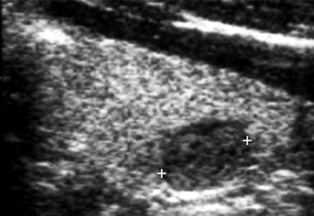
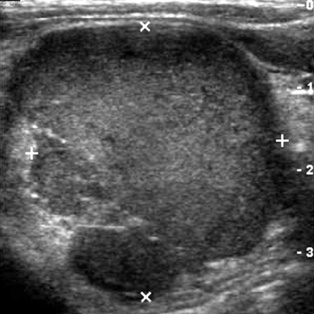
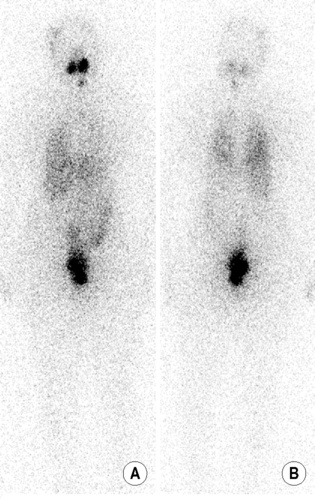
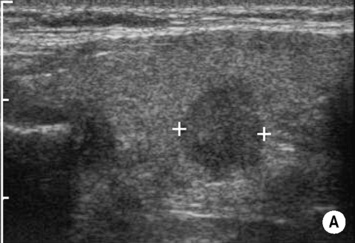
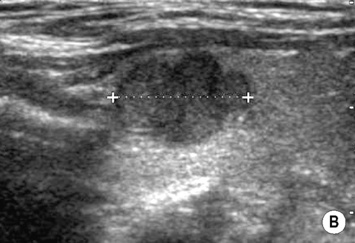
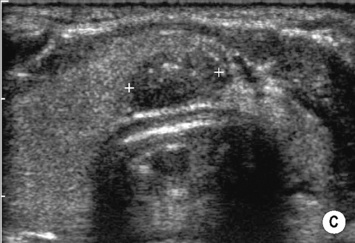
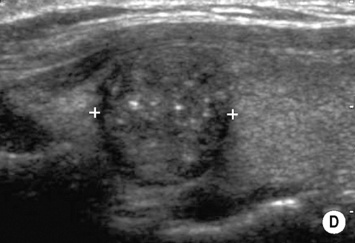
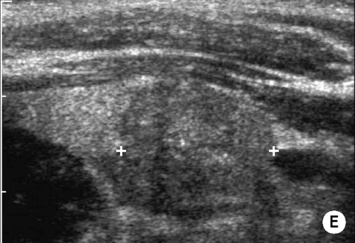
• A malignant tumour arising from the thyroid or parafollicular C cells • Risk factors: previous radiation exposure • 99mTc-pertechnetate is not used for detecting metastatic disease • Other sites demonstrating similar uptake: salivary glands • More than 80% of solitary nodules are hypofunctioning ‘cold’ nodules: up to 20% of these are tumours • Approximately 10% of solitary nodules are hyperfunctioning ‘warm’ nodules (on a background of normal thyroid activity): up to 10% of these will be tumours • Up to 5% of solitary nodules are hyperfunctioning ‘hot’ nodules (on a background of suppressed remaining thyroid activity): these are very rarely malignant • There is a reduced incidence of malignancy with an increasing number of nodules detected: whilst less likely than with a solitary nodule, a cold nodule within a multinodular goitre can still represent a malignancy • Thyroid nodules appear as low attenuation lesions (particularly after IV contrast medium) • US features of benign and malignant thyroid nodules (FNAC is still required for suspicious lesions) US features of benign and malignant thyroid nodules (FNAC is still required for suspicious lesions) Multiple endocrine neoplasia (MEN) • Papillary/follicular tumours: thyroidectomy ± lymph node dissection ± postoperative 131I-ablation therapy • Anaplastic tumours: radical or palliative radiotherapy ± chemotherapy • Medullary carcinoma: thyroidectomy ± radiotherapy (with chemotherapy for advanced disease) • Whole-body iodine imaging is performed after discontinuing thyroid hormone (for 4 weeks for T4 or for 2 weeks for T3) and establishing that TSH concentrations are > 30μmol/L • In patients following removal of a medullary carcinoma, serum calcitonin concentrations are used to diagnose recurrence • Generally (but not always) this is a benign disorder • Dominant cold nodules (especially enlarging ones) require further evaluation by aspiration biopsy • Autonomous foci are common and if extensive will ultimately result in hyperthyroidism (a toxic multinodular goitre or Plummer’s disease) Thyroid malignancies – key features
Endocrine system
THYROID CANCER
THYROID CANCER
DEFINITION
 it is an uncommon tumour (accounting for 0.5% of all cancer deaths)
it is an uncommon tumour (accounting for 0.5% of all cancer deaths)
 iodine excess
iodine excess  a genetic predisposition
a genetic predisposition  alcohol excess
alcohol excess
RADIOLOGICAL FEATURES
99mTc-pertechnetate scintigraphy
 gastric mucosa
gastric mucosa  choroid plexus
choroid plexus
 if one of these lesions is malignant it will usually be cold with 123I imaging
if one of these lesions is malignant it will usually be cold with 123I imaging
CT
Benign
Malignant
Nodule characteristics
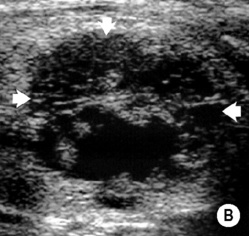
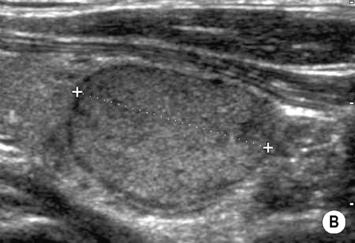
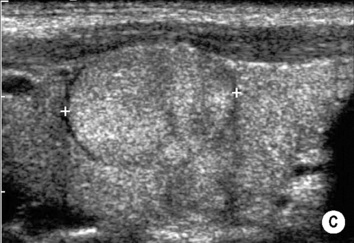
• A cystic nodule ± debris ± septations  a sponge-like nodule
a sponge-like nodule
• Posterior acoustic shadowing
• A hyperechoic nodule
• ‘Comet tail’ artefact (colloid nodule)
• Multiple isoechoic nodules (multinodular goitre)
• Multiple hypoechoic nodules (Hashimoto’s thyroiditis)
• Indeterminate: a solid well-defined nodule ± cystic components
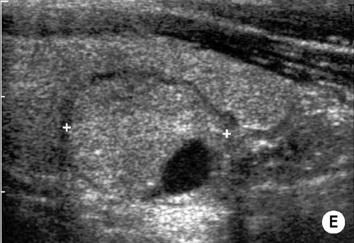
• Solid nodules protruding into the cystic space
• No posterior acoustic shadowing
Peripheral halo
• A thin uniform halo
• An incomplete, irregular or thickened halo
Nodule margin
• Smooth regular margins
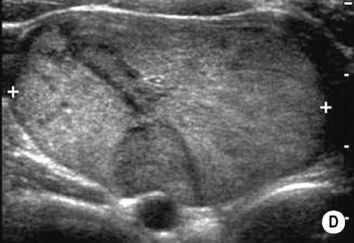
• An irregular, lobulated or poorly defined margin
Calcification
• This is generally absent (eggshell calcification may be present)
• Microcalcification  fine or coarse calcification (commonly papillary or medullary carcinomas)
fine or coarse calcification (commonly papillary or medullary carcinomas)
Metastatic spread
• Invasion of the adjacent tissues ± enlarged ipsilateral or bilateral cervical lymph nodes
MEN type I
• Parathyroid adenoma or hyperplasia (hyperthyroidism)
• Pancreatic islet cell tumours
• Pituitary adenoma
MEN type IIA
• Parathyroid hyperplasia
• Adrenal medullary tumour
• Medullary thyroid cancer
MEN type IIB
• Medullary thyroid cancer
• Adrenal medullary tumour
• Marfanoid features, multiple cutaneous and mucosal neuromas, neurofibromas and gastrointestinal ganglioneuromas
PEARLS
Treatment
 thyroglobulin can be used as a postoperative tumour marker if there has been complete resection
thyroglobulin can be used as a postoperative tumour marker if there has been complete resection  radical radiotherapy and chemotherapy can be used for locally advanced or metastatic disease
radical radiotherapy and chemotherapy can be used for locally advanced or metastatic disease
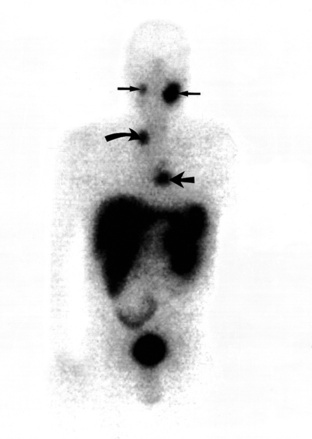
Subsequent follow-up
 one can then identify most functioning metastases, which are usually located in the neck, lungs or bone
one can then identify most functioning metastases, which are usually located in the neck, lungs or bone
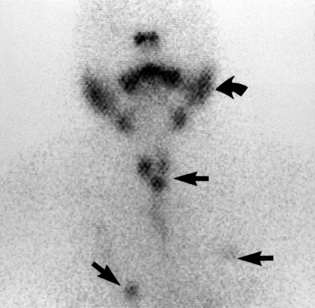
 if they become elevated, pentavalent 99mTc-DMSA, 111In-DTPA-octreotide, or 123I-MIBG can be used for the detection of recurrent or residual disease
if they become elevated, pentavalent 99mTc-DMSA, 111In-DTPA-octreotide, or 123I-MIBG can be used for the detection of recurrent or residual disease  in cases of 123I-MIBG-positive disease, therapy with 131I-MIBG can be instituted
in cases of 123I-MIBG-positive disease, therapy with 131I-MIBG can be instituted
Multinodular goitre
Description
Pattern of spread
Papillary carcinoma (50–80%)
Low-grade tumours with a good prognosis (histologically multicentric)  tumours concentrate radio-iodine
tumours concentrate radio-iodine
Early lymph node spread (metastatic lymph nodes may be normal in size, cystic, calcified, haemorrhagic or contain colloid)  distant metastases are rare (and usually to the lungs)
distant metastases are rare (and usually to the lungs)
Follicular carcinoma (10–40%)
Slow growing  tumours concentrate radio-iodine
tumours concentrate radio-iodine
It rarely metastasizes to the regional lymph nodes  the tendency is to spread via the bloodstream and disseminate to the lungs, bones or liver
the tendency is to spread via the bloodstream and disseminate to the lungs, bones or liver
Anaplastic carcinoma (10%)
Undifferentiated malignant tumours (which do not concentrate radio-iodine)  there is a poor prognosis
there is a poor prognosis  they tend to occur in older patients
they tend to occur in older patients  punctate calcification and necrosis is frequently present
punctate calcification and necrosis is frequently present
Lymphatic metastases occur in the majority of patients
Medullary carcinoma (5%)
This originates from the parafollicular C cells  it does not concentrate radio-iodine
it does not concentrate radio-iodine  it may be sporadic or familial (and associated with the MEN type II syndrome or other endocrine neoplasms)
it may be sporadic or familial (and associated with the MEN type II syndrome or other endocrine neoplasms)  it is usually a unilateral solitary lesion
it is usually a unilateral solitary lesion  calcification is seen in 10%
calcification is seen in 10%  123I-MIBG and somatostatin analogues (e.g. octreotide) can be used for evaluation
123I-MIBG and somatostatin analogues (e.g. octreotide) can be used for evaluation  circulating calcitonin levels are usually elevated
circulating calcitonin levels are usually elevated
It may invade locally, spread to the regional nodes, or demonstrate haematogenous spread to the lungs, bones or liver
Lymphoma (10%)
It is usually a non-Hodgkin’s lymphoma  it occurs in ⅓ of patients with Hashimoto’s thyroiditis (a MALT-type lymphoma)
it occurs in ⅓ of patients with Hashimoto’s thyroiditis (a MALT-type lymphoma)  it presents as a rapidly enlarging solitary nodule (80%) or as multiple nodules (imaging cannot distinguish between a lymphoma and thyroiditis)
it presents as a rapidly enlarging solitary nodule (80%) or as multiple nodules (imaging cannot distinguish between a lymphoma and thyroiditis)  necrosis and calcification is uncommon
necrosis and calcification is uncommon
It can involve the nodes with spread to the GI tract
Metastases (<1%)
The commonest primary is renal cell carcinoma
 there can be hoarseness (due to recurrent laryngeal nerve involvement), dysphagia or hyperthyroidism
there can be hoarseness (due to recurrent laryngeal nerve involvement), dysphagia or hyperthyroidism it cannot differentiate between a follicular adenoma or adenocarcinoma (histologically the distinction relies on documenting capsular or venous invasion and this requires a core biopsy)
it cannot differentiate between a follicular adenoma or adenocarcinoma (histologically the distinction relies on documenting capsular or venous invasion and this requires a core biopsy) once in the thyroid gland it is not incorporated into thyroglobulin
once in the thyroid gland it is not incorporated into thyroglobulin it can be used for detecting metastatic disease
it can be used for detecting metastatic disease there is increasing uptake with less differentiated tumour types
there is increasing uptake with less differentiated tumour types  it can also be used in medullary cancer
it can also be used in medullary cancer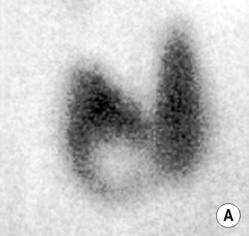
 the size of the tumour
the size of the tumour  the degree of differentiation
the degree of differentiation  the presence of invasion, nodal or distant metastases
the presence of invasion, nodal or distant metastases anaplastic and medullary cancers do not concentrate 131I and are thus not detectable by iodine scanning
anaplastic and medullary cancers do not concentrate 131I and are thus not detectable by iodine scanning like CT, false-positive results can be caused by inflammatory lymphatic hyperplasia and granulation tissue
like CT, false-positive results can be caused by inflammatory lymphatic hyperplasia and granulation tissue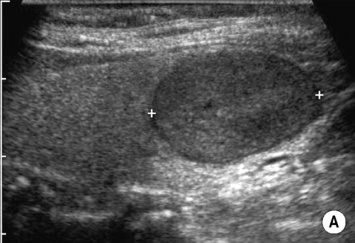

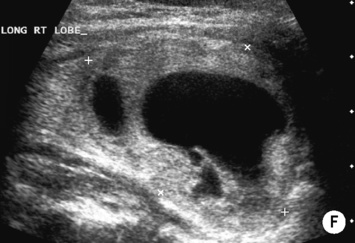
 with a pre-existing normal thyroid this will result in a diffuse toxic goitre
with a pre-existing normal thyroid this will result in a diffuse toxic goitre  there may underlying thyroid disease in 5–10% of patients (e.g. solitary thyroid nodules, a multinodular goitre, or Hashimoto’s thyroiditis)
there may underlying thyroid disease in 5–10% of patients (e.g. solitary thyroid nodules, a multinodular goitre, or Hashimoto’s thyroiditis)







