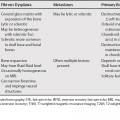
38 Many pathologic entities can effect the ear and temporal bone, with the most common etiologies being inflammatory. Imaging can help differentiate between the various entities and help to determine the presence of residual/recurrent disease in the postoperative setting. One of the more common diagnostic imaging dilemmas, differentiating cholesteatoma from inflammatory tissue, particularly in the postoperative ear, will be addressed in detail here. Skull base lesions and jugular foramen lesions that can affect this region are addressed in Chapters 7, 25, and 26. Inflammatory processes, namely otitis media, either acute or chronic, most often affect the middle ear. The imaging characteristics of acute otitis media (AOM) include opacification of the middle ear and mastoids (otomastoiditis) without bony destruction. Complications of AOM included coalescent mastoiditis, subperiosteal, epidural or subdural abscess/empyema, petrous apicitis, dural sinus thrombosis, or associated soft tissue (Bezold’s) abscess. Chronic otomastoiditis (CO) may present with a variety of manifestations including effusion, granulation tissue, or cholesteatoma. A common diagnostic dilemma is to differentiate cholesteatoma from chronic inflammatory tissue (Table 38.1). Cholesteatomas are associated with bony erosion, most commonly of the scutum or ossicular chain, where the long process of the incus is most often affected. They may also erode intracranially. However, on postoperative studies, the finding of bony erosion is no longer reliable. On magnetic resonance imaging (MRI), they are moderately hyperintense to brain on T2-weighted magnetic resonance [MR] images (T2WI) and isointense on T1-weighted magnetic resonance [MR] images (T1WI) with or without moderate peripheral enhancement.
Ear and Temporal Bone Lesions
Cholesteatoma versus Chronic Otitis Media
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree