Disorders of the Fingers and Hand
Flexor Tendons
Anatomy and Clinical Aspects
The profundus tendon continues distally to insert on the volar aspect of the distal phalanx. The two tendons are contained within a common sheath. Vascular supply is from the adjacent digital arteries, with the vascular pedicle, or vincula, invaginating the tenosynovium as the tendovaginum.
Disorders of the tendon and tendon sheath, as with tendons elsewhere, include tenosynovitis, tendinosis and tendon rupture. Tenosynovitis refers to inflammation on the tendon sheath. The term tendinosis is sometimes used for intratendinous mucinous degeneration, which is not associated with symptoms. Tendinopathy is a similar term, but in the same context indicates that symptoms are present. Others use the term tendinosis regardless of whether symptoms are present or not.
Tenosynovitis
Patients with tenosynovitis may initially complain of stiffness and inability to form a fist and not infrequently arthritis is suspected.
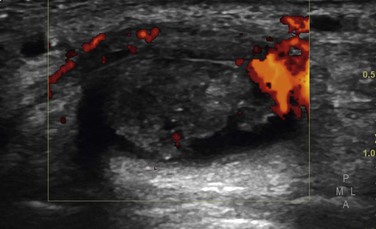
Inflammatory changes within the tendon manifest as increased fluid and, with progress of the disease, thickening of the synovial lining and increased Doppler signal.
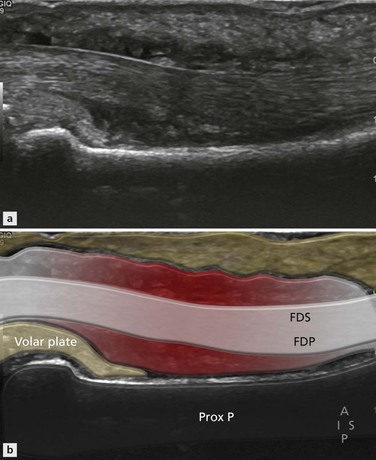
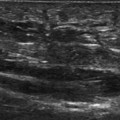
This is due to a thin rim of fluid that comes between the tendon and tendon sheath (Fig. 15.1). This sign is best appreciated on axial images, especially by comparing the affected finger with those that are not involved.
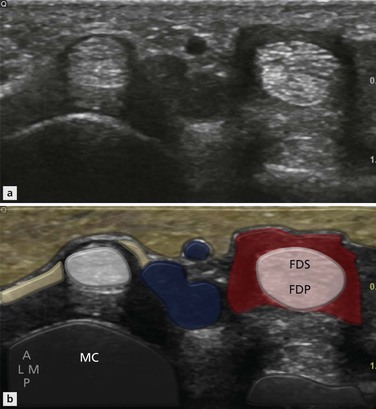
Figure 15.1 Transverse section of flexor tenosynovitis of third finger. Note a thickened low-reflective halo around the otherwise normal tendon. Compare with the adjacent flexor tendon.
As the amount of fluid increases, the tendon sheath becomes increasingly distended (Fig. 15.2). In long axis fluid and synovial thickening will not be evenly distributed along the length of the tendon (Fig. 15.3), but will be initially constrained in the areas of the flexor pulleys, creating a lobulated appearance. This should not be misinterpreted as multiple ganglia. As the disease progresses, the degree of synovial thickening (Fig. 15.4) and Doppler activity increases (Fig. 15.5). At this stage associated tendinopathy is common and vascular ingrowth is identified within the substance of the tendon itself, alongside accompanying intratendinous matrix changes.
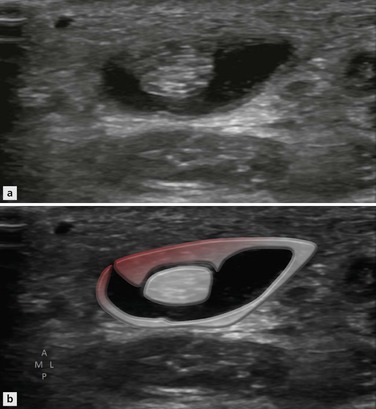
Figure 15.2 Flexor tenosynovitis. Fluid surrounds the tendon apart from where the tenovaginum attaches. Note the slight thickening of the synovial lining of the tendon sheath.
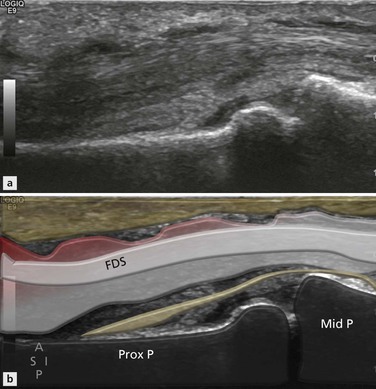
Figure 15.3 Long axis of flexor tenosynovitis. Note the rind of low-signal material around the tendon. It has an undulating appearance where the sheath is constrained by the flexor pulleys.
Tendon Rupture
This injury is referred to as a jersey finger or rugby finger, reflecting a common cause of injury. The profundus tendon of the ring finger is the most commonly affected by the jersey pull injury. The injured player attempts to grab his opponent by the jersey but only manages to gain purchase with the tip of the finger, which is then forcibly extended. The insertion of the profundus tendon is avulsed from the underlying bone with a small bony fragment attached, or a small stump of tendon remains attached to the distal phalanx (zone 1 injury) and the remainder of the tendon retracts proximally (Fig. 15.6). The index finger is involved in 75%.
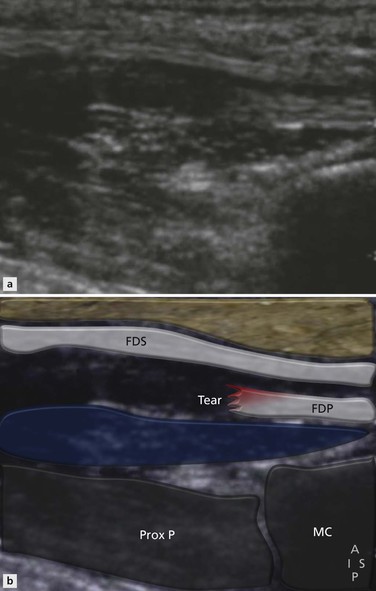
Figure 15.6 Flexor tendons at the level of the palm. The superficial flexor tendon is intact. There is a tear of the profundus tendon that is retracted.
The flexor tendons are less strongly attached to the surrounding structures and thus the degree of retraction is often quite large.
Flexor Pulleys
Anatomy
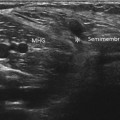
The flexor tendons of the hand are held in place by a series of connective tissue retinacula that are formed by condensations of the fibrous sheath. They are arranged into annular and cruciate configuration, referred to as the A and C pulleys (Fig. 15.7). The pulley system is important for keeping the flexor tendons close to the phalanges to maximize their ability to flex the fingers. Clinically, the annular A pulleys are by far the most important and these are numbered A1–5. The A1, A3 and A5 are at the level of the metacarpalphalangeal, PIP and DIP joints respectively. They are on the convexities of the flexor tendons and are thus less prone to injury. The A2 pulley is at the level of the midportion of the proximal phalanx and the A4 pulley at the midportion of the middle phalanx (Fig. 15.8). These are on the concavity of the flexor tendon and are more prone to injury.
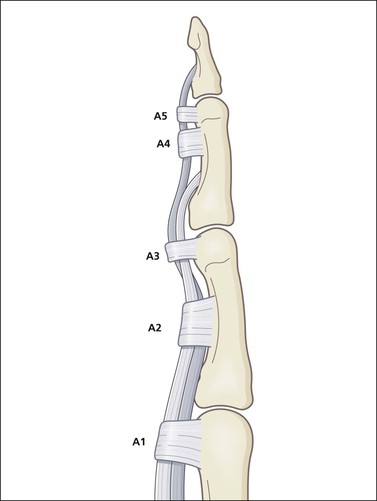
Figure 15.7 Schematic diagram of the annular pulleys. Five sets are present. A1, A3 and A5 are at the level of the articulations on the convexity of the tendon. A2 and A4 are on the tendon concavities and are the most prone to injury.
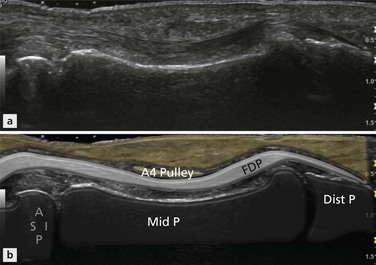
Figure 15.8 The normal A4 pulley is a low-signal, thin structure surrounded by a rim of more reflective connective tissue. The A2 and A4 pulleys overlie the tendon at its most concave portion.
Pulley Injury
The classic injury leading to pulley rupture is typified by the crimp grip of rock climbers. Hyperextension occurs at the metacarpalphalangeal joint and flexion at the IPJ. If the weight supported by the fingers in this position is suddenly increased beyond the restraining ability of the pulley system, rupture occurs. The flexor tendons are pulled away from the phalanges and shorten. This is called bowstringing. The middle and ring fingers are the most vulnerable. There is some disagreement as to which pulley ruptures first, although most commonly the injury is said to begin at the distal portion of the A2 pulley. It then progresses through A4 with progressive bowstringing of the flexor tendon (Fig. 15.9).
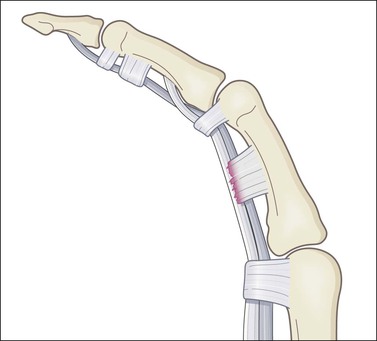
Figure 15.9 With increasing strain, the A2 pulley ruptures. The flexor tendon separates from the proximal phalanx with bowstringing.
A small gap (<3 mm) suggests isolated A2 injury and gaps more than 5 mm suggest multiple pulley involvement. The A1 pulley is rarely involved in this injury. Injuries to the cribriform or C pulleys are reported, but not common.
Ultrasound Imaging of Pulley Rupture
Injury to the pulley itself may be visualized by both ultrasound and MRI (Fig. 15.10). Ultrasound offers an advantage over MRI in that the pulley can be stressed dynamically. The patient places the back of their hand on the examination couch and the probe is placed in long axis overlying the A2 pulley. A free finger of the examiner’s hand is placed on the distal phalanx of the finger being examined, restraining it as the patient flexes (Fig. 15.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree