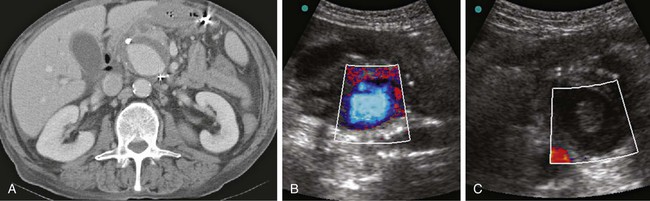
Kenneth R. Thomson, Stuart M. Lyon, Mark F. Given and James P. Burnes Vascular surgery has been the preferred method of treatment, especially if the aneurysm is superficial,1 but more recently, computed tomography (CT) has shown that endoleaks occur in peripheral aneurysms post surgery, just as they do after aortic endovascular repair.2 Recent advances in endovascular methods of treatment and development of new endovascular tools for peripheral aneurysms have made this method a reasonable alternative to conventional surgery. False aneurysms are most common after trauma (including angiographic access). The cause of an aneurysm may be obvious (trauma or iatrogenic) or more obscure (due to atheromatous change, increased flow, or infection), and it may be impossible to determine which type of aneurysm is present based on angiography alone. Multidetector-row CT and Doppler ultrasonography have increased detection of asymptomatic peripheral aneurysms. Aneurysms related to thoracic outlet compression are commonly symptomatic owing to peripheral embolization.3 Permanent occlusion of an aneurysm requires more than just proximal occlusion of the supplying artery. If arterial occlusion is performed, the vessel should be occluded both proximal and distal to the site of the aneurysm to prevent retrograde filling of it via collateral vessels. In the case of an abdominal pseudoaneurysm (e.g., splenic artery pseudoaneurysm) in an unstable patient, proximal arterial occlusion may provide equivalent results to the more conventional segmental occlusion.4 In general, false aneurysms, particularly those caused by an arterial puncture, are more likely to be associated with pain than true aneurysms. Early treatment of false aneurysms is important to reduce the risk of rupture. Factors that influence rupture of cerebral aneurysms are disturbed flow patterns, small impingement regions, and narrow jets.5 The same factors probably apply in peripheral aneurysms. Patients with aneurysms related to arteritis should ideally be treated until the erythrocyte sedimentation rate and other inflammatory markers are within normal range and the etiologic disease is under control, if this is possible. However, aneurysms related to Behçet disease are more likely to arise suddenly and are prone to early rupture.6 • Micropuncture access kit (Cook Inc., Bloomington, Ind.; AngioDynamics Inc., Queensbury, N.Y.) • 0.035-inch guidewire (1.5-mm J or Terumo guidewire [Cook Inc.; Terumo Corp., Somerset, N.J.]) • 5F access sheath (Cook Inc.) • 4F or 5F diagnostic catheter (Cobra 2) (Cook Inc., AngioDynamics Inc., Terumo Corp.) • Guide catheters (Cordis Corp., Hialeah, Fla.; Abbott Vascular, Santa Clara, Calif.) • Microcatheter (Terumo Progreat or equivalent) • Ultravist 370 or equivalent nonionic contrast media • Arterial stent (balloon-expandable or self-expanding), provided the interstices of the stent allow passage of a catheter • Peripheral endograft (Symbiot [Boston Scientific, Natick, Mass.], Atrium [Atrium Medical, Hudson, N.H.], Jo-Graft [Abbott Vascular, Abbott Park, Ill.]) • Balloon angioplasty catheter for use with vinyl alcohol copolymer (Onyx [ev3/Covidien, Irvine, Calif.]) • Occlusion coils (fiber coils are preferred in 0.018- or 0.035-inch wire diameters [Cook Inc., Boston Scientific]) • Detachable coils (Micro Therapeutics Inc. [Irvine, Calif.], Cook Inc., Boston Scientific) • Vinyl alcohol copolymer (Onyx) • N-butyl cyanoacrylate (NBCA) adhesive and iodized oil (Cordis Corp.) • Thrombin (USP), 1000 IU/mL or 5000 IU/5 mL (Thrombin-JMI [GenTrac Inc., Middleton, Wis.]) Approach to the aneurysm will be determined by its site. If the aneurysm cannot be accessed angiographically, it may be possible to directly puncture it using a 22-gauge needle. Of the visceral aneurysms, splenic artery aneurysms are the most common.7 There are several methods of treating peripheral aneurysms. The concept of this procedure is that introducing a small amount of thrombin into the aneurysmal sac will induce a rapid and localized coagulation cascade that will be confined to the aneurysm and not lead to any thrombosis or distal embolization within the native vessel (Fig. 41-1).
Endovascular Treatment of Peripheral Aneurysms
Indications
Contraindications
Equipment
Technique
Anatomy and Approaches
Technical Aspects
Thrombin Injection Into a False Aneurysm
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Endovascular Treatment of Peripheral Aneurysms