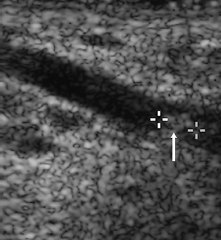
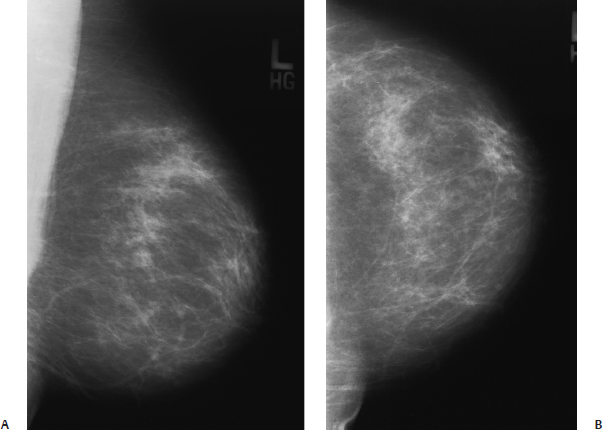
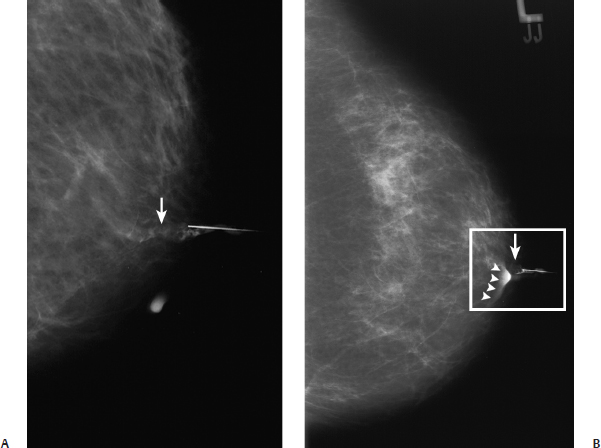
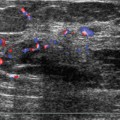
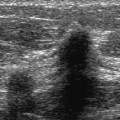
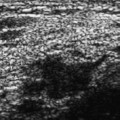
33 Ductal Abnormalities A 46-year-old woman presents with right nipple discharge. • Right breast: clear discharge expressed from nipple • Left breast: normal exam, no discharge Fig. 33.1 Normal heterogeneously dense right breast. (A) Right MLO mammogram. (B) Right CC mammogram. Frequency • 13 MHz Mass (Figs. 33.2 and 33.3) • Echogenicity: hypoechoic • Retrotumoral acoustic appearance: no shadowing • Shape: ellipsoid Fig. 33.2 Right radial breast sonogram. At the 6 o’clock position of the nipple, there is a dilated duct. Within the duct is a small, solid, hypoechoic mass (arrow). Fig. 33.3 Right radial breast sonogram. Sonography was used intraoperatively to identify the dilated duct demonstrated in Fig.33.2. The surgeon inserted a wire into the nipple. With real-time sonography, the wire (arrowheads) was demonstrated within the abnormal duct touching the intraductal mass (arrow). • Benign papilloma • BI-RADS assessment category 4, suspicious; biopsy should be considered. • Although ductography is the usual method to evaluate ducts, high-frequency sonography may be used to systematically evaluate ducts around the nipple. The operator places one end of the transducer at the nipple and rotates the transducer around the nipple. The ducts are demonstrated in a radial orientation, so they appear as linear anechoic fluid collections. In patients with abnormal nipple discharge, sonographic findings that suggest a focal etiology of the discharge include one or a few dilated ducts within the same quadrant, an intraductal or intracystic solid mass, or a solid mass near the nipple not associated with fluid. If no ducts or masses are identified or if all the ducts are dilated, then ductography is necessary to further evaluate the ducts. Sardanelli F, Imperiale A, Zandrino F, et al. Breast intraductal masses: US-guided fine-needle aspiration after galactography. Radiology 1997;204:143–148 A 71-year-old woman presents with left bloody nipple discharge. • Left breast: small clear, yellow discharge from a duct at the 3 o’clock position; no bloody discharge observed • Right breast: normal exam Fig. 33.4 Normal left breast mammogram. (A) Left MLO mammogram. (B) Left CC mammogram. Fig. 33.5 Left ductogram. Contrast is obstructed by a lobulated intraluminal mass (arrow). Because the mass obstructs the duct, contrast flows retrograde and spills outside the nipple (arrowheads). (A) Left MLO ductogram. (B) Left CC ductogram. • Benign papilloma • BI-RADS assessment category 4, suspicious; biopsy should be considered. • About 50% of women with spontaneous discharge have papillomas.
Case 33.1: Intraductal Papilloma
Case History
Physical Examination
Mammogram (Fig. 33.1)
Ultrasound
Pathology
Management
Pearls and Pitfalls
Suggested Reading
Case 33.2: Intraductal Papilloma
Case History
Physical Examination
Mammogram (Figs. 33.4 and 33.5)
Pathology
Management
Pearls and Pitfalls
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine