and Abtin Doroudinia2
(1)
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
(2)
Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Case 4.1
History
A 73-year-old male with history of metastatic gastric carcinoma and peritoneal disease , on chemotherapy. Patient is status post total gastrectomy and splenectomy.
Findings
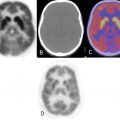
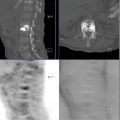
Review of images demonstrates a large hypermetabolic mass in the left mid to upper abdomen at the site of multiple surgical clips with SUVmax of 10.0 (Fig. 4.1). A hypermetabolic mesenteric focus in the mid abdomen inferior to the left hepatic lobe demonstrates SUVmax of 5.3 is identified (Fig. 4.2). Focal activity along the medial aspect of colon in the right lower quadrant is compatible with serosal involvement with SUVmax of 4.1 (Fig. 4.3). Focal FDG activity at the presacral area likely represents a hypermetabolic iliac lymph node with SUVmax of 8.4 (Fig. 4.4). Correlation of the areas with increased PET activity with specific anatomic locations was difficult due to the complete lack of intraperitoneal fat causing poor definition of intra-abdominal structures.
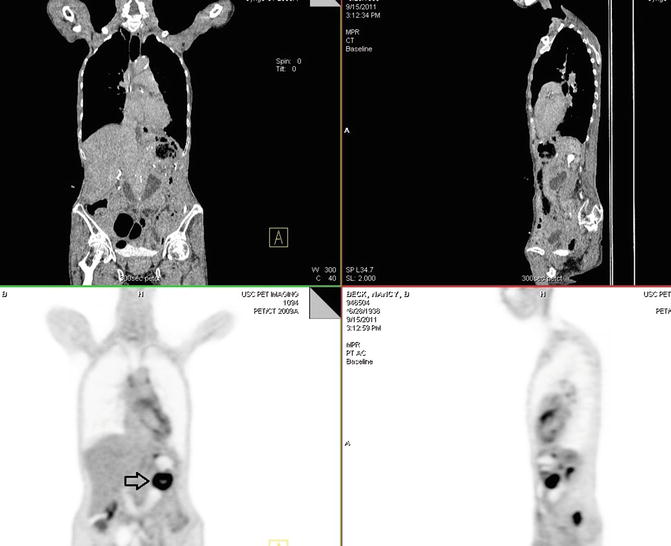
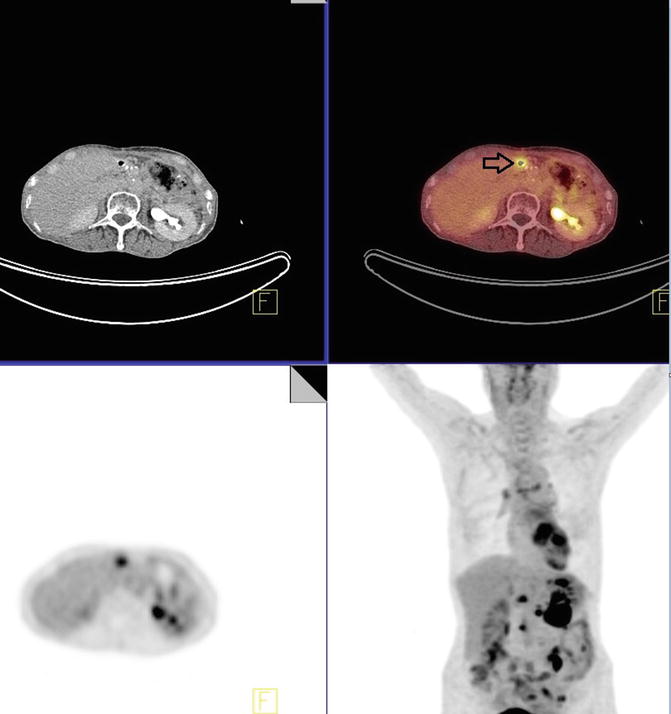
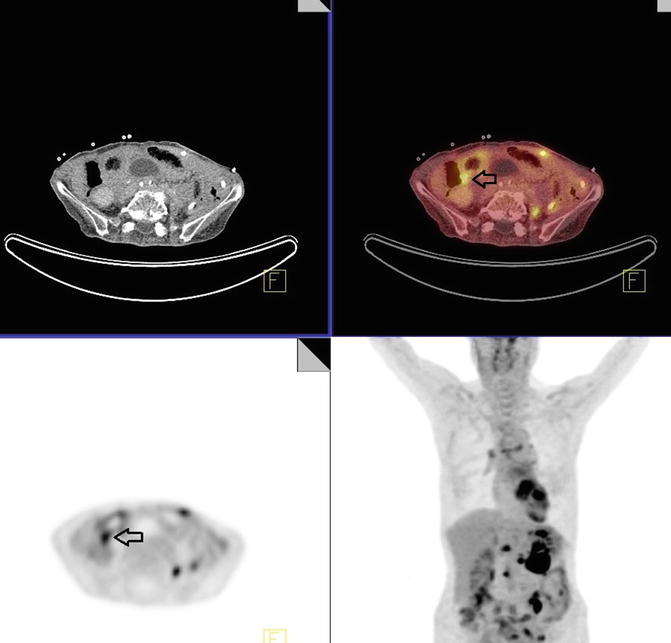
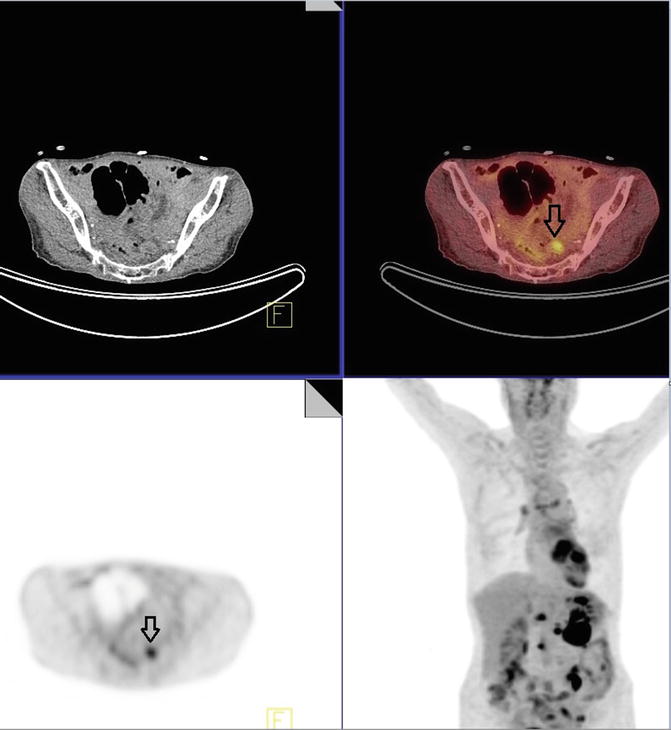
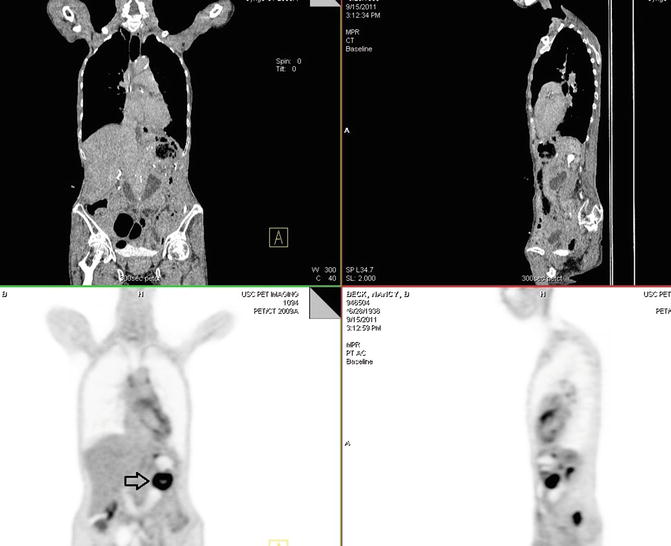
Fig. 4.1
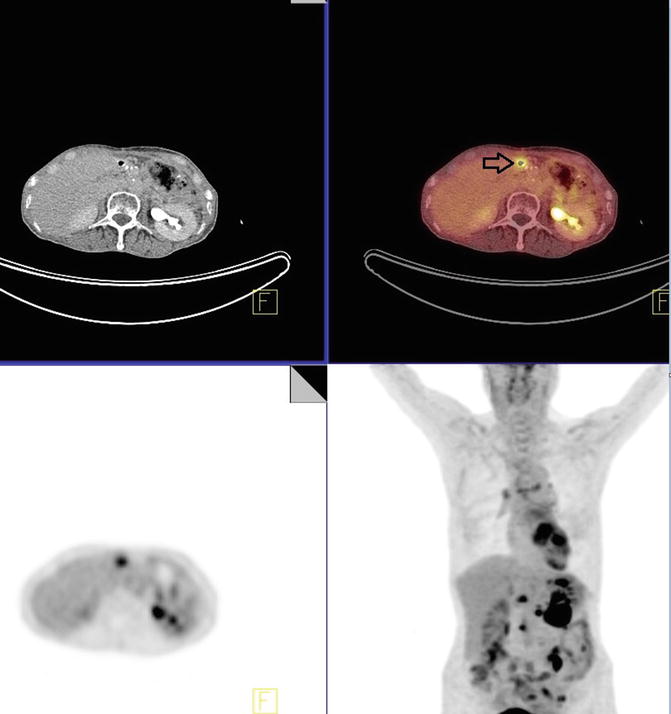
Fig. 4.2
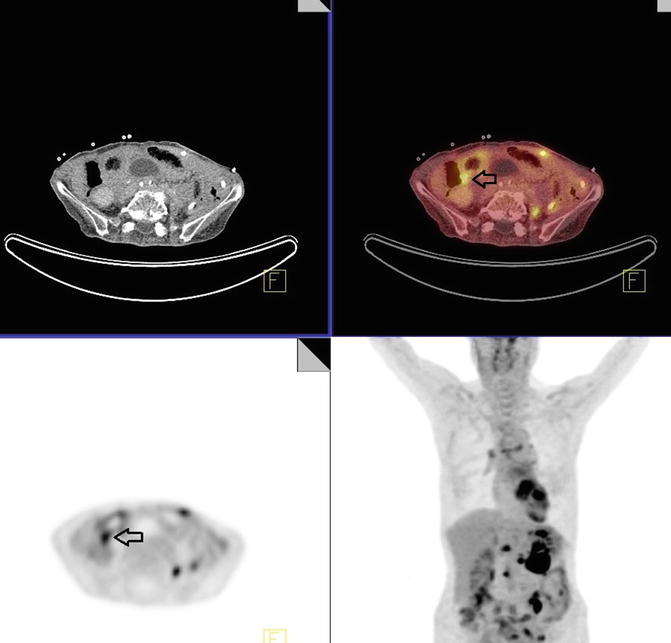
Fig. 4.3
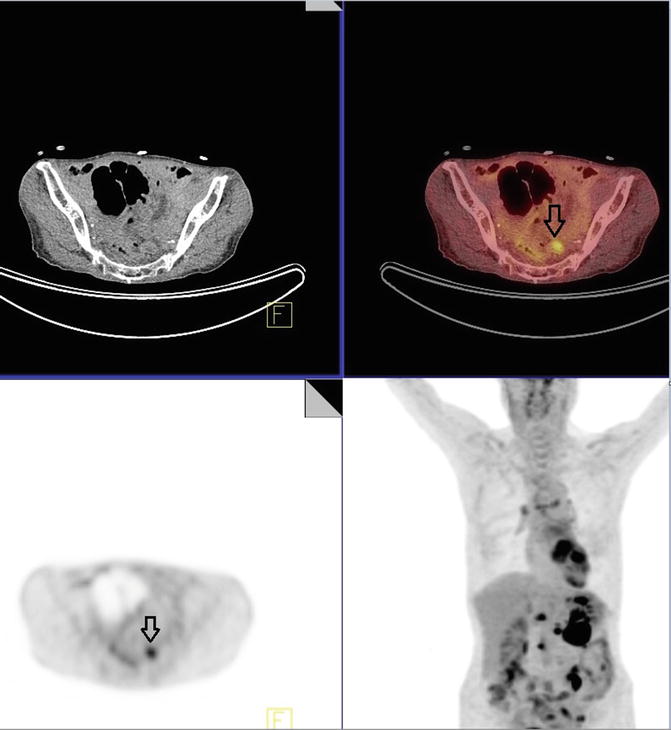
Fig. 4.4
Impression
1.
Multiple hypermetabolic peritoneal and mesenteric metastatic disease
2.
Pelvic nodal metastatic disease
Pearls and Pitfalls
1.
FDG PET may be useful in evaluation of recurrent gastric cancer as well as detecting distant metastatic disease
2.
Staging of gastric cancer with FDG PET scanning will alter the clinical management in patients with recurrence and complement standard staging methods such as laparoscopy, which are more effective at staging local nodal spread and peritoneal disease
Discussion
Gastric cancer is one of the most prevalent cancers worldwide and is a leading cause of cancer mortality. Complete resection of gastric cancer is the only method of achieving permanent control. However, surgeries can be morbid and futile in patients who have advanced disease, making appropriate staging and characterization of disease burden of paramount importance.
The value of PET-CT has been of increasing interest among clinicians and increased its use in the detection, staging, and management of a variety of malignancies. During and after therapy, PET-CT may be useful in determining response to chemotherapy. It may be helpful for restaging and diagnosing recurrence at an earlier time or with greater certainty.
Case 4.2
History
A 53-year-old male patient with submucosal squamous cell carcinoma of the esophagus, status post thoracic laparoscopic esophagectomy with gastric pull-up.
Findings
A hypermetabolic mass measuring 4 × 4.1 × 4.2 cm with SUVmax 19.9 in the proximal esophageal anastomosis is identified. There were no enlarged or hypermetabolic hilar, mediastinal, or axillary lymph nodes (Fig. 4.5).
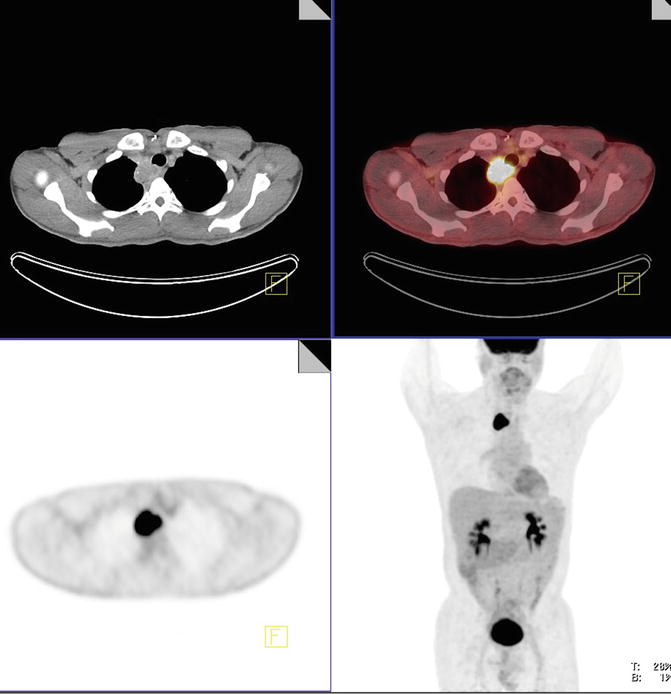
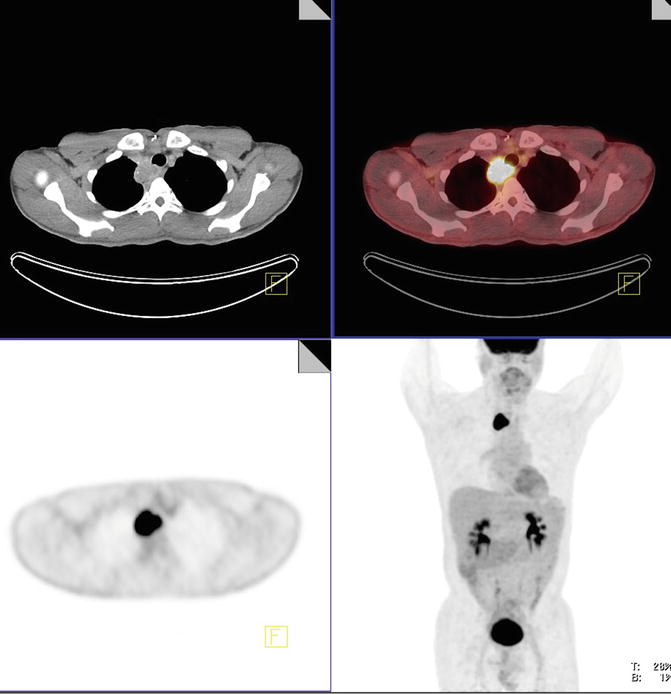
Fig. 4.5
Impression
1.
Hypermetabolic mass at the proximal esophagogastric anastomotic site, consistent with locally recurrent disease
2.
No nodal or distant metastatic disease
Pearls and Pitfalls
1.
Sensitivities for FDG PET imaging are between 91 and 100 %. False-positive uptake can occur due to inflammation, and there can be normal mild FDG activity from muscular contractions.
2.
Accuracy of FDG PET in the staging of regional lymph node metastases ranges from 24 to 90 %. The major limitation of FDG PET with regard to the detection of nodal metastases adjacent to the primary tumor is its relatively poor spatial resolution (approximately 6 mm for a dedicated PET scanner) which reduces sensitivity. The level of metabolic activity and pattern of mediastinal and hilar lymph nodes as well as coexisting nodal calcification is helpful in determining inflammatory versus metastatic etiology.
3.
Recurrence is most common near the esophagogastric anastomosis.
Discussion
Because esophageal cancer is associated with unfavorable prognosis, proper assessment of primary tumor and regional/distant metastasis is necessary for treatment selection and follow-up planning. The depth of invasion and presence of lymph node metastasis are independent prognostic variables in esophageal cancer. Open esophagectomy with comprehensive lymph node dissection is the most accurate method for pathologic staging as well as the most common treatment method for esophageal cancer. However, this operation is frequently associated with significant morbidity, and a mortality rate from experienced institutes is reported in the range of 6–7 %. There are several noninvasive staging methods for esophageal cancer. Endoscopic ultrasound (EUS) and 18F-FDG PET have recently shown good results for clinical staging in esophageal cancer. The degree of 18F-FDG uptake in the primary tumor presenting as the standardized uptake value (SUV) is associated with prognosis in esophageal cancer.
Case 4.3
History
Patient with invasive well-differentiated adenocarcinoma of the distal esophagus.
Findings
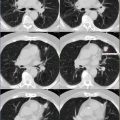
There is a hypermetabolic distal esophageal circumferential thickening with SUVmax of 17.4, consistent with biopsy-proven tumor (Fig. 4.6). There are subcentimeter subcarinal and right hilar nodes with SUVmax of 3.3 and 2.9, respectively. Constellation of latter findings is most suggestive of granulomatous disease by pattern. There was also an AP window node with SUVmax of 4.5, measuring 6 mm (white arrow), also more suggestive of inflammatory (likely granulomatous disease) than malignant etiology (Fig. 4.7). There are several subcentimeter mediastinal nodes with no PET activity but below PET resolution. No enlarged or hypermetabolic axillary lymph nodes are identified.
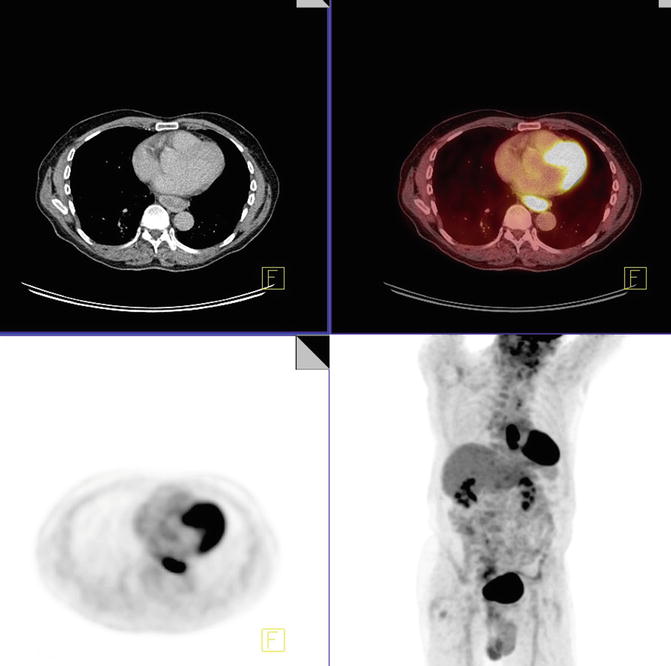
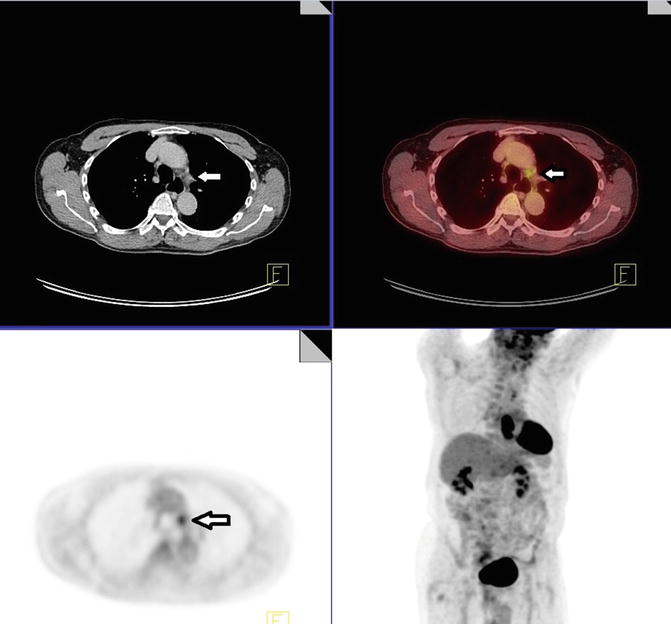
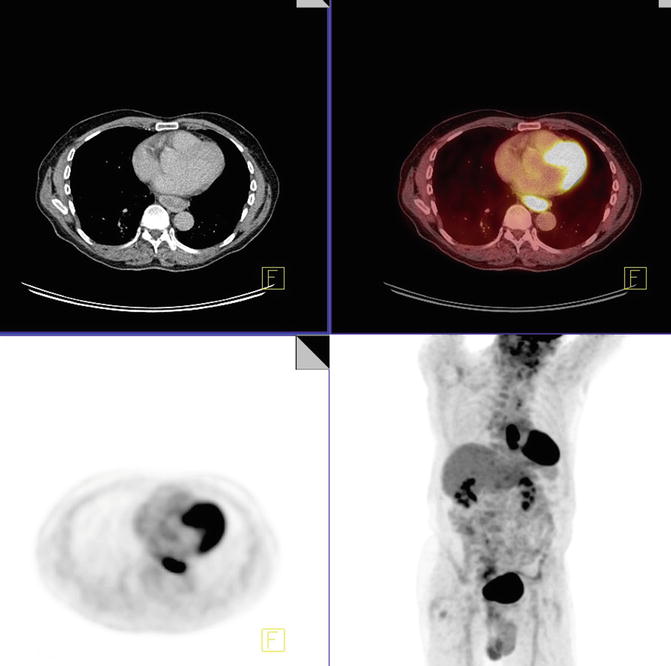
Fig. 4.6
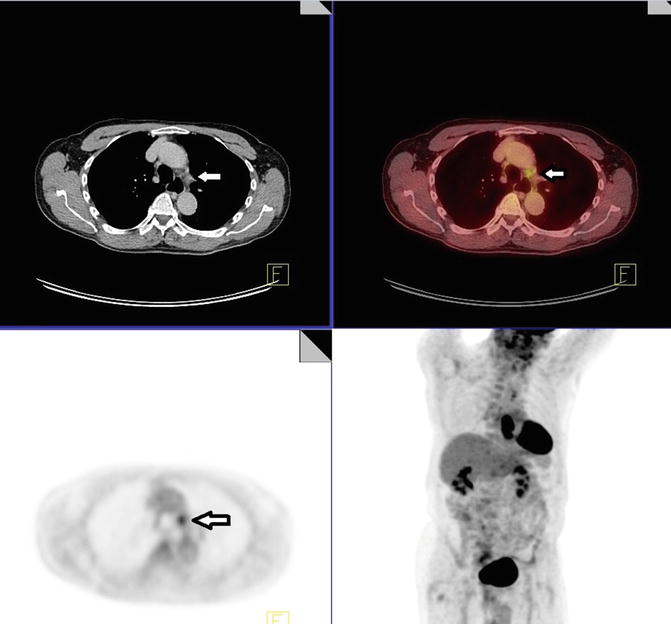
Fig. 4.7
Impression
1.
Hypermetabolic distal esophageal mass consistent with biopsy-proven malignancy
2.
Hypermetabolic mediastinal lymph nodes as noted above
Pearls and Pitfalls
1.
PET is a useful tool for staging in esophageal cancer prior to surgical intervention and has higher accuracy in comparison with CT (88 % versus 65 %).
2.
PET is not sensitive enough to assess local invasion.
3.
Carcinoma in situ and small volume tumors are predisposing factors for false-negative PET.
Discussion
There are two histologic types of esophageal carcinoma that account for the majority of malignant cases: squamous cell carcinoma (>75 to 90 %) and adenocarcinoma. Esophageal cancer tends to be aggressive in its behavior. It invades locally, spreads to local lymph nodes, and then metastasizes throughout the body. Approximately 15 % of esophageal cancers occur in the upper third of the esophagus, 45 % in the middle third of the esophagus, and 40 % in the distal third of the esophagus.
Esophageal carcinoma carries a poor prognosis. Although it is a disease that can be treated, it can rarely be cured. By the time the patient becomes symptomatic, the disease is usually at an advanced stage. The overall 5-year survival rate in patients who undergo surgery ranges from 5 to 20 %, while the 5-year survival rate in patients with lymph node metastases (nonsurgical patients) ranges from 0 to 7 %. Once the diagnosis of esophageal cancer has been made, staging is the next critical step in determining the most appropriate treatment plan for the patient.
Case 4.4
History
Patient with a history of moderate to poorly differentiated adenocarcinoma of the distal esophagus, status post trans-hiatal esophagectomy and gastric pull-up. Patient had biopsy-proven metastatic disease involving the mesentery and liver and was on chemotherapy at the time of imaging.
Findings
There is status post esophagectomy and gastric pull-up with prominent physiologic and/or inflammatory metabolic activity (white arrow) (Fig. 4.8). There are reticular nodular fibrotic changes, predominantly in the lower lungs, suggestive of posttreatment changes (red arrow).
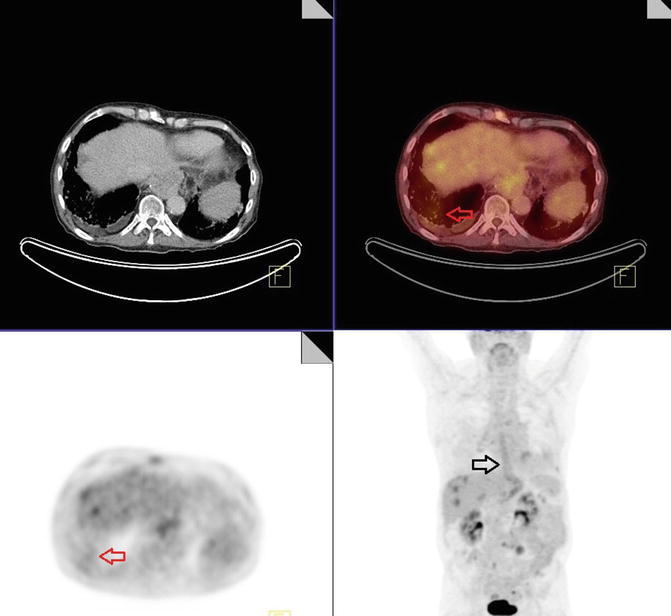
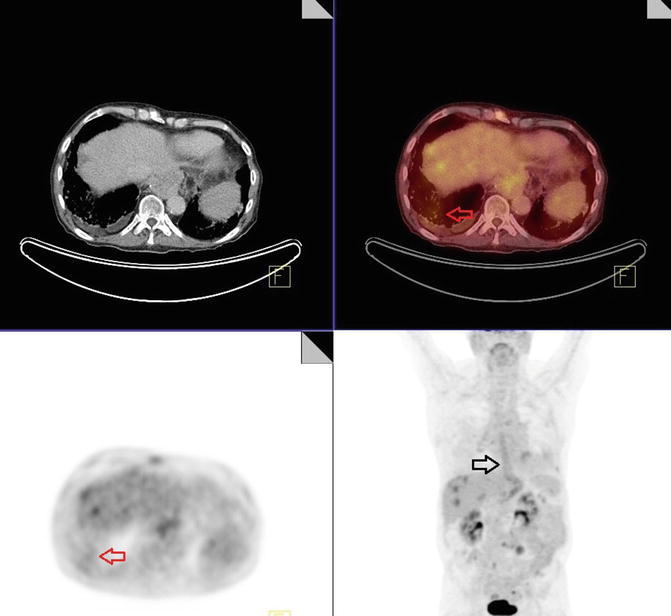
Fig. 4.8
Several metabolic active hypoattenuating hepatic lesions are identified. One of which demonstrates SUVmax of 4.5 in the lateral right lobe; another lesion is seen in the inferior posterior right hepatic lobe with SUVmax of 3.7 (Fig. 4.9).
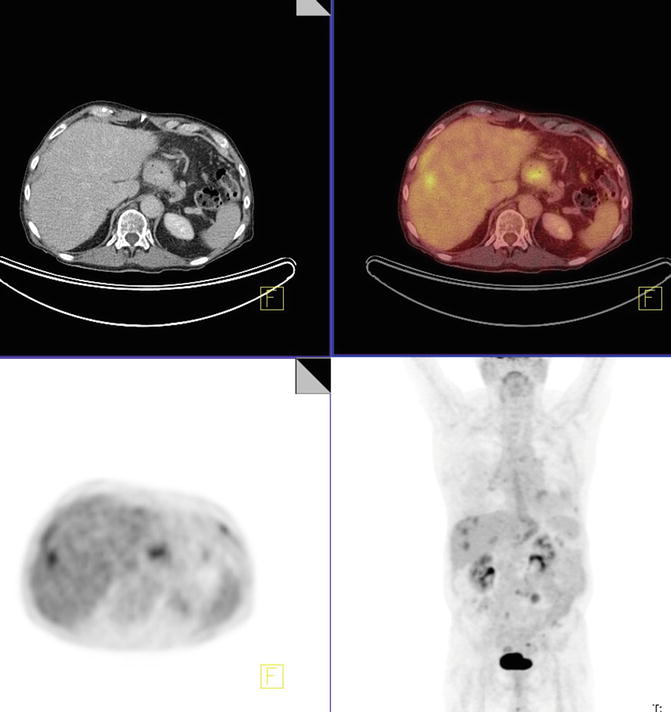
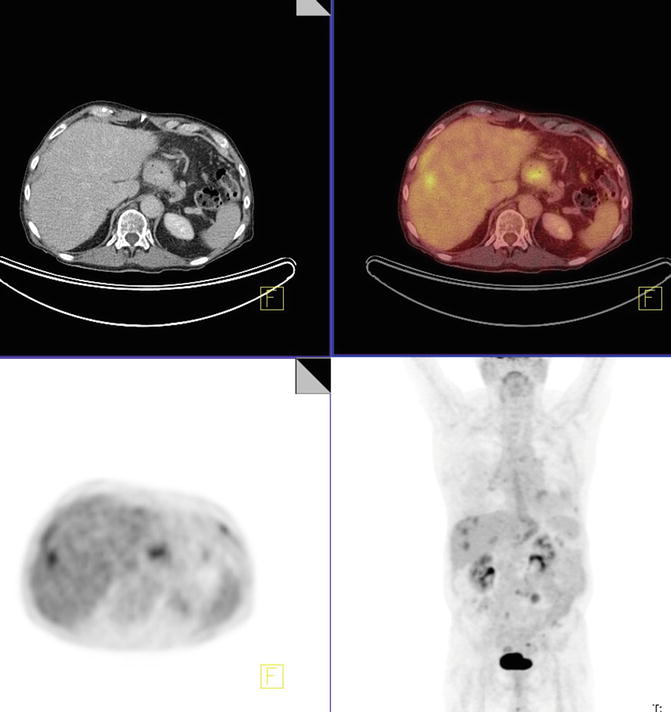
Fig. 4.9
Two hypermetabolic mesenteric nodules are identified that are most consistent with metastatic disease. One of these nodules is at the level of L3–L4 (ventral to third part of duodenum), measuring 2.1 cm with SUVmax of 4.5 (Fig. 4.10).
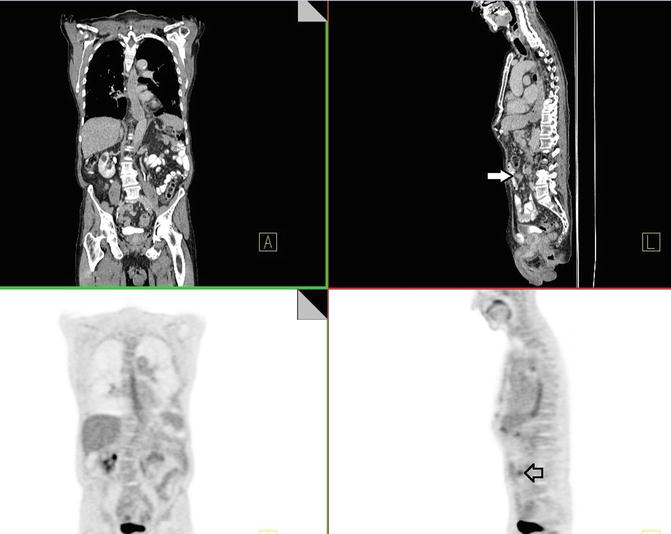
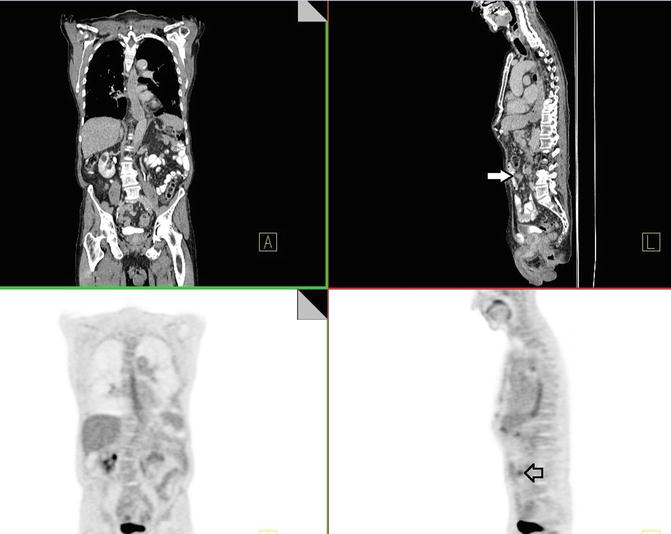
Fig. 4.10
Impression
Enlarged and metabolically active metastatic disease involving mesentery and liver parenchyma.
Pearls and Pitfalls
1.
18F-FDG PET is sensitive and accurate in the preoperative staging of distant metastases in patients with cancer of the esophagus and leads to upstaging.
2.
Though performance of PET in assessing N1 disease is not better than that of current staging methods, there is a significant advantage in detection of M1 disease, avoiding unnecessary surgery.
Discussion
Performance of PET in assessing N1 disease is not better than that of current staging methods. There is a significant advantage in detection of M1 disease, avoiding unnecessary surgery. 18F-FDG PET detects 95 % of the primary esophageal tumors. To identify unsuspected M1 disease, 18F-FDG PET performed better than the combination of CT and EUS. The rate of M1 metastases only detected by 18F-FDG PET in conventionally staged tumors is 10–20 %. 18F-FDG PET upstaged the disease in about 20 % as M1 disease. The accuracy of 69 % for detecting M1 disease with CT and EUS increased to 86 % when combined with 18F-FDG PET.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree