the heel on the affected side.
Tenosynovitis
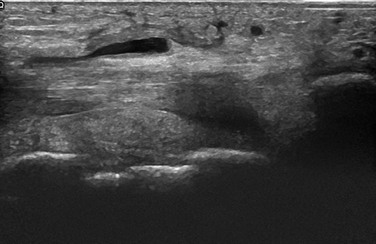
A small quantity of fluid is frequently found in the normal tendon sheath, particularly in the submalleolar region. A useful rule of thumb is that the cross-sectional area of fluid should not exceed that of the adjacent tendon. In the earliest stages, findings may be limited to excess fluid within the tendon sheath (Fig. 27.1).
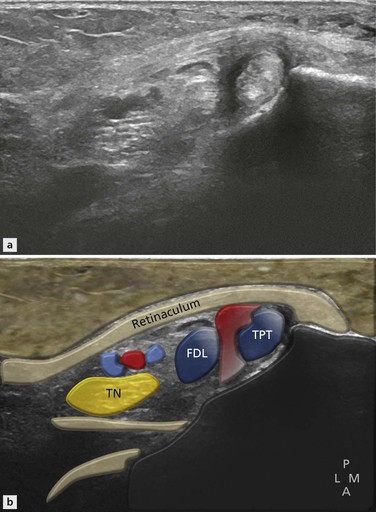
Figure 27.1 Earliest sign of tenosynovitis. A small quantity of fluid with minimally thickened synovium surrounds the tendon on the axial image.
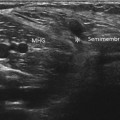
Distension often begins in the immediate submalleolar area as this is where the sheath has room to expand (Fig. 27.2).
As tenosynovitis progresses, synovial thickening as opposed to echo-free fluid becomes more apparent (Fig. 27.3) and increased Doppler signal develops within it (Fig. 27.4). Apart from the nutrient artery, Doppler signal will not under normal circumstances be found in the synovial lining and its presence is generally indicative of tenosynovitis. Synovial thickening may become quite marked, even mass-like (Fig. 27.5). Even at this stage, the tendon may remain completely normal, although in most cases some degree of underlying tendon disease is apparent, especially if high-resolution equipment is used. Detecting even small degrees of tendinopathy may have important implications in planning treatment.
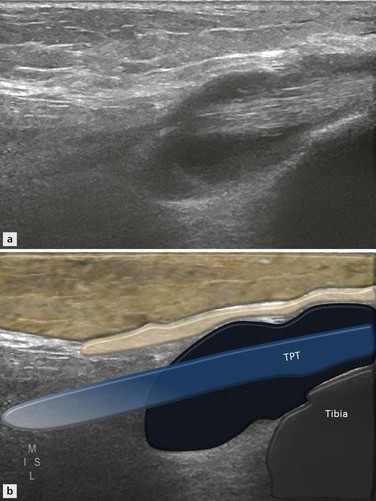
Figure 27.2 Advanced tenosynovitis. The long axis shows the fluid is predominantly submalleolar and more than the diameter of the associated tendon. This indicates an abnormal quantity of fluid.
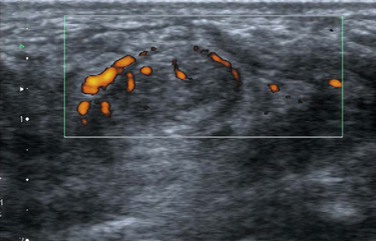
Figure 27.4 Axial image of posteromedial ankle. There is increased Doppler signal within the tendon and surrounding tendon sheath indicative of tibialis posterior tenosynovitis and tendinopathy.
Hypertrophic, Atrophic and Calcific Tendinopathy
These are due to loss of the normal tendon architecture with areas of focal hypointensity representing tendon degeneration. The tendon may begin to delaminate and longitudinal splits appear. Progression leads to enlargement of the tendon and areas of further focal breakdown and partial tear. The name hypertrophic tendinopathy or type 1 partial tear is applied to this condition. Increased Doppler activity can be detected within the tendon at an early stage.
Under normal circumstances, blood vessels should not be found within a tendon apart from perhaps an occasional vessel close to the nutrient artery.
The detection of intrinsic tendon abnormalities also has a significant impact on therapeutic decision making and many feel that corticosteroid injection therapy for tenosynovitis is contraindicated when the tendon becomes abnormal. Others argue that minor signal changes within the tendon, particularly using sensitive ultrasound, are not a contraindication to corticosteroid injection; however, in all cases the patient should be warned about the potential for tendon rupture and protected against it.
These early abnormalities predominate in the submalleolar region and may be associated with other findings. There is a fibrous pulley enthesis on the posterior aspect of the medial malleolus where the TPT passes around it. Involvement of the enthesis may lead to bony hypertrophy and the formation of a spur on the posterior aspect of the medial malleolus (Fig. 27.6). This may be visible on plain films and is a useful plain film clue to the underlying tendon disorder. It is also clearly visible on MR imaging, particularly in the axial plane.
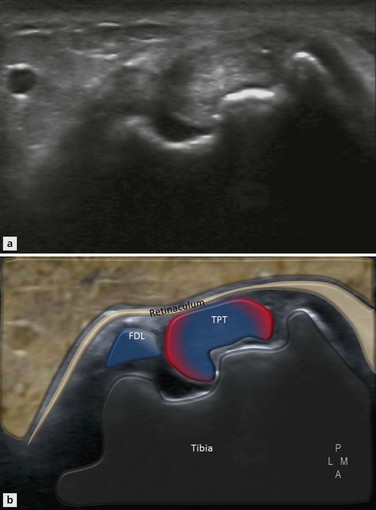
Figure 27.6 Axial image of posteromedial ankle. There is marked bony irregularity of the posterior margin of the medial malleolus with a posteromedial bony spur. Chronic enthesopathy may occur in association with TPT disease.
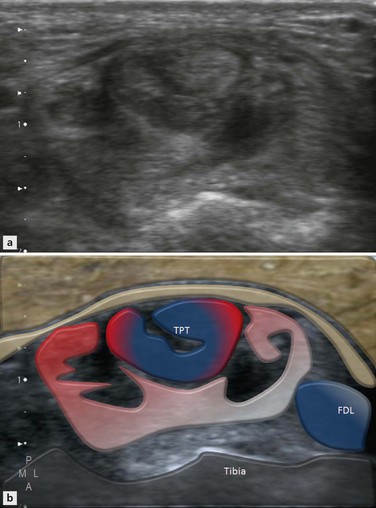
As the tendon begins to further elongate and as the arch of the foot drops, the tendon becomes further stretched. In some cases, there is a decrease in the cross-sectional area of the tendon that now appears of equal size to or smaller than the adjacent flexor digitorum tendon. The appearance of atrophic tendinopathy, as it is called (Fig. 27.7), has been likened to a fraying rope. As the individual strands begin to dissociate, they slide apart, reducing the tendon cross-sectional area in the most involved segment (Fig. 27.8). As has previously been outlined …
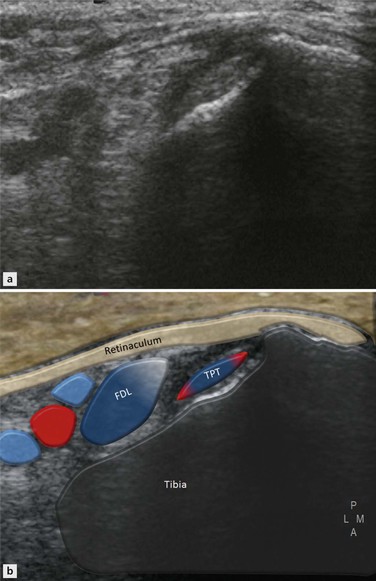
Figure 27.7 Axial image of posteromedial ankle. There is marked reduction in the diameter of the TPT, indicative of a type 2 tear. This is less common than the hypertrophic-type 1 tear.
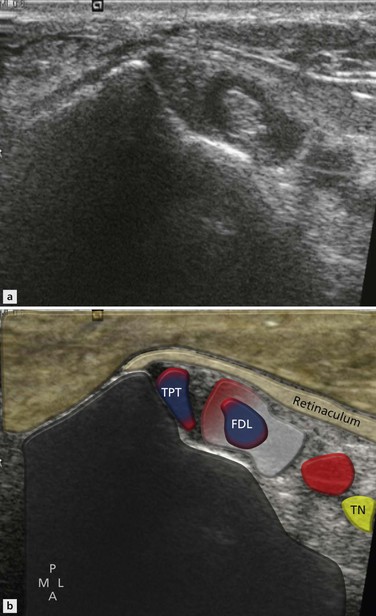
Figure 27.8 Axial image of posteromedial ankle. There is marked loss of reflectivity, particularly in tibialis posterior, which is decreased in size compared with flexor digitorum. This indicates a type 2 atrophic tear. The abnormality extends into the tendon sheath of flexor digitorum, which can be a shared sheath with TPT.
In general this is a relatively straightforward diagnosis with ultrasound as the tendon sheath is frequently involved and the internal structure of the tendon is grossly abnormal. On MRI, however, the abnormalities of the tendon sheath may be less obvious and the degenerating tendon may preserve its low signal on both T1 and T2 weighting. An alteration in size is therefore often the only feature of type 2 partial tear and the diagnosis may be overlooked.
Other forms of tendinopathy include acute calcific (Fig. 27.9) and insertional tendinopathy. Fibrosing tenosynovitis is uncommon in the TPT, although it has been described. Calcification in the tendon sheath leading to acute calcific tenosynovitis is rare. A few flecks of calcification within the tendon, particularly at tendon insertions, should not be regarded as significant and calcification of this type is frequently asymptomatic. As with the supraspinatus tendon, occasionally acute calcific tendinopathy presents very acutely. The skin is red, the subcutaneous tissues are swollen and the tendon is very tender to touch. Calcium may be seen as a conglomerate within the tendon that can be associated with an increase in Doppler signal.
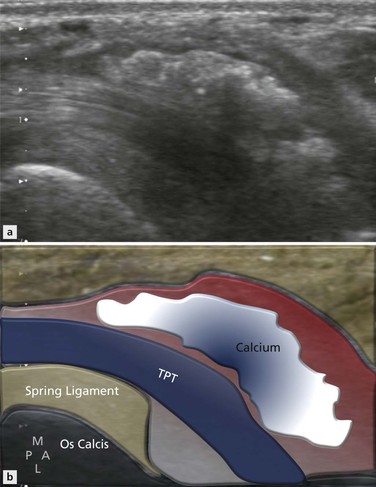
Figure 27.9 Axial image of medial ankle close to TPT insertion. There is enlargement of the tendon sheath that is filled with reflective material representing milk of calcium.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree