Clinical Presentation
The patient is a 71-year-old female who had a relatively abrupt onset of moderately severe mid and right-sided neck pain, difficulty lifting her right arm, and mild loss of balance. These symptoms began 12 days before presentation. No history of trauma. Patient is taking Coumadin for atrial fibrillation.
Imaging Presentation
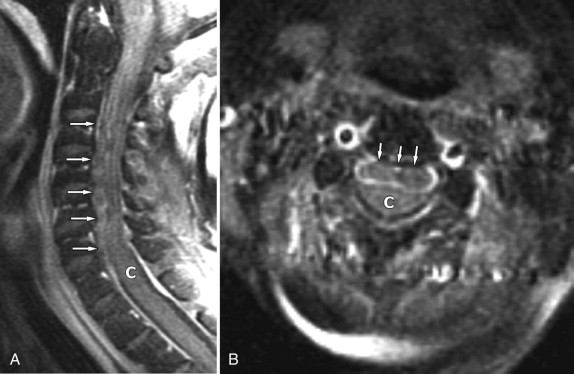
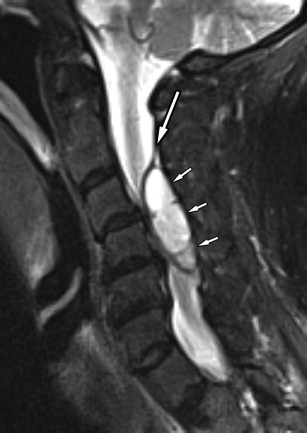
Magnetic resonance (MR) imaging of the cervical spine reveals a heterogeneous epidural fluid collection causing compression of the right posterolateral aspect of the thecal sac and spinal cord from the C3 to C5 level on the right consistent with epidural hematoma ( Figs. 29-1 to 29-3 ) .

Discussion
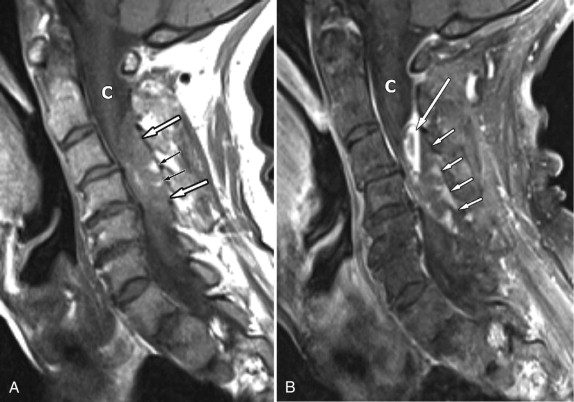
Spinal epidural hematoma (EDH) is a collection of blood that accumulates in the spinal canal outside of the dural sac, usually from epidural venous hemorrhage. EDH most commonly occurs after spinal trauma or surgery and may arise in the anterior or posterior epidural space, but is more common posteriorly in the postoperative setting ( Fig. 29-4 ) . Postoperative epidural hematomas more commonly occur when multilevel spine surgery has been performed or in patients with a coagulopathy. Epidural hematomas may be associated with traumatic or pathologic vertebral fractures as well.
Spontaneous epidural hematomas are those that occur in the absence of trauma or any invasive iatrogenic procedure. Spontaneous epidural hematomas (SEDH) most commonly occur in patients on anticoagulant therapy or patients with a coagulopathy or bleeding diathesis, but can occur secondary to presence of tumor, vascular malformation, epidural hemangioma, or epidural varix. Coughing episodes or Valsalva maneuver also may cause spontaneous epidural hematomas, probably by rupture of epidural veins. There is an increased incidence of epidural hematoma during the third trimester of pregnancy when blood volume is high and engorged veins may be more prone to rupture.
Small epidural hematomas frequently arise adjacent to herniated discs, especially extruded disc fragments, most common in the lumbar region, likely caused by rupture of epidural veins. These small epidural hematomas that may accompany disc extrusions often are overlooked and therefore go unreported. Spinal epidural hematomas may occur in association with epidural metastases, leukemia, and lymphoma. Some have hypothesized that alteration in intracranial pressure may predispose one to spontaneous spinal epidural hematoma development in rare cases. In some cases of spontaneous epidural hematoma, no etiology is found.
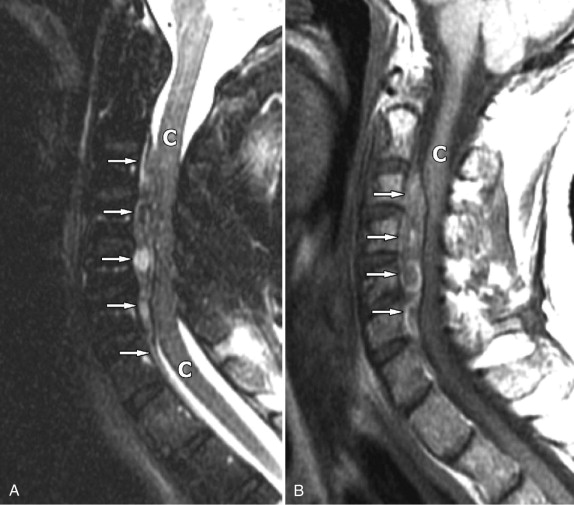
Spontaneous ED hematomas more commonly arise posterior to the thecal sac and are more common in the cervical or upper thoracic region (see Figs. 29-1 to 29-3 ). Spontaneous epidural hematomas can occur in the anterior epidural space as well ( Figs. 29-5 and 29-6 ) .