Fig. 3.1
(a) Coronal view of the common flexor tendons. (b) Tr-trochlea, asterisk indicates joint space, orange indicates common flexor tendons, and green indicates ulnar collateral ligament
Injection Technique: In-Plane Coronal Approach
Patient positioning: The patient should be seated or lay supine with 90° of elbow flexion and the shoulder externally rotated. Place a towel underneath the lateral epicondyle for comfort.
Probe position: Place the probe longitudinally (coronal) with the proximal end of the transducer over the medial epicondyle to visualize the common flexor tendon. Scan proximally and distally until the medial epicondyle and the proximal attachments of the CFT are clearly identified (Fig. 3.2a).
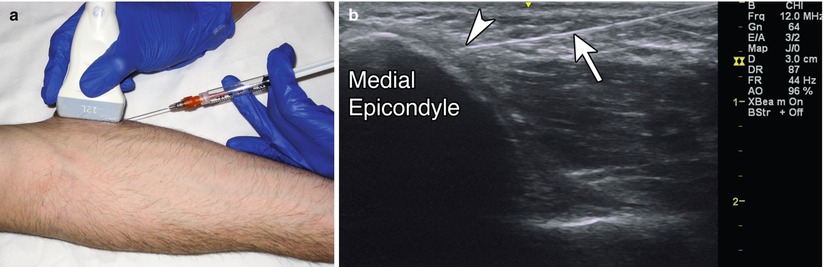
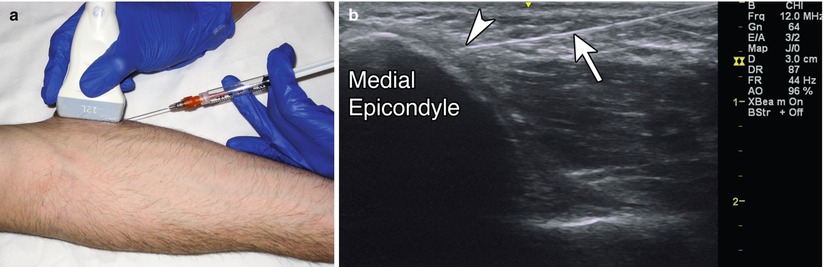
Fig. 3.2
(a) Example of probe position over medial epicondyle with in-plane injection technique. (b) Example of in-plane long-axis approach, white arrow indicates needle, arrowhead indicates needle tip, medial epicondyle labeled
Markings: Mark any obvious vessel or tendon prior to injection. Mark the medial epicondyle and the olecranon process.
Needle position: The needle should be inserted parallel to the transducer from either proximal to distal or distal to proximal. Due to the superficial nature of the tendon, a gel standoff may be helpful. For PNT, insert the needle into the tendon itself. For a peritendinous injection, keep the needle above or below the tendon.
Safety considerations: For corticosteroid injections, be careful when injecting superficial to the tendon since this can cause subcutaneous atrophy or depigmentation. PNT may cause local bleeding and post-procedure pain. Be careful to not inject too posterior, as this is where the ulnar nerve may lie.
Pearls:
If performing PNT, intermittently switch to an out-of-plane/short-axis view in order to determine the anterior-posterior/radial-ulnar position of the needle within the region of tendinosis [4]. Repetitively fenestrate the entire region of tendinosis while injecting local anesthetic, PRP, or AB. Resistance should decrease with increased passes. Calcifications and enthesophytes should be mechanically broken up [11–13].
Equipment needed:
High-frequency linear array transducer (10 MHz+).
25 gauge, 1.5″ needle.
0.5 mL of steroid preparation.
1–3 mL of local anesthetic.
For PNT, use a larger (18–20 gauge) needle.
Ulnar Collateral Ligament (UCL)
Ultrasound is very useful for distinguishing UCL pathology, including partial or complete tears, avulsion fractures, and chronic UCL injury and thickening. The UCL is a short and broad-based ligament divided into three components: an anterior, posterior, and transverse segment [5]. The anterior bundle provides the primary stabilization of the medial elbow, playing a critical role during valgus stress of the joint [10]. In injuries from sports requiring overhead throwing, prompt diagnosis is critical in determining appropriate management, whether it is surgical intervention for a complete tear versus conservative care for a partial tear or sprain [10]. For a professional athlete, delayed diagnosis of a torn ligament that ultimately requires surgery will have a significant adverse impact and may lead to the abrupt end of a professional sports career.
Clinically, a patient will present with medial elbow pain, tenderness to palpation along the ligament, and increased laxity with valgus stress at 30–90° [6]. Treatment with corticosteroid injection or PRP shows variable to promising improvement [5, 11]. In acute UCL injury, avoid using steroids for symptomatic relief, as there is an increased risk of ligamentous laxity and potential rupture [7]. In these cases, lidocaine injection may be used for temporary pain relief. After a corticosteroid injection, the patient should undergo a rehabilitation program focusing on proximal muscle strength, trunk rotation, core and gluteal strength, and the entire kinetic chain. A formal physical therapy program may be helpful [12].
Scanning Technique and Anatomy to Identify
The UCL is best visualized with the elbow positioned at 30° of flexion and the forearm supinated [4, 6]. Sprains include stretch injury with continuity of the ligament (Grade 1), partial tears (Grade 2), or complete rupture (Grade 3). With grade 1 sprains, the UCL may appear mildly thickened and hypoechoic [2]. Partial tears of the UCL appear as abnormal ligament thickening with internal hypoechoic disruption; the presence of hypoechoic fluid is variable [2, 9]. Complete tears or full thickness rupture appear as focal discontinuity of the ligament with surrounding hypoechoic edema or inability to visualize the ligament at all [13]. Increased gapping with valgus stress implies partial or full thickness tear. The anterior bundle extends from the anterior-inferior aspect of the medial epicondyle to the medial edge of the coronoid process [2, 3]. UCL avulsion, more commonly seen in the adolescent population, appears as a hyperechoic bony fragment adjacent to the medial epicondyle [2]. Chronic UCL injury from repetitive microtrauma causes progressive thickening, hypoechoic foci and calcifications that can lead to ligamentous instability (Fig. 3.3) [2, 5].
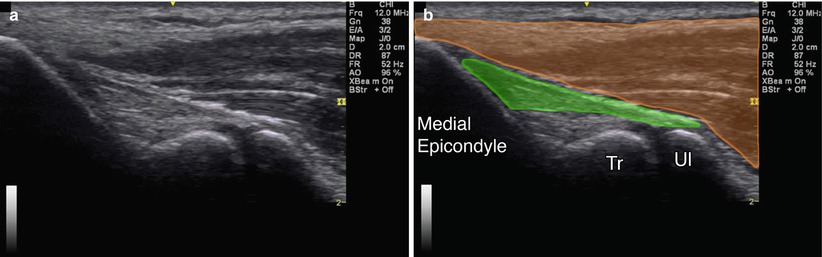
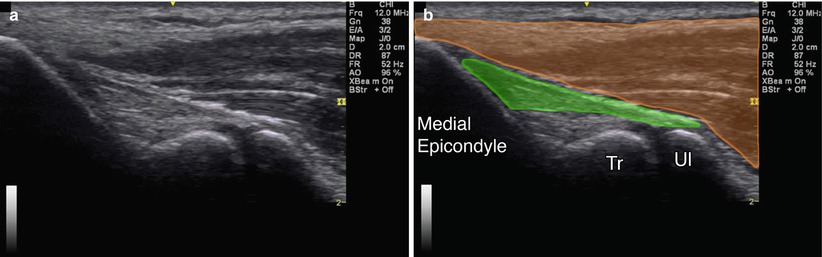
Fig. 3.3
(a) Coronal view of ulnar collateral ligament. (b) Green indicates ulnar collateral ligament, orange indicates common flexor tendons, Tr trochlea, Ul ulna, medial epicondyle labeled
Injection Technique: In-Plane Coronal Approach
Patient positioning: The patient should be seated or lay supine with 30° of elbow flexion and the shoulder externally rotated. Place a towel underneath the lateral epicondyle for comfort.
Probe position: Place the probe longitudinally (coronal) with the proximal end of the transducer over the medial epicondyle to visualize the CFT. Scan proximally and distally until the medial epicondyle and the proximal attachments of the CFT are clearly identified. The UCL appears deep to the CFT (Fig. 3.4a). A normal UCL appears compact, fibrillar, and hyperechoic compared to an abnormal UCL, which appears as a thin hypoechoic band [3].
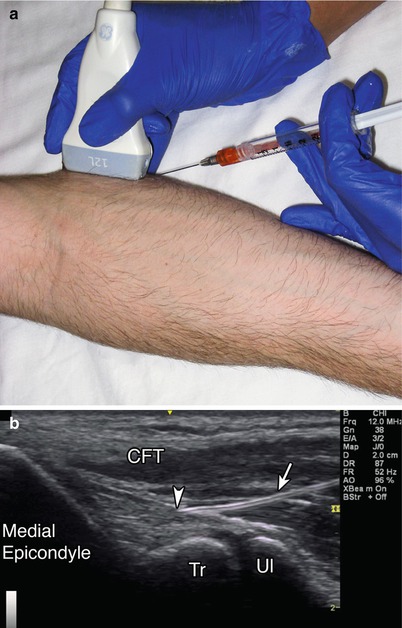
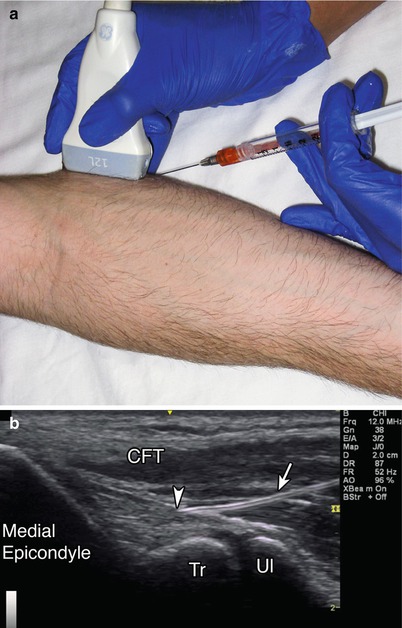
Fig. 3.4
(a) Example of probe position over ulnar collateral ligament. (b) Example of in-plane long-axis approach, white arrow indicates needle, arrowhead indicates needle tip, Tr trochlea, Ul ulnar, CFT-common flexor tendon, medial epicondyle labeled
Markings: Mark the length of the anterior band of the UCL to plan the needle approach.
Needle position: The needle should be inserted in-plane to the transducer. Inject into the hypoechoic region of the pathologic ligament with a single injection directed from distal to proximal [5].
Safety considerations: There is a risk of fatty atrophy and local depigmentation with corticosteroid injection. Be careful to not inject too posterior, where the ulnar nerve may lie.
Pearls:
Valgus stress on the elbow will help to identify laxity of the UCL.
An abnormal UCL appears hypoechoic with discontinuous fibers.
Ulnar Nerve at the Elbow
The ability of ultrasound to evaluate structures dynamically is particularly useful when evaluating the ulnar nerve at the elbow for ulnar subluxation or other causes of neuropathy [14]. At the level of the elbow, the ulnar nerve lies in the retroepicondylar groove and has a variable amount of slack in extension. This predisposes it to subluxation over the medial epicondyle during flexion, which can occur in roughly 20 % of individuals, although many may be asymptomatic. This movement predisposes the patient to ulnar neuritis [9]. Ulnar nerve subluxation also occurs in “snapping triceps syndrome.” This can occur when the distal medial head of the triceps muscle subluxes from a lateral direction during elbow flexion, causing displacement of the ulnar nerve from its groove over the medial epicondyle [9]. As a result, ulnar nerve compression and neuropathy can occur at the retroepicondylar groove and the edge of the flexor carpi ulnaris muscle aponeurosis.
Clinically, patients commonly present with upper extremity weakness, hand pain, and numbness in the ulnar distribution [15]. It may be difficult to determine if the ulnar nerve is involved and the level of involvement. Ultrasound guided diagnostic ulnar nerve blockade is an effective and efficient method to determine ulnar nerve involvement [16]. This method is often used prior to a peripheral nerve stimulator in cases of refractory ulnar neuropathy. In addition, regional anesthesia of the ulnar nerve using ultrasound guidance is an effective technique. This is often used to potentiate distal anesthesia in incomplete brachial plexus blocks and in postoperative anesthesia of forearm and hand procedures to help minimize the need for pain medication.
Scanning Technique and Anatomy to Identify
Begin by scanning proximal to distal in the transverse plane at the level of the medial epicondyle. Proximally, the nerve appears oval or triangular in shape with internal punctate hyperechoic areas [16]. The ulnar nerve has a characteristic honeycomb pattern in the transverse plane, which is the typical appearance of a peripheral nerve [17]. This pattern describes the arrangement of the hypoechoic nerve fascicles with the hyperechoic perineurium and endoneurium. Identify the medial epicondyle and triceps muscle. Distally, the nerve becomes thinner and difficult to differentiate from tendon. This is because the nerve contains smaller amounts of myelinated axons and thus can mimic the appearance of tendons. In the longitudinal plane, the ulnar nerve appears as a thin hyperechoic tubular structure. In an entrapment, the ulnar nerve becomes enlarged and edematous with an increase in hypoechoic appearance with loss of fascicular pattern (Fig. 3.5) [17].
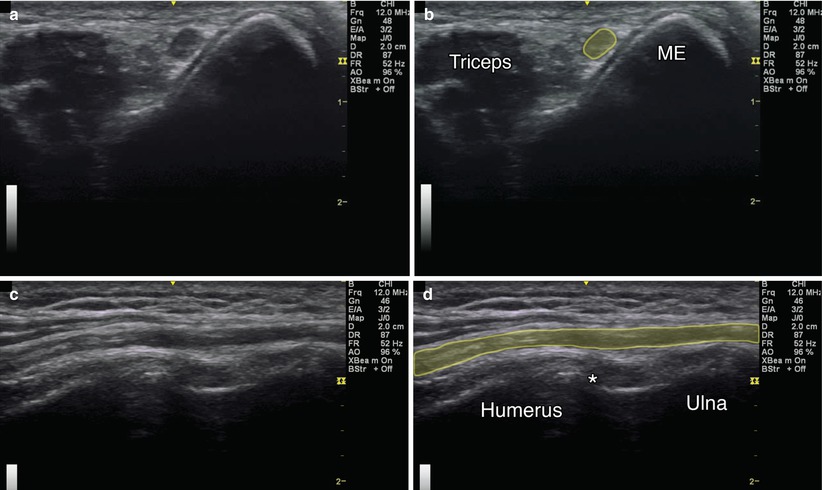
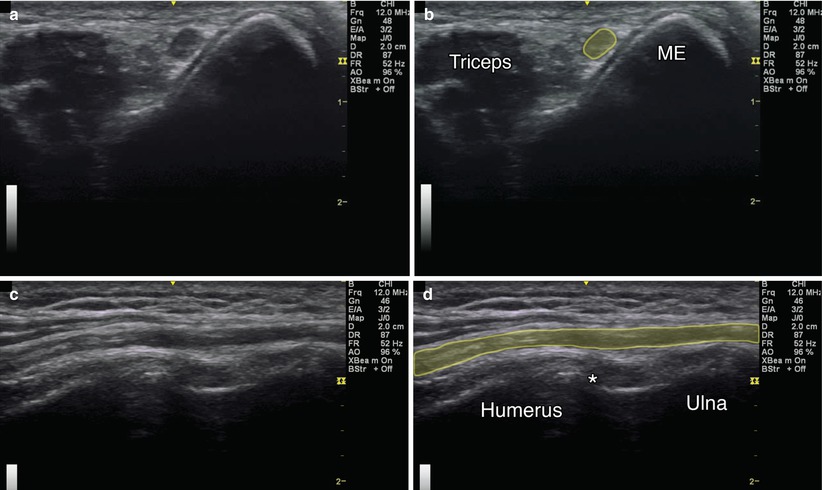
Fig. 3.5
(a) Transverse (axial) view of the ulnar nerve. (b) Yellow indicates ulnar nerve, ME medial epicondyle, triceps labeled. (c) Longitudinal view of the ulnar nerve. (d) Yellow indicates ulnar nerve, asterisk indicates joint space, humerus and ulna labeled
Injection Technique: In-Plane Axial Approach
Patient positioning: The patient should lay supine, shoulder abducted 90° and elbow flexed approximately 90°, or be seated with the elbow flexed 90° with the hand on the table [15].
Probe positioning: Place the transducer transverse relative to the ulnar nerve at the elbow (Fig. 3.6a).
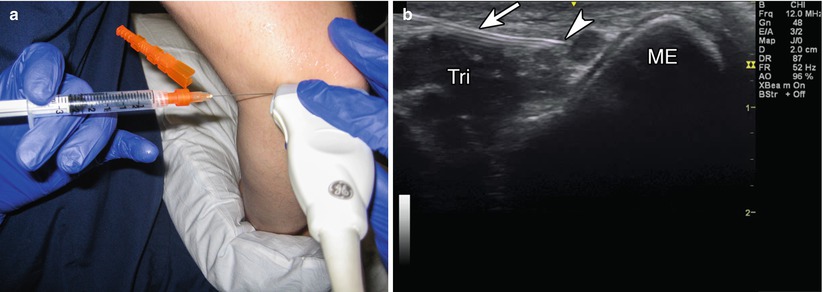
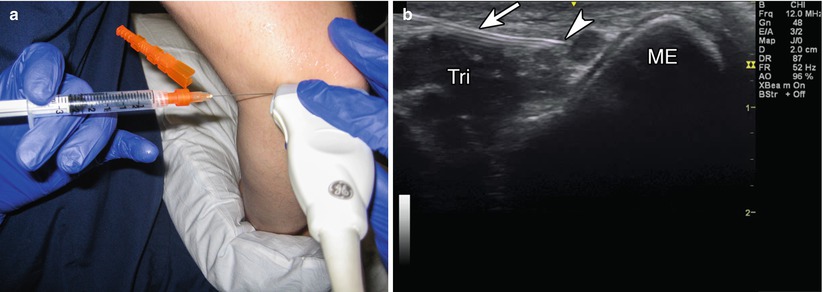
Fig. 3.6
(a) Example of probe position over ulnar nerve at the elbow. (b) Example of in-plane short-axis approach, white arrow indicates needle, arrowhead indicates needle tip, Tri triceps, ME medial epicondyle
Markings: Mark any blood vessels prior to injection.
Needle position: Start from the ulnar (medial) aspect of the transducer. An in-plane approach is advised, as this provides continuous visualization of the needle tip. Identify the ulnar nerve and then guide the needle adjacent to the nerve and inject medication to create a “target sign.” Look for spread around the circumference of the nerve and reposition as needed.
Safety considerations: Identify and avoid intravascular injection into the superior ulnar recurrent artery. Injections at this site should be limited to 3–5 mL in volume to minimize the risk of a compartment syndrome.
Pearls:
Unlike blood vessels, nerves are not compressible structures.
Injecting small amounts of anesthetic can help localize the needle tip.
Equipment needed:
High-frequency linear array transducer (10 MHz+)
25G 1.5″ needle
3–5 mL local anesthetic
Injection Technique: In-Plane Longitudinal Approach
Patient positioning: Lay the patient supine, shoulder abducted 90° and elbow flexed approximately 90°, or with the patient sitting and the elbow flexed 90° with the hand on the table [15].
Probe positioning: Place the transducer longitudinal relative to the ulnar nerve at the elbow (Fig. 3.7a).


Fig. 3.7
(a) Example of probe position over ulnar nerve at the elbow. (b) Example of in-plane longitudinal approach, white arrow indicates needle, white arrowhead indicates needle tip, black arrowheads indicate injectate over nerve sheath, asterisk indicates joint space, humerus and ulna labeled
Markings: Mark any blood vessels prior to injection.
Needle position: Start from the ulnar (medial) aspect of the transducer. An in-plane approach is advised, as this provides continuous visualization of the needle tip. Identify the ulnar nerve and then guide the needle adjacent to the nerve. Look for spread around the superficial aspect of the nerve.
Safety considerations: Identify and avoid intravascular injection into the superior ulnar recurrent artery. Injections at this site should be limited to 3–5 mL in volume to minimize the risk of a compartment syndrome.
Pearls:
Unlike blood vessels, nerves are not compressible structures.
Injecting small amounts of anesthetic can help localize the needle tip.
Equipment needed:
High-frequency linear array transducer (10 MHz+)
25G 1.5″ needle
3–5 mL local anesthetic
Lateral Epicondylosis (LE)
Lateral epicondylosis, also known as tennis elbow, is a common tendinopathy in the upper extremity. LE consists of pain at the proximal attachment of the common extensor tendon, usually arising from repetitive use and microtrauma. Patients often complain of pain in the region of the proximal wrist extensor attachments, especially with resisted wrist extension, twisting motions as the wrist, and grasping objects. Physical examination may reveal tenderness to palpation over the lateral epicondyle and reduced strength with resisted grip, supination, and wrist extension [18]. Provocative tests such as Cozen’s and Mill’s can reproduce the symptoms. Ultrasound may assist in identifying enthesophytes, tendon thickening, and calcifications [17, 18]. PNT, PRP, and corticosteroid injection into or around the involved tendon have all shown varying efficacy in treating lateral epicondylosis (Table 3.1) [19–21].
Table 3.1
Outcomes of USG percutaneous needle tenotomy in the treatment of common extensor tendinosis in the elbow, N = 52 [11]









