Fig. 15.1
EHF complicated by cerebral edema. (a, b) Plain CT scanning demonstrates symmetric density decrease in the cerebral white matter of cerebral hemispheres
Case Study 1
A male patient aged 25 years complained of fever, chills, headache, orbital pain, nausea, vomiting, and decreased volume of urination with no known causes for 4 days. He was then hospitalized. By physical examination, his body temperature was 38.5 °C and he had bulbar conjunctival congestion of both eyes, hemorrhagic spots in the skin of anterior chest, and bilateral renal percussive pain. By laboratory tests, WBC was 14.6 × 109/L, Scr was 621.5 μmol/L, and BUN was 13.6 mmol/L. At day 6 after hospitalization, he experienced sudden convulsion. And CT scanning defined the diagnosis of cerebral edema.
15.7.1.2 Cerebral Hemorrhage
CT scanning is the examination of choice for the clinically suspected cases of EHF complicated by intracranial hemorrhage. Intracerebral hematoma is demonstrated by CT scanning as round- or oval-shaped evenly high-density lesion in the brain parenchyma with surrounding edema, well-defined boundary, and space-occupying effect (Fig. 15.2). Intracerebral hematoma is demonstrated by MR imaging as long T1 long T2 signals in the hyperacute stage, equal T1 short T2 signals in the acute stage, short T1 long T2 signals in the subacute stage, and long T1 long T2 signals in the chronic stage.
Fig. 15.2
EHF complicated by cerebral hemorrhage. (a) Plain CT scanning demonstrates hemorrhage in the left thalamus and peripheral edema. (b) Reexamination by CT scanning after 20 days demonstrates absorption of hematoma
Case Study 2
A male patient aged 25 years complained of chills, fever, headache, lower back pain, orbital pain, nausea, vomiting, and decreased volume of urination with no known causes for 2 days. He was then hospitalized. By CT scanning, the diagnosis was defined to be intracerebral hemorrhage.
15.7.1.3 Subarachnoid Space Hemorrhage
CT scanning is the examination of choice for the diagnosis of subarachnoid space hemorrhage, which is demonstrated as increased density in the cerebral sulcus, fissures, and cistern (Fig. 15.3). MR imaging tends to misdiagnose acute subarachnoid space hemorrhage. T1WI demonstrates high signals in cases of subacute subarachnoid space hemorrhage, while T2WI demonstrates low signals in cases of chronic subarachnoid space hemorrhage.
Fig. 15.3
EHF complicated by subarachnoid space hemorrhage. (a, b) Plain CT scanning demonstrates high-density hemorrhagic foci in the suprasellar cistern, lateral fissure cistern, ambient cistern, and cerebral sulcus
Case Study 3
A male patient aged 22 years complained of aversion to cold, fever, and oliguria for 8 days with accompanying headache, lower back pain, orbital pain, nausea, and vomiting. After he was hospitalized, by physical examination, his body temperature was 39.6 °C and he had drunken-like appearance, bulbar conjunctival congestion of both eyes, subaxillary hemorrhagic spots, and bilateral renal percussive pain. At day 4 after the hospitalization, he experienced convulsion and meningeal irritation sign. By laboratory tests, WBC was 12.4 × 109/L, Scr was 450 μmol/L, and BUN was 32.7 mmol/L. By CT scanning at day 5, the diagnosis was defined as subarachnoid space hemorrhage.
15.7.2 Respiratory System
15.7.2.1 Lung Congestion
Pulmonary congestion mainly occurs in the febrile stage. X-ray demonstrates enlarged hilar shadow; thickened, increased, and deranged lung markings; as well as excessively decreased transparency of the lung field. CT scanning demonstrates enlarged hilum in both lungs, thickened and twisted pulmonary arterial branch, and ground-glass opacity of the lung field. In addition, rare patients are demonstrated with pleural thickening.
15.7.2.2 Pulmonary Edema
Interstitial pulmonary edema mainly occurs in the terminal febrile stage and the hypotensive shock stage. X-ray demonstrates enlarged hilar shadow, thickened and blurry pulmonary vascular branches, excessively decreased transparency of the lung field, and spots or flakes of ground-glass shadows distributed unevenly and asymmetrically in both lungs. There are also nodular cuff sign, reticular shadow, interlobular septal line and cord-like shadows, enlarged heart shadow, as well as blunt costophrenic angle. In cases with aggravated pulmonary vascular lesions, pulmonary alveolar edema can be found mainly in the hypotensive shock or oliguria stage. X-ray demonstrates enlarged intrapulmonary shadows distributed symmetrically with the hilum as the center, which extend into the lung field of both lungs with decreased coloring and excessively decreased transparency of lung fields (Fig. 15.4). Otherwise, X-ray demonstrates large or small flakes of intrapulmonary shadows confined in only one pulmonary lobe with poorly defined boundary, possibly demonstration of enlarged heart shadow, and increased cardiothoracic ratio. In cases with pericardial effusion, flask-shaped heart shadow is demonstrated while pleural reactions are demonstrated as blunt costophrenic angle. CT scanning clearly demonstrates a small quantity of pleural effusion, pleural thickening, and pericardial effusion as pericardial thickening and liquid density shadow in the pericardium (Fig. 15.5).
Fig. 15.4
EHF complicated by pulmonary edema. (a) X-ray demonstrates symmetrically enlarged hilum of both lungs and large flakes of light and thin cloudy shadows in the medial part of both lower lungs. (b) Reexamination after 7 days demonstrates absorption of most lesions
Fig. 15.5
EHF complicated by pericardial and pleural effusion. (a) X-ray demonstrates enlarged heart shadow in flask-like shape as well as absent right diaphragmatic surface and costophrenic angle. (b) CT scanning demonstrates arch-shaped low-density shadow in the right thoracic cavity as well as pericardial thickening with liquid-like low density
Case Study 4
A male patient aged 46 years complained of fever for 7 days and oliguria for 3 days. He reported a history of contact to rats during field construction work. He experienced typically drunken-like appearance and pinpoint-like hemorrhagic spots in his right armpit. After receiving the therapies for anti-infection, hemostasis, and diuresis for 5 days, his body temperature returned to normal and the volume of urination also returned to normal. By routine urine test, protein was positive (+) and granular cast was also positive (+++). By electrocardiography, no abnormalities were found. By X-ray, there was pulmonary edema. And 7 days later, the disease is completely cured with no lesions detected.
Case Study 5
A male patient aged 32 years complained of fever, cough, and lower back pain for 2 days and was hospitalized. He experienced typically drunken-like appearance and pinpoint-like hemorrhagic spots in the skin of the chest. By physical examination, his body temperature was 39.8 °C. By laboratory tests, urine volume was 1500 ml per 24 h that reaches 6200 ml per 24 h after 5 days, urine protein was positive (++), granular casts were positive, and blood BUN was 10.8 mmol/L.
15.7.2.3 Pulmonary Infection
Pulmonary infection may occur in any stage of EHF, but mostly in oliguria stage and diuresis stage. X-ray and CT scanning demonstrate patches of blurry shadows diffusely distributed along singular or bilateral lung markings. In rare cases, small patches of increased-density shadows are demonstrated, possibly with decreased transparency of both lower lungs and quite even distribution. Their fusion into large flakes can be locally found (Figs. 15.6 and 15.7).
Fig. 15.6
EHF complicated by double pneumonia. (a, b) CT scanning demonstrates multiple small flakes of ground-glass shadows in both lungs
Fig. 15.7
EHF complicated by double pneumonia and double pneumothorax. (a, b) Plain CT scanning demonstrates large flakes and patches of shadows with poorly defined boundaries in both lungs as well as pulmonary area with no lung marking in the lateral part of lung fields in bilateral thoracic cavity
Case Study 6
A female patient aged 24 years complained of aversion to cold, fever, lower back pain, orbital pain, nausea, vomiting, and decreased volume of urination with no known causes for 3 days and she was then hospitalized.
Case Study 7
A male patient aged 52 years was admitted to the hospital due to the complaints of fever, cough, and chest pain for 4 days. He experienced typically drunken-like appearance and pinpoint-like hemorrhagic spots in the skin of the chest. By physical examination, his body temperature was 39.2 °C, and he had drumlike sounds in bilateral thoracic cavity by auscultation. By laboratory tests, the volume of urination was 1250 ml that reached 4300 ml after 5 days, urine protein was positive, granular casts were positive, and BUN was 10.2 mmol/L.
15.7.2.4 Pulmonary Hemorrhage
X-ray and CT scanning demonstrate diffusely distributed intrapulmonary consolidation shadows with ground-glass density or large flakes of high density (Fig. 15.8).
Fig. 15.8
EHF complicated by pulmonary hemorrhage. (a, b) Plain CT scanning demonstrates patches of shadows with ground-glass-like density in both lungs with poorly defined boundaries
Case Study 8
A male patient aged 45 years complained of fever, headache, and lower back pain for 7 days as well as oliguria for 2 days. After hospitalization, he experienced persistent fever with the highest body temperature of 40 °C, systemic soreness and pain, severe headache, orbital pain, lower back pain, and accompanying cough with bloody sputum.
15.7.3 Digestive System
15.7.3.1 Hepatic and Splenic Changes
Both liver and spleen are the target organs of hemorrhagic fever virus, and the patients with EHF experience different degrees of hepatic and splenic lesions. Ultrasound demonstrates enlarged liver, increased echo from the liver parenchyma, as well as dense, increased, and enhanced light spots. CT scanning demonstrates enlarged and plump liver, diffusively decreased density of the liver parenchyma whose CT value being lower than the spleen, and poorly defined intrahepatic ducts. In cases with complication of intrahepatic hematoma, intrahepatic high-density hemorrhagic lesions can be found, with formation of liquid level and enlarged spleen.
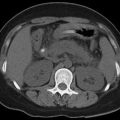
15.7.3.2 Pancreatic Changes
EHF complicated by acute pancreatitis rarely occurs. Pancreatic swelling is commonly caused by pancreatic vascular dilation, congestion, edema, and hemorrhage or occlusive pancreatic duct-induced juice retention due to swelling or compressed epithelial cells of the pancreatic ducts or pancreatic tissues. Pancreas ultrasound demonstrates swollen and enlarged pancreas with enhanced echo from the parenchyma. CT scanning demonstrates swollen and enlarged pancreas with poorly defined boundary. In some serious cases, peripancreatic hematoma can be demonstrated, with increased density in the perirenal fascia and intestinal mesentery. In cases complicated by intrapancreatic hematoma, the lesions are demonstrated with high-density fluid level.
15.7.3.3 Gallbladder Changes
Coarse and thickened gallbladder is commonly caused by hepatic lesions and hypoproteinemia, which commonly coexist with hydrothorax and ascites. Both ultrasound and CT scanning demonstrate irregular thickening of gallbladder wall, even echoes or density in the gallbladder, as well as gallbladder fossa effusion.
15.7.3.4 Gastrointestinal Changes
Gastrointestinal barium meal X-ray demonstrates erosive lesions in the gastric mucosa, linear superficial ulceration, as well as thick and twisted gastric mucosa that is especially obvious in the mucosa of gastric fundus and body. But the more serious lesions are found in the mucosa of the anteroposterior wall of greater curvature.
CT scanning demonstrates even thickening of the gastrointestinal wall with decreased density. In cases with hemorrhage in the gastrointestinal mucosa, the density can be demonstrated with uneven increase and the density of intestinal mesentery can be demonstrated with uneven increase. Some patients may also experience incomplete intestinal obstruction such as intestinal canal dilation and inflation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree