She’s a little embarrassed. And she’s more than a little nervous. She saw a spot of blood in her bra. Does she have cancer? Her mammogram last month was normal, so everything must be fine.
Don’t let this make you nervous. Figuring out who has concerning versus benign discharge is actually pretty straightforward. One of the most helpful things you can do now is go talk with her and examine her. Ask her to show you the discharge. With a few questions, you can usually tell whether she needs reassurance or imaging. (P.S. The mammogram is almost always normal.)
In a typical history for worrisome discharge a woman notices a spot of blood in her bra or a wet spot on her nightgown upon awakening. Worrisome discharge is usually unilateral, but can occur in women with preexisting bilateral benign nipple discharge. It may occur only once or a few times and seem to resolve. A typical history for benign nipple discharge is discharge that is expressed or occurs during mammographic compression and can be any color except bloody. A warm bath or shower relaxes the smooth muscle in the nipple, so discharge that only appears following bathing is not considered spontaneous and is usually benign.
Discharge that is bloody is concerning, but so is serous discharge. If the discharge is yellow or clear, the fluid can be checked for the presence of blood using a urine dipstick. A dipstick that turns green within the first 30 seconds indicates blood products and should be considered a true positive. If you look at the dipstick later, it will eventually turn green due to the lactoferrin that is normally secreted in breast fluid, which is a false positive ( Table 15-1 ).
| POTENTIALLY CANCEROUS | PROBABLY BENIGN |
|---|---|
| Unilateral | Often bilateral |
| Bloody or serous | Yellow, green, black, milky |
| From a single orifice | From multiple orifices |
| Spontaneous | Expressible |
Etiology of Nipple Discharge
Milky discharge (galactorrhea) is not concerning for breast cancer but may be due to a brain tumor—specifically a pituitary prolactinoma. Women with thyroid disorders can also have milky discharge because thyroid-stimulating hormone (TSH) can cross-talk with prolactin. Serum prolactin and TSH should be checked in women with milky discharge. Some medications can also result in milky discharge, including psychotropic medications, such as antidepressants, neuroleptics, and metoclopramide. These medications are dopamine antagonists, which stimulate prolactin production.
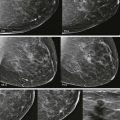
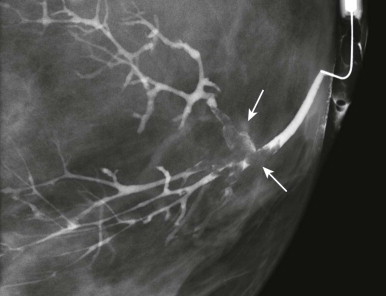
Benign nipple discharge (not milky) ( Fig. 15-1 ) in premenopausal women is most commonly due to fibrocystic change in which cysts communicate with the ducts ( Fig. 15-2 ). In postmenopausal women, duct ectasia is the most common cause. With duct ectasia, the ducts are dilated in the subareolar region and become attenuated more posteriorly ( Fig. 15-3 ).

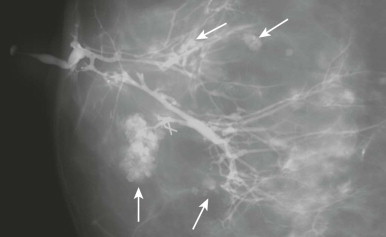
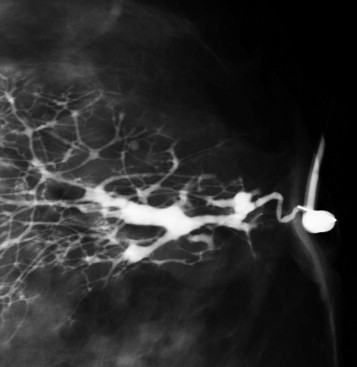
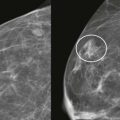
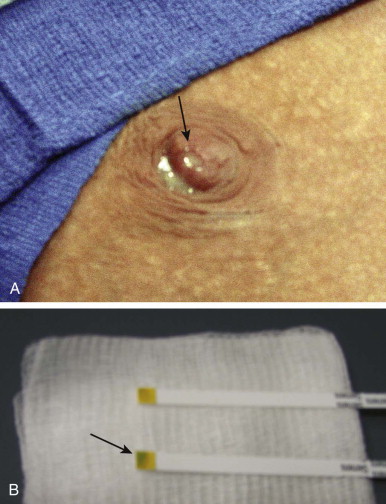
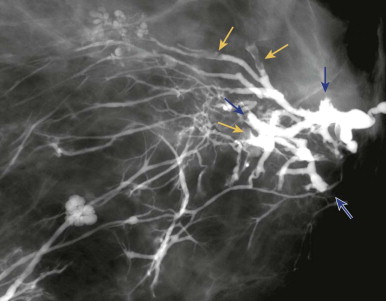
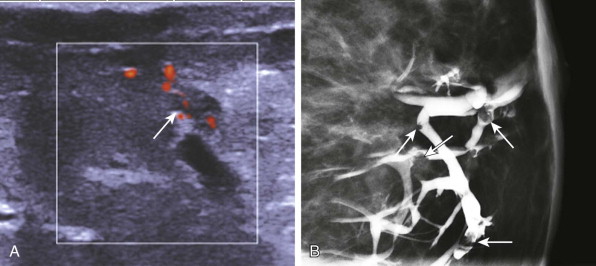
Worrisome discharge ( Fig. 15-4 ) is due to an intraductal papilloma 90% of the time ( Fig. 15-5 ), but is due to ductal carcinoma in situ (DCIS) about 8% of the time ( Fig. 15-6 ). A single intraductal mass near the nipple is most likely to represent a papilloma; however, the imaging appearance is not definitive, and a tissue diagnosis is needed. Multiple intraductal masses (see Fig. 15-6 ) are concerning for DCIS but may be due to papillomatosis or even debris. Trauma (e.g., injury due to a motor vehicle collision), core or surgical biopsy, and cyst aspiration are rare causes of bloody discharge. Occasionally, a cause is not identified.
Evaluating Nipple Discharge
Clinical history and examination are important in order to triage who needs blood work (milky), reassurance (benign), or workup (worrisome). The first question to ask is how the patient noticed the discharge. This will tell you if it is spontaneous or expressible. You will also want to know the color and duration of the discharge, and whether it is unilateral or bilateral. Women should also be asked about medications that could explain milky discharge and whether there is any recent history of trauma.
Mammography may reveal suspicious calcifications indicating DCIS as the cause, but is nearly always negative. Sometimes a solitary dilated duct will correlate with the offending duct. This finding is not very specific, although it becomes more suspicious if it is new or increasing, associated with concerning calcifications, or in a non-subareolar location. Don’t bother with spot compression or magnification views behind the nipple unless an abnormality is suspected on the routine views.
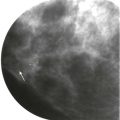
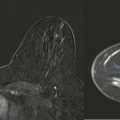
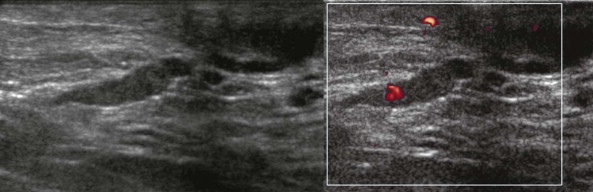
Ultrasound can be very useful for evaluating ductal pathology ( Fig. 15-7 ). The location of the discharging orifice on the nipple can be helpful in guiding the ultrasonography (US) examination. For example, if the orifice is on the lateral aspect of the nipple, it is likely that the abnormal duct system will also be in the lateral breast. If there is a known trigger point—a specific site that elicits discharge on palpation—it can also be used to localize the abnormal duct system. If an intraductal mass is identified on a galactogram, US can be performed to see if the mass is amenable to wire localization using ultrasound guidance. However, US is poor in identifying peripheral intraductal masses ( Fig. 15-8 ), so if the US is negative, additional evaluation will be necessary.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree