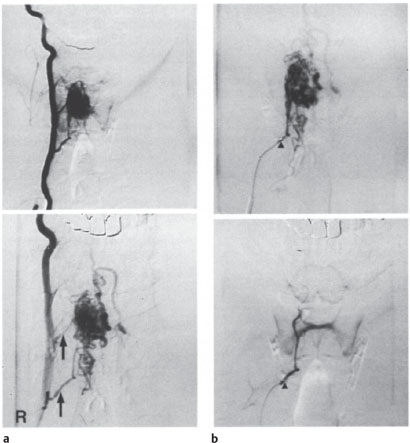
5 Endovascular Therapy and Other Minimally Invasive Treatments for Spinal Diseases Contents Catheterization Techniques and Embolic Materials Treatment of Angiodysplasias and AV Fistulas Preoperative Devascularization of Hypervascular Tumors Indications and Contraindications Methods, Results, and Complications Treatment Principles The spinal diseases that are accessible to endovascular therapy include the following: • Dural AV fistulas (dural fistulas), • AV malformations, • Hypervascular tumors. An essential prerequisite is the availability of digital subtraction angiography (DAS) with a highresolution image matrix (at least 512×512) and the capacity for simultaneous biplanar imaging. This makes it possible to check the result of the embolization without loss of time. Generally the patient is awake and cooperative during the procedure. General anesthesia is indicated only if the patient’s ability to cooperate is impaired. The recording of evoked potentials is unnecessary during the procedure as long as close clinical supervision is maintained. The initial part of the procedure follows the technique used in spinal angiography (see p. 273), and basically the same materials are used as in the endovascular treatment of craniocerebral lesions. The therapeutic goal of spinal endovascular procedures is to obliterate the spinal lesion as completely as possible. Complete obliteration is an essential goal for dural fistulas, while hemodynamic improvement is an acceptable goal for large intradural arteriovenous (AV) malformations. Generally the same techniques can be used as in the treatment of cerebral angiodysplasias. But due to certain peculiarities in the spinal vascular system, especially in the territory of the anterior spinal artery, it is somewhat more difficult to find a safe and effective embolization site than in the brain. The question of whether tissue adhesive can be deposited within the nidus or whether particle embolization is feasible can be determined only on a case-by-case basis, giving due consideration to the procedural risk. Before treatment is initiated, it is essential to devise a treatment plan based on spinal angiographic findings, discuss the plan with the patient, and if necessary coordinate the plan with a neurosurgeon and with surgical options. General information on nonendovascular minimally invasive procedures relevant to the spine can be found on page 384 ff. Catheterization Techniques and Embolic Materials The special catheter used for selective vascular catheterization is introduced through a femoral arterial sheath. It should be able to accommodate a coaxial flow-directed or wire-directed microcatheter. In rare cases, the use of a balloon-tipped catheter may be considered if the access vessel is large enough. The embolic materials consist almost exclusively of liquid tissue adhesives that harden on contact with anions, such as Histoacryl and Bucrylate, and polyvinyl alcohol (PVA) particles (Ivalon) with a size range of 50–300 μm. The successful use of tissue adhesives (glues) requires considerable experience, especially in estimating the polymerization time and how it is affected by adding the oily contrast medium Lipiodol. Because the glues are not radiopaque, tantalum powder should also be added to improve visualization. Glucose, an anion scavenger, is injected first to keep the glue from hardening prematurely while still in the microcatheter. After a certain quantity of adhesive has been injected, the microcatheter must be withdrawn quickly to avoid gluing the catheter to the vessel. Cyanoacrylate glues lead to inflammatory changes in the vessel wall and incite foreign body reactions. When used properly, they provide permanent vascular occlusion. On the other hand, embolization with PVA particles is often followed by recanalization, most likely due to the fibrinolytic breakdown of secondary thromboses. The particles, mixed with contrast material, are administered in fractionated doses under fluoroscopic control. Embolization should be discontinued at once if stasis or reflux occurs. Treatment of Angiodysplasias and AV Fistulas Dural AV Fistulas The goal of treating this type of fistula is to permanently occlude the dural shunt along with the origin of the draining vein. This can be done surgically or by an endovascular approach. Endovascular treatment. The endovascular treatment of a dural AV fistula is contraindicated if spinal angiography demonstrates a radiculomedullary supply vessel at the same level. Permanent endovascular occlusion of the fistula can be accomplished with tissue adhesives of the cyanoacrylate type (Fig. 5.1). After the segmental artery has been catheterized, the microcatheter is advanced superselectively into the spinal branch that supplies the dura. The mixture of glue and Lipiodol should be adjusted for a polymerization time that will allow the injected material to reach the fistula site and the mouth of the draining vein but will prevent the material from entering the medullary veins where it might cause ischemia or hemorrhage within the cord. Spinal angiography should be repeated 1–2 months after the embolization to check for disease progression with recruitment of collateral feeders (following an incomplete embolization). Embolization with PVA particles is considered inadequate due to the high recanalization rate. Operative treatment. Dural AV fistulas can be exposed and obliterated through a laminectomy or hemilaminectomy by identifying and clipping the arterialized vein that runs along the nerve root at the intrathecal level. The dural shunt itself may be left alone. For a successful operation, the level of the fistula must first be accurately determined by angiography. With typical intraoperative findings and successful clipping, there is no need for postoperative angiographic follow-up. Surgery and endovascular therapy have low complication rates when suitable precautions are taken. According to published data and our own experience, embolization has a successful occlusion rate of 70–81%. The advantage of surgery is that it offers higher confidence in occluding the fistula. It is also safer in terms of preserving angiographically occult arteries that supply the spinal cord. AV Malformations (Angiomas) These very rare angiodysplasias located on or in the spinal cord usually require a combination of surgery and endovascular therapy. Some AV malformations are not treatable by any method. Per imedullary angiomas are generally an indication for surgical treatment. Once the fistulous connection between a spinal cord artery and vein has been precisely located by angiography, it can usually be occluded surgically (or in rare cases with an endovascular balloon) without much difficulty. For glomus-type angiomas with numerous feeders, a low-risk embolization depends on the accessibility of the nidus. Reaching an effective embolization point is no longer a rarity, however, when modern microcatheters are used (Fig. 5.2). Given the high shunt volume in large AV malformations, there is a danger that, even with superselective catheterization, all supply vessels to the spinal cord will not be visualized after contrast injection. The choice of embolic material is determined largely by the intended site of superselective catheter placement and whether the lesion will be accessed through the anterior spinal artery or through a posterolateral spinal artery. Flow sufficient for the embolization must be preserved. If the embolization is done over a relatively long vascular segment because the microcatheter cannot be placed close to the nidus, the use of particles is preferred. For lesions in the territory of the anterior spinal artery, the catheter must be maneuvered into the nidus before depositing adhesive material. Fig. 5.1 a-c Endovascular occlusion of a thoracic dural fistula. a Anteroposterior (AP) thoracic myelogram shows long, meandering filling defects (arrows) that are characteristic of abnormally dilated and elongated medullary blood vessels. b Contrast injection into the ninth intercostal artery on the rightside opacifies the vascular malformation. the arrowhead marks the location of the dural fistula. the straight arrow indicates the direction of intradural venous drainage, which is more caudad than cephalad following a partial reversal at the level of the curved arrow. c The fistula has been completely obliterated by embolization with tissue adhesive. Spinal angiogram; AP projection. In the treatment of AV malformations with multiple vascular pedicles, the embolization can be staged by partially embolizing the lesion in an initial sitting. If this leads to a decrease in the caliber of remaining arterial feeders, these vessels can then be superselectively catheterized and occluded. Unlike spinal dural fistulas, some spinal A V malformations can be successfully managed by particle occlusion (Figs. 5.2, 5.3). With modern microneurosurgery, moreover, it is possible to remove at least small or partially embolized intramedullary AV malformations. Magnetic resonance imaging (MRI) has an important role in planning the approach for this type of surgery. With spinal angiomas that cannot be completely eliminated, partial embolization is often sufficient to relieve or improve the patient’s symptoms. Clinical improvement can also be obtained in some cases by staged particle embolization, even if only partial embolization is achieved. Embolization is even recommended in patients wh o already have a fixed neurologic deficit due to a cervical or high thoracic AV malformation, since intramedullary hemorrhage from these lesions can spread to the craniocervical region, with life-threatening consequences. Fig. 5.2 a-c Endovascular occlusion of a thoracic AV malformation of the glomus type. a The vascular malformation (large arrow) is supplied from the left tenth intercostal artery via the great radicular artery (left, small arrows) and from the left second lumbar artery via the posterolateral artery (right, small arrows). Spinal angiograms; AP projection b Superselective visualization of the lesion (large arrows) by injection of the posterolateral artery (small arrows). Open arrows indicate the draining vein. Spinal angiograms; sagittal and lateral projections. c On follow-up at 18 months, the AV malformation has been completely obliterated by embolization with PVA particles. Spinal angiograms; AP projection. Fig. 5.3 a, b Endovascular occlusion of an intramedullary cervical AV malformation.






Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree