Fig. 23.1
Esophagography. Metal markers were implanted endoscopically as landmarks for tumor location in the esophageal wall close to the proximal edge of the primary tumor
Three-dimensional treatment planning with 5-mm thick CT images was performed using the HIPLAN software program [8]. Gross tumor volume (GTV) was defined as the primary tumor and pathologic lymph nodes (LNs) based on pretreatment staging examinations. The initial planning target volume (PTV) included the GTV and the node regions according to tumor location. The reduced PTV included the whole primary tumor with a 3-cm margin in the cranio-caudal direction and metastatic LNs with a minimum 1-cm margin. A respiratory gating system was used during acquisition of the CT images and during treatment [9]. The beams were delivered in combination with anterior and posterior opposed portals (Fig. 23.2).


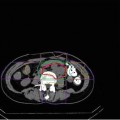
Fig. 23.2
Dose distribution. The beams were delivered in combination with anterior and posterior opposed portals. High-dose area was concentrated around the esophagus
In terms of adverse events in some organs, special attention is required in the treatment planning. Spinal cord should not be included in the area of the dose exceeding 25 GyE to avoid nerve damage. In addition, the portion of the heart included in the high-dose area should be as small as possible to avoid severe adverse events, especially when treating tumors of the middle or lower thoracic esophagus.
23.4.2 Results of Carbon-Ion Radiotherapy for Esophageal Carcinoma
The first phase I/II clinical trial was carried out as a dose-escalation study of short-course preoperative C-ion RT for resectable esophageal carcinoma between July 2004 and June 2008. Then, the second phase I/II clinical dose-escalation study of definitive irradiation for early-stage esophageal carcinoma was started in April 2008 and is currently ongoing.
23.4.2.1 Short-Course Preoperative Carbon-Ion Radiotherapy (Protocol 0301)
Thirty-one patients with stage I–IVa, excluding T4, esophageal squamous cell carcinoma were enrolled in this study [10]. C-ion RT was administered in 8 fractions over 2 weeks. The total radiation dose was escalated from an initial dose of 28.8 GyE in 5 % increments up to 36.8 GyE. Four to 8 weeks after the completion of C-ion RT, esophagectomy and lymph node (LN) dissection were performed. All patients were followed for 36 months or more after surgery.
Toxicity was classified in accordance with the criteria of the Common Terminology Criteria for Adverse Events version 3.0 (CTCAE v 3.0) [11]. Clinical and pathological evaluation of the primary tumor was performed according to the Japanese classification of esophageal cancer (ninth edition) [12].
Toxicities
All observed toxicities are listed in Table 23.1. None of the patients except one case (3.2 %) showed grade 3 or greater toxicities. One case (3.2 %) treated with 35.2 GyE presented grade 3 postoperative acute respiratory distress syndrome (ARDS). However, the correlation between C-ion RT and ARDS was uncertain.
Table 23.1
Toxicity (National Cancer Institute Common Terminology Criteria for Adverse Events version 3)
Acute toxicity (grade) | Late toxicity (grade) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
0 | 1 | 2 | 3 | 4 | 0 | 1 | 2 | 3 | 4 | |
Esophagus | 0 | 19 | 12 | 0 | 0 | |||||
Skin | 4 | 27 | 0 | 0 | 0 | 28 | 0 | 0 | 0 | 0 |
Respiratory | 30 | 0 | 0 | 1 | 0 | 28 | 0 | 0 | 0 | 0 |
Blood | 25 | 4 | 2 | 0 | 0 | 28 | 0 | 0 | 0 | 0 |
Antitumor Effects
In total, 12 of the 31 patients achieved a clinically complete response (CR) (Fig. 23.3), 13 patients achieved a partial response (PR), and the overall response rate (CR + PR) was 80.6 %. According to the tumor depth, all 12 cases with T1 and all 8 cases with T2 achieved CR or PR (response rate, 100 %), while only 5 of the 11 cases with T3 disease achieved CR or PR (response rate, 45.5 %).
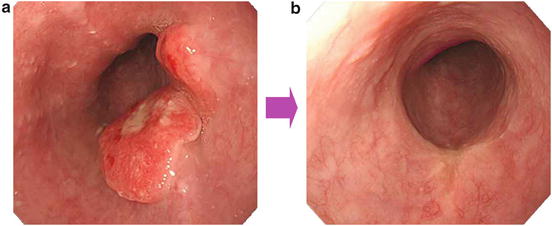
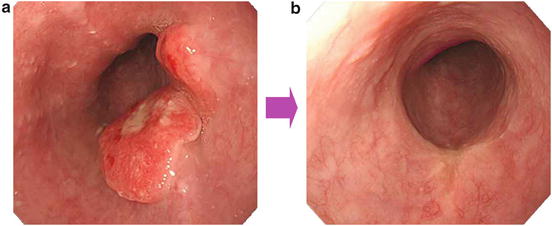
Fig. 23.3
A case with complete response to C-ion RT. The tumor also disappeared pathologically. (a) Before treatment. (b) After carbon-ion irradiation
The pathological response in the resected primary tumor after surgery is shown in Fig. 23.4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree