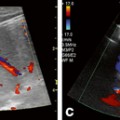
Fig. 12.1
Transducer positioning for the hepatorenal area (a), normal view of Morison’s pouch (b), and an abnormal exam with free fluid between liver and kidney denoted by white arrow (c). Panel c courtesy of Geoffrey E. Hayden, MD, RDMS
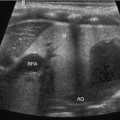
The splenorenal fossa is in an analogous position on the left side of the abdomen and is often relevant in the setting of suspected splenic trauma. The probe is placed in the left posterior axillary line at the inferior intercostal spaces and positioned to provide a coronal view of the interface between spleen and left kidney (Fig. 12.2). The entirety of the spleen can be seen with slight translation and rotation of the probe in this fashion. Positive findings again entail anechoic areas representing free intraperitoneal fluid in either the splenorenal or splenodiaphragmatic spaces. If difficulties are encountered visualizing either the hepatorenal or splenorenal views, asking the patient to hold full inspiration, if possible, can slide the area of interest more inferiorly and into better view. More posterior positioning of the probe to the extent that the bed or gurney allows is also often helpful in avoiding bowel gas.
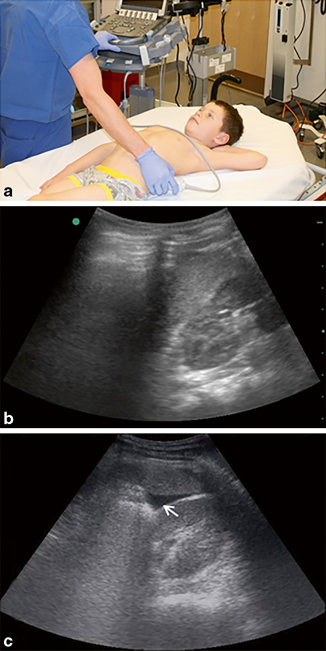
Fig. 12.2
Transducer positioning for the splenorenal area (a), normal view of the recess (b), and an abnormal exam with free fluid between spleen and kidney denoted by white arrow (c). Panel c courtesy of Geoffrey E. Hayden, MD, RDMS
Suprapubic positioning of the probe allows assessment of the dependent areas of the inframesocolic peritoneum, which are the rectovesicular pouch in males and the rectouterine pouch (of Douglas) in females. The transducer is placed immediately cephalad to the pubic bone and the array angled inferiorly into the pelvis (Fig. 12.3), where the bladder is generally easily seen. Longitudinal and transverse images are both typically obtained, with particular attention paid to the posterior border of the bladder, where fluid can be seen as an anechoic stripe.
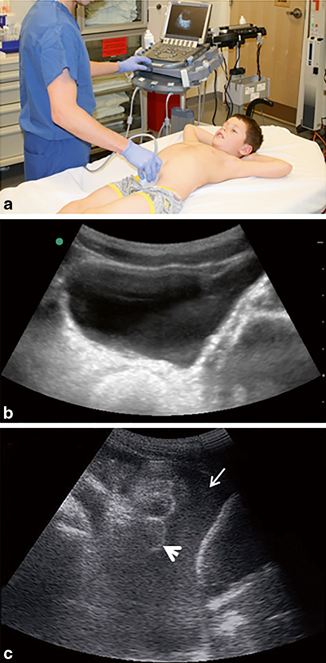
Fig. 12.3
Transducer positioning for the suprapubic area (a), normal view of the bladder (b), and an abnormal exam with free fluid around bladder and freely floating bowel loops, denoted by white arrow and arrowhead, respectively (c). Panel c courtesy of Geoffrey E. Hayden, MD, RDMS
Finally, interrogation of the pericardial space is a useful benefit of the FAST exam in blunt trauma. Hemopericardium and the resultant tamponade can be a consequence of either direct sternal impact or a deceleration injury that coincides with subxiphoid abdominal impact. There are two acceptable ways in which cardiac views can be obtained by ultrasound. A subxiphoid approach entails placing a transducer just inferior to the xiphisternum and directing it towards the left shoulder with the probe marker pointed to the right shoulder to aquire a four-chamber view of the heart and surrounding pericardium (Fig. 12.4). However, this requires a fair amount of deep pressure into the abdomen and may not be tolerated by all patients. Alternatively, a parasternal long-axis view can be achieved by orienting the probe in a parasagittal axis just to the left of the sternum and locating an interspace that permits identification of the heart. In either view, finding more than trace fluid in the dependent posterior pericardial space is abnormal and should be considered a positive finding.
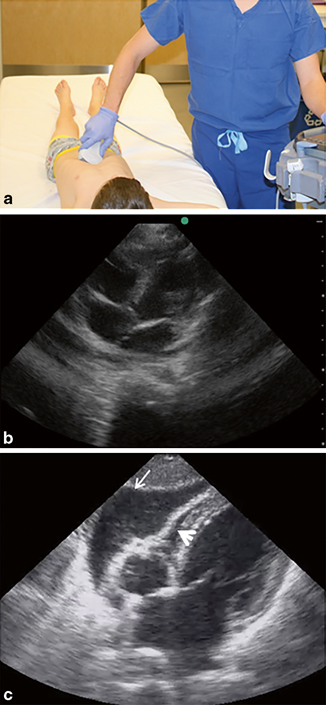
Fig. 12.4
Transducer positioning for subxiphoid view of pericardium (a), normal four-chamber view of the heart (b), and pericardial tamponade with pericardial fluid and right ventricular collapse denoted by white arrow and arrowhead, respectively (c). Panel c courtesy of Geoffrey E. Hayden, MD, RDMS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree