Carotid atherosclerosis is an important contributor to ischemic stroke. When imaging carotid atherosclerosis, it is essential to describe both the degree of luminal stenosis and specific plaque characteristics because both are risk factors for cerebrovascular ischemia. Carotid atherosclerosis can be accurately assessed using multiple imaging techniques, including ultrasonography, computed tomography angiography, and magnetic resonance angiography. By understanding the underlying histopathology, the specific plaque characteristics on each of these imaging modalities can be appreciated. This article briefly describes some of the most commonly encountered plaque features, including plaque calcification, intraplaque hemorrhage, lipid-rich necrotic core, and plaque ulceration.
Key points
- •
When imaging carotid atherosclerosis, degree of stenosis and carotid plaque features are the most important findings.
- •
Many high-risk carotid plaque features are detectable on carotid ultrasonography, computed tomography angiography, and magnetic resonance angiography.
- •
Some plaque features are more closely associated with cerebrovascular ischemia than degree of stenosis.
Introduction
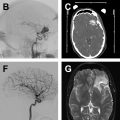
Stroke is a major cause of morbidity and mortality worldwide, with carotid atherosclerosis contributing to a significant proportion of ischemic strokes. , Detailed imaging assessment of extracranial carotid artery disease is critical for the appropriate risk stratification and management of those presenting with cerebrovascular ischemia. When imaging carotid atherosclerosis, the 2 important factors are the degree of luminal stenosis and the assessment of plaque components. Luminal stenosis has been the basis for patient inclusion in multiple randomized stroke prevention trials, and the results of these studies established stenosis severity as the primary imaging-based method for carotid disease risk stratification. However, recent mounting evidence of the contribution of individual plaque components to vulnerable carotid plaque has challenged the primacy of luminal stenosis measures alone as the imaging biomarker of choice for stroke risk assessment. Imaging of luminal stenosis and carotid plaque can be performed with several techniques, including ultrasonography (US), digital subtraction angiography (DSA), computed tomography (CT) angiography, and high-resolution magnetic resonance (MR). Accurate characterization of both luminal stenosis and plaque characteristics is the primary objective of imaging the extracranial carotid artery and is the focus of this review.
Normal anatomy and imaging technique
Most carotid atherosclerotic plaque develops near the bifurcation and proximal internal carotid artery (ICA). Hemodynamic forces and stress play critical roles in the development of atherosclerosis at the carotid bifurcation, in addition to other local and systemic inflammatory and thrombotic processes. The carotid bifurcation is usually between the C3 and C5 levels but can vary slightly in position and may have differing angles among individuals and even among sides in an individual patient.
Carotid Ultrasonography
B-mode US, an inexpensive examination without ionizing radiation, is often the first-line examination to evaluate for carotid stenosis. It is a commonly used screening examination that can indirectly assess the degree of carotid stenosis and evaluate specific carotid plaque features. Limitations of carotid US include its dependence on the sonographer or technologist performing the examination; inherent limitations secondary to patient habitus and anatomy; its flow dependence, which can limit evaluation in the setting of systemic hemodynamic alterations; and inability to discern low levels of stenosis.
In addition to B-mode sonographic techniques, contrast-enhanced US (CEUS) can also be used in the assessment of carotid plaque. In CEUS, sonography is performed after the intravenous injection of microbubble contrast agent, which remains intravascular for the duration of the examination and allows the evaluation of the carotid lumen and plaque neovascularity.
Computed Tomography Angiography
Computed tomography angiography (CTA) of the neck is commonly performed in the acute stroke setting and is an accurate method to evaluate carotid stenosis. CTA is a widely available imaging technique that can be quickly performed without specialized equipment or postprocessing software but still has the ability to directly visualize luminal stenosis and many plaque features. Major considerations with CTA examinations are ionizing radiation and the need to inject intravenous contrast, limiting its use in patients with renal insufficiency. In addition to standard multidetector CTA, dual energy/dual source CT can also be performed to evaluate carotid plaque. Dual energy CT allows improved delineation between calcification associated with a carotid plaque and the increased density from luminal contrast.
Magnetic Resonance Imaging
MR-based imaging is well established for the evaluation of carotid artery plaque. , MR angiography (MRA) can be performed to evaluate the degree of luminal stenosis and to evaluate for additional plaque features that are known to be high risk. MR-based imaging evaluation does not involve ionizing radiation and many sequences can be performed without the administration of intravenous contrast. MR evaluation of carotid plaque is limited because of its often-lengthy imaging acquisition time, higher costs, and individual patient contraindications to MR imaging, such as certain types of cardiac device.
Protocols
Ultrasonography
When evaluating carotid atherosclerotic disease using B-mode US, a 4-MHz to 7-MHz linear array transducer is used to evaluate the distal common carotid arteries (CCAs), the carotid bifurcations, and the cervical ICAs. A complete examination of the carotid arteries includes assessment with gray-scale imaging, color Doppler imaging, and spectral Doppler velocity evaluation. , Peak systolic velocity (PSV) in the ICA along with the presence of plaque are the most important factors in assessing carotid stenosis. Additional Doppler parameters, such as ICA/CCA ratios, can also be used to confirm and/or assist in the diagnosis of carotid stenosis. Power Doppler may be used when there is critical stenosis or near occlusion to evaluate for the presence of any flow.
Computed Tomography Angiography
Multidetector CTA is the most commonly performed type of CTA examination when evaluating cervical vasculature. After the administration of nonionic iodinated contrast using a power injector (4 mL/s flow rate), helical-mode CT scanning with a multidetector scanner is performed. Imaging is performed from the aortic arch to the C1 ring for a neck CTA examination with submillimeter (typically 0.625 mm) resolution. , Sagittal, coronal, and sometimes oblique reconstructions are performed for complete evaluation of the carotid bifurcations. Dual energy CT examinations can also be performed and have been shown to be useful for differentiating calcified plaque from the luminal contrast. At present, dual energy CT is not frequently used in the clinical setting.
Magnetic Resonance Angiography/Magnetic Resonance Imaging
There is more variability in protocols when imaging the cervical vasculature using MR-based techniques. Protocols range from simple, quickly performed noncontrast MRA of the neck to more time-intensive examinations using multiple sequences and dedicated carotid neck coils. All protocols should have at least 1 sequence centered on the carotid bifurcation and extending 3 to 4 cm longitudinally. Most protocols include a time-of-flight (TOF) sequence to assess flow directionality. Contrast-enhanced sequences are also commonly performed in order to more fully assess for stenosis at the origins of the great vessels and vertebral arteries and for more accurate evaluation of luminal stenosis. Many institutions include some kind of sequence with blood suppression to evaluate plaque burden. Often a three-dimensional (3D) T1-weighted sequence, such as MPRAGE (magnetization prepared–rapid gradient echo), is performed to evaluate for intraplaque high-intensity signal, a marker for intraplaque hemorrhage. Either 1.5-T or 3-T scanners can be used, but 3-T scanners have improved signal/noise ratio.
Imaging findings/pathology
There are 2 main findings being imaged with extracranial vascular disease in the carotid artery: luminal stenosis and plaque features. Although luminal stenosis has historically been the focus of imaging, plaque features are becoming increasingly important in the management of patients with carotid artery disease.
Luminal Stenosis
One of the most important findings to report on extracranial vessel imaging is the degree of luminal stenosis. On MRA and CTA, stenosis can be defined by several different measurement techniques, but most commonly by criteria set by the North American Symptomatic Carotid endarterectomy trial (NASCET). , This method requires measurement of the area of the greatest degree of luminal narrowing and then measurement of a nonstenotic region in the normal mid to distal ICA, not in an area where there is poststenotic dilatation ( Fig. 1 ). Although these measurements were initially validated using DSA, there is good correlation with CTA and contrast-enhanced MRA images so measurement is made in a similar fashion. , Other schemes for measuring luminal stenosis are not as commonly used in the United States but include the European Carotid Surgery Trial and common carotid methods of measurement. Luminal stenosis can also be estimated using a technique suggested by Bartlett and colleagues on CTA, in which the narrowest measurement in millimeters is associated with degree of stenosis by NASCET criteria. In this method, 2.2 mm corresponds to a stenosis of approximately 50% and 1.3 mm to a stenosis of 70%.

In contrast, for US, luminal measurements of the area of greatest narrowing cannot be directly made. Instead, the degree of stenosis is inferred based on blood velocity in the ICA and the ratio of PSVs in the CCA and ICA and the plaque burden. US allows a real-time, flow-dependent assessment of stenosis. Issues include any states that can alter the flow, such as aortic stenosis or regurgitation.
Plaque Features
In addition to the degree of luminal stenosis, the plaque composition is also essential to evaluate and discuss. The histopathologic findings in carotid plaque evolution and development have been extensively studied. Atherosclerotic plaque develops along a spectrum from mild fatty deposition in asymptomatic young arteries to complex, irregular plaques prone to releasing thromboemboli. The features identifiable on plaque vessel wall imaging are correlates to histopathologic features. Many plaque characteristics have a typical appearance on each of the most frequently performed imaging modalities ( Table 1 ). Some of the most commonly encountered plaque features on routine imaging are reviewed here.
| Plaque Feature | Definition/Histopathologic Correlate | US Finding | CTA Finding | MR Finding |
|---|---|---|---|---|
| Calcification | Plaque calcification | Echogenic plaque with posterior acoustic shadowing | Plaque with density ≥130 HU | Profound hypointensity on all sequences |
| Intraplaque hemorrhage | Hemorrhagic plaque components | Echolucent plaque | Plaque with low attenuation in the 40–50 HU range | Hyperintense on all T1 and TOF sequences |
| Lipid-rich necrotic core | Necrotic core within lipid-rich plaque that contains macrophages and inflammatory cells | Echolucent plaque | Plaque with low attenuation in the 40–50 HU range | Hyperintense on T1-weighted sequences; isointense on TOF |
| Plaque ulceration | Ulceration of the surface of the plaque leading to exposure of plaque materials to the lumen | Concavity along the surface of the plaque >2 × 2 mm with color Doppler signal within the concavity | Extension of hyperdense contrast beyond the vessel wall into the plaque by at least 1 mm | Surface irregularity on most MR sequences with extension of contrast beyond the lumen wall on MRA |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree