Elbow Anatomy
The elbow is a synovial joint composed of three elbow joint articulations: the trochlea and ulna, the capitellum and the radial head, and the proximal ulna and radius ( Fig. 4.1 ). The elbow joint has prominent joint recesses located in the coronoid and radial fossae anteriorly and within the olecranon fossa posteriorly. Within each joint recess exists an intracapsular but extrasynovial fat pad, which becomes displaced with joint distention. The medial elbow joint is stabilized by the ulnar collateral ligament, of which the anterior bundle is most important, extending from the humerus anteriorly to the sublime tubercle and several centimeters distal along the ulna ( Fig. 4.1C ). Other components of the ulnar collateral ligament include posterior and oblique bundles. Laterally, the elbow joint is stabilized by the lateral collateral ligament complex, which is composed of the radial collateral ligament, the annular ligament, and a smaller accessory radial collateral ligament ( Fig. 4.1D ). An additional component, the lateral ulnar collateral ligament, extends from the lateral epicondyle to the supinator cress of the proximal ulna; however, proximally the lateral ulnar collateral ligament is continuous with the lateral collateral ligament and typically only appears as a discrete structure extending distal from the annual ligament.
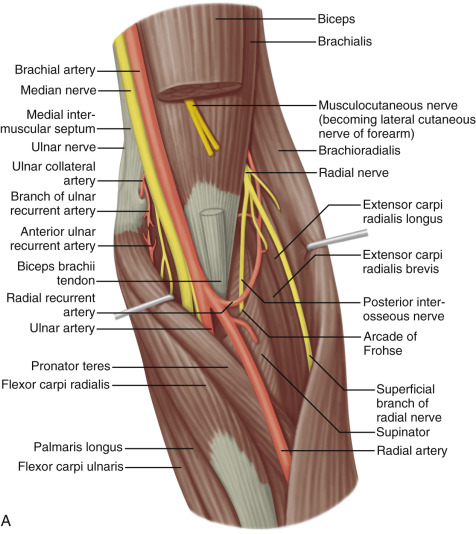
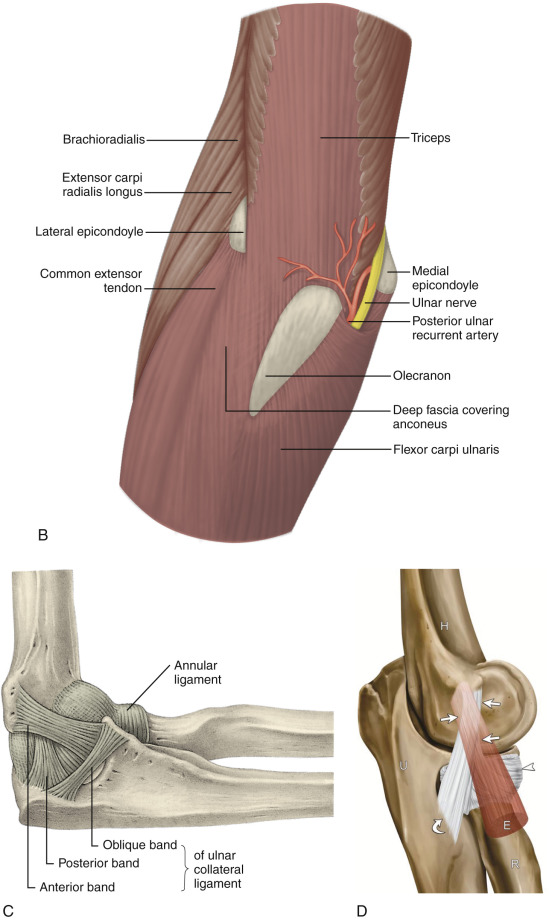
Anterior to the elbow joint, the brachialis inserts on the ulna, and the biceps brachii tendon inserts on the radial tuberosity. With regard to the biceps brachii, a dual insertion exists where the short head is superficial and inserts more distal relative to the long head on the radial tuberosity. Posteriorly, the triceps brachii inserts on the olecranon process of the proximal ulna, over which is located the olecranon bursa. The lateral and long heads of the triceps brachii represent the most superficial layer of the distal triceps, whereas the deep aspect with a relatively shorter tendon is the medial head. The anconeus is located between the olecranon process and the lateral epicondyle of the humerus. Medially, the common flexor tendon, consisting of the flexor carpi radialis, palmaris longus, flexor carpi ulnaris, and flexor digitorum superficialis, originates on the medial epicondyle of the distal humerus. Laterally, the common extensor tendon, composed of the extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris, originates at the lateral epicondyle of the distal humerus. The extensor carpi radialis brevis is the most anteriorly located of the group; the extensor carpi radialis longus originates proximal to the lateral epicondyle on the lateral humeral metaphysis.
The space between the olecranon process of the ulna and the medial epicondyle is bridged by the cubital tunnel retinaculum (or Osborne fascia) and contains the ulnar nerve. Just distal to this, the ulnar nerve enters the true cubital tunnel, between the dual origins of the flexor carpi ulnaris and deep to the arcuate ligament. The median nerve is located medial to the brachial artery and courses distally between the ulnar and humeral heads of the pronator teres. The radial nerve is located at the posterior aspect of the humeral shaft and then courses distally and laterally beneath the brachioradialis, where a deep branch courses between the two heads of the supinator muscle and a superficial branch courses beneath the brachioradialis and into the forearm.
Ultrasound Examination Technique
Table 4.1 is an elbow ultrasound examination checklist. Examples of diagnostic elbow ultrasound reports are shown in Box 4.1 and Box 4.2 .
Examination: Ultrasound of the Elbow
Date of Study: March 11, 2011
Patient Name: Kevin Saunderson
Registration Number: 8675309
History: Elbow pain, evaluate for tendon abnormality
Findings: No evidence of joint effusion or synovial process. The biceps brachii and brachialis are normal. The common flexor and extensor tendons are also normal. No significant triceps brachii abnormality. The anterior bundle of the ulnar collateral ligament and lateral collateral ligament complex are normal. The ulnar nerve, radial nerve, and median nerve at the elbow are unremarkable. No abnormality in the cubital tunnel region with dynamic imaging. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression: Unremarkable ultrasound examination of the elbow.
Examination: Ultrasound of the Elbow
Date of Study: March 11, 2011
Patient Name: Ricky Bobby
Registration Number: 8675309
History: Elbow pain, evaluate for tendon abnormality
Findings: There is a partial-thickness tear of the distal biceps brachii tendon involving the superficial short head tendon with approximately 2 cm of retraction but with intact long head. Dynamic evaluation shows continuity of the long head excluding full-thickness tear. No joint effusion. The triceps brachii, common extensor, and common flexor tendons are normal. The ulnar, radial, and median nerves are unremarkable, including dynamic evaluation of the ulnar nerve. Unremarkable ulnar and lateral collateral ligaments. No bursal distention.
Impression: Partial-thickness tear of the distal biceps brachii tendon.
General Comments
Ultrasound examination of the elbow may be completed with the patient sitting and the elbow placed on an examination table, or the patient may lie supine. A high-frequency transducer of at least 10 MHz is typically used because most of the structures are superficial. Evaluation of the elbow may be focused over the area that is clinically symptomatic or that is relevant to the patient’s history. Regardless, a complete examination of all areas should always be considered for one to become familiar with normal anatomy and normal variants and to develop quick and efficient sonographic technique.
Anterior Evaluation
The primary structures evaluated from the anterior approach are the brachialis, the biceps brachii, the median nerve, and the anterior elbow joint recess. For sonographic evaluation, the elbow is comfortably extended, and the hand is supinated. Evaluation begins with the transducer short axis to the humerus. An ideal starting position is at the level of the distal humerus where the undulating contours of the humeral articular surface covered by hypoechoic hyaline cartilage appear similar to the surface of a clam shell ( Fig. 4.2 ). The pyramid-shaped hypoechoic muscle immediately anterior to the distal humerus is the brachialis. The pulsating brachial artery is identified more superficial and medial, which is a helpful landmark in that the biceps brachii tendon is immediately lateral to the brachial artery and superficial to the brachialis. Medial to the brachial artery is the honeycomb appearance of the median nerve with the pronator teres muscle more medial. Lateral to the brachialis is the brachioradialis, and within the oblique fascia plane separating these two muscles are located the superficial and deep branches of the radial nerve, which appear hypoechoic. The lateral antebrachial cutaneous nerve is located superficial and immediately lateral to the biceps brachii tendon ( Fig. 4.2B ) as a continuation of the musculocutaneous nerve that courses between the brachialis and biceps brachii muscles more proximally ( Fig. 4.2C ).

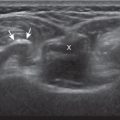
When evaluating the biceps brachii tendon in short axis, the two individual hyperechoic long and short heads may be difficult to visualize although the tendon often appears somewhat bilobed ( Fig. 4.3A ). However, toggling the transducer to create anisotropy will show the long head tendon lateral and the short head tendon medial, separated by a thin echogenic endotenon septum ( Fig. 4.3B ). When moving the transducer distally, the long head tendon will rotate and move deep to the short head tendon. The lacertus fibrosis or bicipital aponeurosis can be seen extending from the biceps brachii tendon to the pronator teres and flexor musculature, superficial to the brachial artery and median nerve, by placing the transducer over the anterior elbow angled from the biceps brachii tendon distal and medial ( Fig. 4.3C ).



The transducer is then moved proximal again to where the biceps brachii is superficial to the brachialis and is rotated 90 degrees ( Fig. 4.4 ). At this location, the biceps tendon will be hyperechoic and fibrillar with a uniform thickness over the brachialis muscle ( Fig. 4.4B ). As the biceps brachii tendon courses deep along the outer contour of the brachialis, the tendon will become hypoechoic from anisotropy ( Fig. 4.4C ). Using the heel-toe maneuver, the sound beam is angled superiorly in order to image the tendon perpendicular to eliminate anisotropy ( Fig. 4.4D ). Some ultrasound machines will have beam steering, which can assist in reducing anisotropy ( Fig. 4.4E and F ). If the distal biceps is difficult to visualize, the elbow position may be changed with additional minimal flexion or extension.

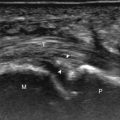
If the distal biceps brachii tendon insertion onto the radial tuberosity in long axis is not clearly seen from an anterior approach, a medial approach should be used ( Fig. 4.5 ), which can be accomplished in several different ways. With one method, the transducer is long axis to the biceps brachii tendon in the sagittal plane on the body, as described in the anterior approach. The transducer is then moved slightly medial until the brachial artery is identified and then the beam is angled slightly lateral toward the center of the elbow to see the biceps tendon ( Fig. 4.5A ). This maneuver is repeated, while adding the heel-toe maneuver until the distal tendon is visualized, where often slight elbow flexion is helpful ( Fig. 4.5B ). Another method is to follow the biceps brachii tendon distally in short axis, moving the transducer toward the medial elbow, and then turning long axis once the footprint is identified. A third method (the pronator window approach) is to begin with the elbow flexed and the transducer over the medial epicondyle in the coronal plane ( Fig. 4.5C ). The transducer is then moved toward the wrist and slightly anteriorly to visualize the radial tuberosity and the biceps brachii tendon in long axis ( Fig. 4.5D ).



Dynamic assessment of the distal biceps brachii is very helpful to distinguish partial from nonretracted full-thickness tear. While this can be effectively accomplished when evaluating the biceps tendon from a medial approach, as described ( ), an additional method to dynamically assess the biceps brachii tendon is from a lateral approach with the elbow flexed. Examination with this technique begins with the transducer in short axis relative to the proximal radius ( Fig. 4.6 ). The radial head is visualized as a curvilinear echogenic structure, and the transducer is moved toward the wrist over the radial neck, where the surrounding supinator muscle can be seen. At this level, the hand can be passively supinated and pronated to visualize movement of the biceps brachii tendon, which is perpendicular to the sound beam ( ). When the hand is fully pronated, the transducer can be moved dorsally toward the ulna to visualize the distal biceps brachii tendon ( Fig. 4.7 ). While this dorsal evaluation with elbow flexion and pronation has limited diagnostic value in that only the distal-most segment of biceps tendon is visible between the radius and ulna, this view is ideal when guiding a needle for biceps tendon fenestration or injection.


To complete the anterior evaluation of the elbow, the transducer is returned to the sagittal plane directly in long axis to the brachialis to visualize the anterior recess of the elbow joint ( Fig. 4.8A and B ). Here, the coronoid fossa and smaller radial fossa are visible as concavities in the distal humerus. Within these fossae, a triangular hyperechoic intracapsular fat pad is normally seen. The hypoechoic hyaline cartilage of the trochlea and capitellum can also be identified. Returning to the original short axis view of the brachial artery, the normal median nerve is again identified in short axis and can be followed distally as it courses between the humeral and ulnar heads of the pronator teres, a potential site of nerve entrapment ( Fig. 4.8C and D ). The ulnar head of the pronator teres is located between the median nerve and the ulnar artery.



Medial Evaluation
For medial evaluation, the elbow is slightly flexed to bring the anterior bundle of the ulnar collateral ligament into the coronal plane. Sonographic evaluation of the medial elbow structures begins by visually identifying or palpating the medial epicondyle of the humerus. The transducer is then placed in long axis to the forearm with the proximal aspect over the medial epicondyle ( Fig. 4.9 ). The characteristic hyperechoic bony contour of the medial epicondyle and the sloped surface of the humerus distally to its articulation with the ulna should be identified. In this imaging plane long axis to the forearm, as indicated by the characteristic bone contours, both the common flexor tendon and the anterior bundle of the ulnar collateral ligament can be identified ( Fig. 4.9B ). The origin of the common flexor tendon should be seen at the superficial aspect of the medial epicondyle as hyperechoic and fibrillar, with transition to hypoechoic musculature more distally. In addition, the anterior bundle of the ulnar collateral ligament is seen attached to the medial epicondyle as hyperechoic and fibrillar, but somewhat more compact than that of tendon. If not perpendicular to the ligament, the anterior bundle of the ulnar collateral ligament will be hypoechoic from anisotropy, but still fairly uniform in thickness where it extends distally over the joint space to insert on the proximal ulna. The anterior bundle of the ulnar collateral ligament has a somewhat variable appearance at its proximal attachment to the humerus; it may appear as a uniform bundle, or it may fan out more proximally, interspersed with hyperechoic fatty tissue. The distal aspect of the ulnar collateral ligament anterior bundle attaches to the sublime tubercle and the ulna more distally. The normal joint recess of the elbow extends proximally between the anterior bundle of the ulnar collateral ligament and adjacent humerus, but it should not extend medially from this point at the humeral attachment of the ligament or distal over the ulna. The long axis view is the key plane in the imaging of both the common flexor tendon and anterior bundle of the ulnar collateral ligament, although if a pathologic process is identified, further characterization is completed by imaging in short axis to these structures. In addition, the ulnar collateral ligament and medial joint space can be evaluated with dynamic valgus stress with the elbow in slight flexion (at least 30 degrees) to assess for ligamentous injury.


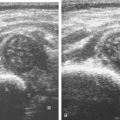
After evaluation of the common flexor tendon and anterior bundle of the ulnar collateral ligament is completed, attention is turned to the cubital tunnel region. For this evaluation, the elbow is turned outward so that the bony protuberances of the olecranon process and the medial epicondyle can be visualized and are palpable. Evaluation should begin with the elbow extended; if the elbow is flexed at this point, it is possible that the ulnar nerve may dislocate and be difficult to locate, and identification of an anconeus epitrochlearis becomes difficult as well (see discussion later in this chapter). The ultrasound transducer is placed in the transverse plane between the olecranon process and the medial epicondyle, and the characteristic hyperechoic and shadowing bone contours of these structures are seen ( Fig. 4.10A and B ). The ulnar nerve is visible as speckled or honeycomb in appearance from hypoechoic nerve fascicles and hyperechoic connective tissue; however, the ulnar nerve posterior to the medial epicondyle often appears hypoechoic from physiologic edema but should not be enlarged. The ulnar nerve may also be bilobed or bifid. Superficial to the ulnar nerve, the cubital tunnel retinaculum (or Osborne fascia) is located and, when present, appears as a thin structure between the olecranon and medial epicondyle. The posterior bundle of the ulnar collateral ligament is deep to the ulnar nerve. Distally, the ulnar nerve can be followed into the true cubital tunnel between the humeral and ulnar heads of the flexor carpi ulnaris and under the arcuate ligament ( Fig. 4.10C ). With rotation of the transducer 90 degrees, the ulnar nerve can be evaluated in long axis ( Fig. 4.10D and E ).





The cubital tunnel region should also be assessed dynamically for pathology. With the transducer again placed in the transverse plane between the medial epicondyle and olecranon process and fixed over the medial epicondyle, the elbow is passively flexed ( Fig. 4.11 ). During this maneuver, the olecranon process moves out of the imaging plane and is replaced by the hypoechoic triceps brachii muscle. Initially performing this maneuver passively is helpful to control the speed of flexion. In addition, the movement can be momentarily stopped and the transducer repositioned if the bone contour of the medial epicondyle apex is not visualized. Normally during elbow flexion, the ulnar nerve moves toward the apex of the medial epicondyle but should not translate over the epicondyle anteriorly. Abnormal ulnar nerve translation over the medial epicondyle may be felt as a palpable snap through the transducer, and typically it returns back into normal position as the elbow is extended. One should avoid too much pressure with the transducer during this dynamic evaluation because this may inhibit the abnormal ulnar nerve translation; intermittent reduction in transducer pressure during the maneuver avoids this pitfall. Ulnar nerve dislocation has been described in up to 20% of asymptomatic individuals, although abnormal movement predisposes to nerve irritation and injury. Isolated ulnar nerve dislocation should also be differentiated from snapping triceps syndrome. In this latter situation, in addition to ulnar nerve dislocation, there is subluxation of the triceps muscle medial head over the medial epicondyle of the humerus in elbow flexion.


Lateral Evaluation
For evaluation of the lateral elbow structures, the arm is rotated inward and slightly flexed. Structures of interest laterally include the common extensor tendon, the lateral collateral ligament complex, the radial head and annular recess, and the capitellum. Unlike the medial aspect of the elbow, the lateral epicondyle is not clearly visible to the eye and is more difficult to palpate; therefore, bone landmarks as seen at sonography are used for orientation. To begin, the transducer is placed in long axis relative to the forearm over the lateral elbow ( Fig. 4.12A ), and the characteristic hyperechoic shadowing contour of the radial head is readily identified ( Fig. 4.12B ). More proximal scanning in this plane reveals the radius articulation with the capitellum, and, more proximally, the relatively flattened contour of the lateral epicondyle. At this site, the hyperechoic and fibrillar common extensor tendon and the deeper radial collateral ligament can be seen attaching to the lateral epicondyle ( Fig. 4.12C ). Although the long axis view is optimum in identification of the common extensor tendon given the characteristic bone landmarks for orientation, any abnormality should also be characterized in short axis as well. Care should be taken to include evaluation of the most anterior aspect of the common extensor tendon, where tendon abnormalities most commonly occur. Distinguishing the common extensor tendon from the underlying radial collateral ligament in long axis may be difficult as both are hyperechoic and fibrillar; however, knowledge of their footprint anatomy on the lateral epicondyle is helpful as the superficial common extensor tendon originates from the proximal 46% of the bone surface and a bony ridge separating the footprints may also be seen. In addition, during real-time scanning the common extensor tendon and radial collateral ligament can be differentiated as they are slightly oblique to each other and an echogenic interface may be seen. Lastly, the radial collateral ligament extends distal to the annular ligament superficial to the radial head, whereas the more superficial common extensor tendon courses distal and becomes muscle. At the radiocapitellar joint, a hyperechoic, triangular, meniscus-like synovial reflection or fold, also termed the posterolateral plica , extends from the radial collateral ligament and joint capsule into the joint. To visualize the lateral ulnar collateral ligament, the transducer is centered over the annual ligament long axis to the radial collateral ligament and then angled dorsally to visualize its attachment to the crista supinator of the ulna; this ligament often appears hypoechoic from anisotropy but should be uniform in thickness ( Fig. 4.12D ). The annual ligament is also evaluated in long axis (in the transverse plane over the radial head). At the level of the radial neck, the collapsed annular recess is difficult to discern unless it is abnormally distended (see Fig. 4.20B ).




With elbow extension and the transducer anterolateral in the sagittal plane, the thin uniform hypoechoic layer of hyaline cartilage can be seen over the anterior aspect of the capitellum ( Fig. 4.13A ). With movement of the transducer posteriorly over the capitellum, the irregular cortex represents a normal appearance void of cartilage and should not be misinterpreted as an osteochondral abnormality. With the elbow in flexion and the transducer posterior in the sagittal plane, the central and posterior aspect of the capitellum hyaline cartilage can also be visualized ( Fig. 4.13B ).

For evaluation of the radial nerve, one approach is to first find the oblique fascial plane between the brachioradialis and the brachialis anteriorly in the transverse plane, where the deep and superficial branches of the radial nerve are seen as round and hypoechoic ( Fig. 4.14A ; see Fig. 4.2B ). These individual branches can be followed proximally in short axis where they join to form the radial nerve ( Fig. 4.14B ). Evaluation can continue more proximal to follow the radial nerve as it traverses the intermuscular fascia and follows the posterior cortex of the humerus. Following the radial nerve branches distally, the deep branch is seen entering into the supinator muscle becoming the posterior interosseous nerve ( Fig. 4.14C ). The transducer is turned 90 degrees to evaluate the radial nerve and its branches in long axis as well ( Fig. 4.14D ). The deep branch of the radial nerve often changes shape as it passes beneath the arcade of Fröhse and should not be interpreted as nerve swelling. The superficial branch of the radial nerve may also be followed distally into the forearm.

Posterior Evaluation
To evaluate the posterior structures of the elbow, the patient’s elbow is flexed to 90 degrees. If the patient is supine, this can be accomplished by asking the patient to place his or her hand across the abdomen. Structures of interest include the posterior joint recess, the triceps brachii, and the soft tissues over the olecranon. By placing the transducer posteriorly in the sagittal plane over the proximal elbow, the characteristic hyperechoic shadowing bone contours of the humerus are identified ( Fig. 4.15 ). As the humeral diaphysis approaches the elbow joint, there is a pronounced concavity, which represents the olecranon fossa. This is also demonstrated in the transverse plane relative to the humerus ( Fig. 4.16 ). This fossa is normally filled with the hyperechoic posterior elbow fat pad and is the site of evaluation for joint fluid, intra-articular bodies, and other joint processes. The hypoechoic trochlear and capitellum hyaline cartilage can also be identified. Superficial to the olecranon recess, the hypoechoic triceps brachii muscle and more distal hyperechoic tendon can be seen inserting onto the olecranon process. The superficial layer of the triceps brachii represents the confluence of the lateral and long heads, whereas the deeper layer with a very short tendon represents the medial head of the triceps brachii. With elbow extension, the soft tissues superficial to the olecranon process can be evaluated for olecranon bursal fluid. A thick layer of gel should be used to float the transducer so as to avoid compression and displacement of olecranon bursal fluid away from view. Although the sagittal plane is most important in evaluation of the described posterior anatomy, pathology should also be characterized in the orthogonal transverse.




Joint and Bursal Abnormalities
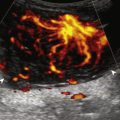
Although a joint effusion may distend the anterior and less commonly the annular joint recesses, the posterior olecranon recess in elbow flexion is the most sensitive location for identification of joint fluid ( Fig. 4.17 ). Imaging in the sagittal plane over the posterior joint recess demonstrates superior and posterior displacement of the hyperechoic fat pad when the joint is distended, similar to findings at radiography. Fat pad displacement, both in the anterior and posterior joint fossae, may result from anechoic simple fluid, although complex fluid may vary from hypoechoic to hyperechoic ( Fig. 4.18 ). Heterogeneous joint fluid may be caused by hemorrhage or infection ( Fig. 4.19 ). Synovial hypertrophy, commonly diffuse, may also distend the joint recesses and may appear hypoechoic (or, less commonly, isoechoic or hyperechoic) relative to the subcutaneous fat. The findings of joint recess compressibility, redistribution or motion of joint recess contents with transducer pressure or joint movement, and lack of internal flow on color Doppler imaging suggest complex fluid rather than synovial hypertrophy when their gray-scale appearances are similar. Synovial hypertrophy may be the result of infection ( Fig. 4.20 ), rheumatoid arthritis ( Fig. 4.21 ), and other inflammatory arthritides ( Fig. 4.22 ) or less likely an adjacent bone process, such as intra-articular osteoid osteoma ( Fig. 4.23 ). Chronic synovial hypertrophy can result in significant distention of the joint recesses, potentially compressing the ulnar nerve ( Fig. 4.24 ) and radial nerve ( Fig. 4.25 ). In the setting of synovitis, cortical discontinuity and irregularity could represent bone erosions (see Fig. 4.21 ). Other synovial proliferative disorders, such as pigmented villonodular synovitis and synovial chondromatosis ( Fig. 4.26 ), should be considered, with possible calcified hyperechoic foci identified within the synovium in the latter condition.



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree