I
Dural sinus (or meningeal vein)
II
Sinus drainage with reflux into cerebral veins
III
Cortical veins only
IV
Supra- or infratentorial venous lake
Cognard (1995)
I | Antegrade drainage via a dural sinus |
IIa | Retrograde drainage into sinus only |
IIb | Retrograde venous drainage into cortical veins only |
IIa + b | Retrograde drainage into sinus and cortical veins |
III | Direct drainage into cortical vein, no ectasia |
IV | Direct drainage into cortical vein, plus ectasia |
V | Direct drainage into spinal perimedullary veins |
Borden (1995)
I | Antegrade dural sinus/meningeal vein flow (benign) |
II | Antegrade dural sinus flow but retrograde cortical vein drainage (aggressive) |
III | Direct retrograde cortical vein drainage (aggressive) |
Lasjaunias (2008)
Natural History
Spontaneous resolution.
Transformation to a different grade 2 %.
Increased inflow.
Venous outflow restriction by stenosis or thrombosis.
Estimated annualized risks of aggressive lesions.
Annual mortality in 10 %.
Hemorrhage in 8 %.
Nonhemorrhagic neurological deficit in 7 %.
Difference in annualized bleeding rate depending on hemorrhagic or nonhemorrhagic presentation.
Presence of “high-risk” angiographic features may be less significant in asymptomatic patients.
Annualized hemorrhage rate for CVR in patients without hemorrhage or nonhemorrhagic neurological deficit in 1.5 %.
Factors Associated with an Aggressive Clinical Course
Cortical venous drainage
Venous varicosities
Venous stenosis
Galenic drainage
Location
Previous intracerebral hemorrhage (ICH)
Factors Associated with DAVF Regression
Reducing inflow (manual compression)
Thrombosis of venous outflow
Recanalization of venous outflow
Hemorrhage
Trauma (Natural history of lesions may differ)
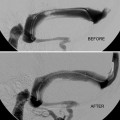
Angiography
Factors Associated with DAVF Progression
Stenosis or thrombosis of venous outflow
Increased arterial inflow
Recruitment of new AV shunts
Ineffective treatment
Treatment Options
Conservative
Curative
Partial treatment
Conservative Management
Natural history risk < treatment risk.
Patients with “low risk” transverse/sigmoid sinus DAVF have a low annual hemorrhage risk and are encouraged to live with their symptoms if tolerable. Patients with indirect CCF, orbital drainage, and normal ocular pressures may also be managed conservatively, particularly if other comorbidities (diabetes or ischemic heart disease) alter their operative risks.
Spontaneous resolution of DAVF is uncommon but well recognized.
Measures that may improve prospect of spontaneous resolution:
Intermittent manual compression of supplying artery
Avoiding aspirin and other antiplatelet/anticoagulant agents
Interventional Neuroradiology
Biplane angiographic facilities.
Trans-arterial or transvenous approach or both, either as a single modality treatment or in combination with other treatments.
Trans-arterial approach:
Proximal arterial occlusion is unlikely to be effective due to the rich collateral dural arterial blood supply.
Use of liquid embolic agents in arterial territories that supply the dura is associated with the risk of cranial nerve injury and stroke (ECA/ICA and ECA/VA collaterals).
Onyx
This liquid agent spreads through compartments of the DAVF and precipitates as the solvent diffuses out of the liquid.
Distal access close to the fistula point.
Microcatheter tip positioned in straight arterial segment (visualize reflux).
Slow injection to establish Onyx plug.
Intermittent injection to control direction of flow.
Gradually fill supplying arteries, diseased sinus compartment, and proximal draining vein.
Possible to reflux Onyx into other supplying arterial pedicles from a single injection.
Check imaging to confirm progressive cast and exclude dangerous reflux.
Possible to achieve cure in a single session.
Specific Risks
Cranial nerve injury or stroke
Catheter retention due to excessive proximal reflux (detachable tip catheter)
Radiation injury from prolonged screening times
DMSO toxicity
NBCA
Requires significant user experience, meticulous preparation, and precise technique (microcatheter wedged or not)
Potential uses dependent on user experience
High flow AV shunts (+/− coils to slow the flow)
Adjunctive treatment option
Challenging material to use
Relatively short time to polymerization
Fragmentation of glue bolus by parallel arterial inflows
Distal glue migration (outflow occlusion)
Uncontrolled proximal reflux (particularly when wedged in small access vessels)
Catheter adhesion/retention
May require multiple procedures
Declining clinical experience since the introduction of Onyx
PVA Particles
Unlikely to be curative when used in isolation
Adjunctive option to transiently reduce arterial inflow in combination with surgery or radiosurgery
Palliative option for symptom control
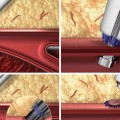
Transvenous Approach
A transvenous approach may be used to:
Sacrifice the involved section of dural sinus
Occlude the involved venous compartment adjacent to or within a dural sinus
Disconnect a “high-risk” venous drainage pathway and downgrade the shunt (possibly without occluding it)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree