Imaging Presentation
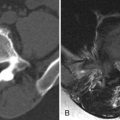
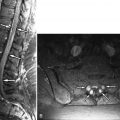
Magnetic resonance (MR) imaging reveals right L4-5 facet hypertrophy and abnormal T2 signal and contrast enhancement in and around the right L4-5 facets compatible with active inflammatory facet arthropathy (facet synovitis) ( Figs. 35-1 to 35-3 ) . Bone scan was initially reported as normal, but reveals minimal increase in activity in the lower lumbar spine on the right ( Fig. 35-4 ) .




Discussion
The zygapophyseal (facet) joints are diarthrodial synovial joints that allow the spine to bend and twist. At any given level, the articular facets are the ovoid surfaces of the inferior and articular processes. Each opposing facet “faces” the joint space, and the facet is composed of a thin layer of dense cortical bone and an overlying layer of hyaline cartilage ( Fig. 35-5 ) . The facet joint contains a small amount of fluid normally and is lined by a thin layer of synovium. Synovial lined joints are contained by a fibroelastic capsule. The facet joint capsule is comprised of two layers, an outer fibrous layer made of parallel bundles of collagen and an inner layer of elastic fibers similar to the ligamentum flavum (see Fig. 35-5 ). The facet joint capsule is thicker where it surrounds the inferior portion of the lumbar facet joint compared with the middle and superior portions of the joint. A band of tendinous fibers reinforce the medial portion of the joint capsule. These tendinous fibers are contiguous with the deep layer of the multifidus muscle and run from the posterolateral margin of the lamina at a given level to the posteromedial margin of the lamina one level above.

Nociceptive and proprioceptive nerve endings are found in the facet capsules and in the synovium. The nociceptive endings are found mainly in the middle-lateral and inferior portions of the joint capsule. Normally nociceptors have a high threshold, firing only when subjected to extreme mechanical stress. When the capsule becomes inflamed, these nociceptors are sensitized by inflammation-induced chemicals that cause the nociceptors to fire at a lower threshold. Hence, pain is generated at a lower threshold in the presence of facet capsular and synovial inflammation. Spinal extension tends to constrict the inferior portion of the facet capsule and therefore is likely to elicit more factogenic pain than spinal flexion.
Arthritis may affect any synovial joint and the facet joints are no exception. Osteoarthritis (degenerative joint disease) is the most common arthritic process that affects the facet joints. Facet joints that are oriented in the sagittal plane are more prone to developing osteoarthritis and are commonly associated with degenerative spondylolisthesis. Facet joint osteoarthritis is a common finding associated with low back pain in a community-based practice. The prevalence of lumbar facet osteoarthritis increases with advancing age, is slightly greater in women, and is most common at the L4-5 level, followed by L5-S1 and L3-4.
The transition between a normally aging facet joint and a “degenerated” facet joint is not clearly defined. Multiple etiologic processes interact or may contribute to the end result we know as facet degeneration or osteoarthritis , including age, a genetic predisposition, trauma (acute or repeated microtrauma), metabolic factors, repeated biomechanical stress, and sometimes infection.
The histopathologic events that cause osteoarthritis in any synovial joint are usually cyclic, and if symptoms occur with this process, these tend to be episodic as well. In an active phase, something triggers an inflammatory response within the synovial joint. The synovial lining of the joint becomes inflamed, thickened, and redundant, and the cells in the synovium malfunction resulting in a joint effusion. The inflammation usually extends to involve the adjacent articular capsular tissues and adjacent bone. The capsules and adjacent tissues become inflamed, thickened, and redundant as well. As a result of this process, articular cartilage becomes degraded and erosions develop in the articular cartilage and subsequently in the adjacent bone ( Fig. 35-6 ) .

A reactive inflammatory response occurs in the adjacent bone. Eventually, when the inflammation becomes quiescent, the cartilage and adjacent bone heal to some extent but not completely. The intra-articular effusion may or may not resolve. Erosions in the cartilage and adjacent bones may heal or persist, and the bone enlarges slightly and becomes sclerotic in this reparative phase. Simultaneously, inflammation in the adjacent joint capsules subsides, but the capsules often remain slightly thickened and weakened. When the same process occurs repeatedly over time, the damage to the synovium, facet capsule, and articular facet bone becomes more extensive. Eventually, as a result of this chronic osteoarthritic process, the synovium becomes thickened and redundant, the articular cartilage becomes degraded and thinned, permanent articular and bone erosions occur, and subchondral cysts or geodes form in the articular facets ( Fig. 35-7 ) . The facet capsules become thickened, yet weakened and lax. The chronically inflamed facet joint capsules and adjacent ligamentum flavum become thickened and encroach upon the paraspinal soft tissues, central vertebral canal, and neural foramen (see Fig. 35-7; Fig. 35-8 ). Cystic outpouchings of the facet joints, called synovial cysts, may form. In the late stages of this episodic inflammatory process, the facet joint often becomes unstable resulting in facet subluxation or dislocation. (See Chapter 75 for more discussion of synovial cysts.)


Facet joint effusions form in the active stage of the disease and may persist long after acute inflammation subsides in a chronic degenerated facet joint ( Fig. 35-9 ) . The facet joint fluid may also become replaced by gas (the vacuum facet phenomenon ) ( Fig. 35-10 ) . The facet joint spaces are typically widened when acute or chronic inflammatory effusions are present, but the facet joint space is often narrowed with an undulating, irregular margin in severe chronic facet degeneration ( Fig. 35-11 ) .



As facet hypertrophy becomes pronounced, the hypertrophic bone encroaches upon adjacent structures, contributing to neural foraminal stenosis, central canal stenosis, and lateral recess stenosis. Superior facet hypertrophy is the primary cause of lateral recess stenosis. Facet hypertrophy, along with ligamentum flavum thickening, also contributes to central canal stenosis. Facet hypertrophy tends to encroach upon the lower portion of the lumbar neural foramen initially. Because the lumbar nerve roots are positioned in the superior portion of the neural foramen, severe facet hypertrophy is usually required to cause significant foraminal nerve root impingement. At any given lumbar level, foraminal stenosis is typically caused by disc bulging or protrusion, posterolateral vertebral osteophyte formation and hypertrophy of the superior articular process/facet (see Figs. 35-6 and 35-8 ). The L5 nerve root is the most commonly affected nerve by neural foraminal narrowing secondary to bulging or protruding disc, posterolateral vertebral osteophytes, and facet hypertrophy. The L5 nerve root is also the most common nerve to be affected by lateral recess stenosis. (See Chapter 71 , Chapter 72 for further discussion of spinal stenosis and lateral recess stenosis).
At the same time the osteoarthritic process is occurring in the facets, other degenerative processes are occurring elsewhere in the spine including intervertebral disc degeneration, vertebral osteochondrosis, and spondylosis deformans. Although disc degeneration and vertebral osteophyte formation are considered degenerative processes, osteoarthritis is not causing these other degenerative conditions because the disc is not a synovial joint. Yet these coexistent degenerative processes likely alter the biomechanical stresses placed upon various spinal articulations and as a result may accelerate the degenerative process in these other articulations.
The osteoarthritic process involving the facets described above may be asymptomatic or accompanied by a varying degree of stiffness or pain . Pain accompanying facet osteoarthritis is often related to active inflammation (facet synovitis). It is inflammation that likely sensitizes the nociceptors in the facet capsule and synovium. Facetogenic pain is caused by any stress placed upon the inflamed facet capsule, so facetogenic pain is often worse while sitting or twisting or bending the spine. Facetogenic pain may be referred into the buttocks, groin, or thigh but usually does not extend below the knee, although there are exceptions to this.
Patients with facet joint instability develop vertebral subluxations (spondylolisthesis). Spinal instability is commonly associated with back pain. Degenerative lumbar vertebral spondylolisthesis is most commonly related to facet instability secondary to longstanding facet osteoarthritis at that level of the vertebral subluxation. The facet joints in patients with degenerative spondylolisthesis tend to be oriented in the sagittal plane. When the spine becomes unstable, back pain is often produced as a result of the spinal instability.
Discussion
The zygapophyseal (facet) joints are diarthrodial synovial joints that allow the spine to bend and twist. At any given level, the articular facets are the ovoid surfaces of the inferior and articular processes. Each opposing facet “faces” the joint space, and the facet is composed of a thin layer of dense cortical bone and an overlying layer of hyaline cartilage ( Fig. 35-5 ) . The facet joint contains a small amount of fluid normally and is lined by a thin layer of synovium. Synovial lined joints are contained by a fibroelastic capsule. The facet joint capsule is comprised of two layers, an outer fibrous layer made of parallel bundles of collagen and an inner layer of elastic fibers similar to the ligamentum flavum (see Fig. 35-5 ). The facet joint capsule is thicker where it surrounds the inferior portion of the lumbar facet joint compared with the middle and superior portions of the joint. A band of tendinous fibers reinforce the medial portion of the joint capsule. These tendinous fibers are contiguous with the deep layer of the multifidus muscle and run from the posterolateral margin of the lamina at a given level to the posteromedial margin of the lamina one level above.

Nociceptive and proprioceptive nerve endings are found in the facet capsules and in the synovium. The nociceptive endings are found mainly in the middle-lateral and inferior portions of the joint capsule. Normally nociceptors have a high threshold, firing only when subjected to extreme mechanical stress. When the capsule becomes inflamed, these nociceptors are sensitized by inflammation-induced chemicals that cause the nociceptors to fire at a lower threshold. Hence, pain is generated at a lower threshold in the presence of facet capsular and synovial inflammation. Spinal extension tends to constrict the inferior portion of the facet capsule and therefore is likely to elicit more factogenic pain than spinal flexion.
Arthritis may affect any synovial joint and the facet joints are no exception. Osteoarthritis (degenerative joint disease) is the most common arthritic process that affects the facet joints. Facet joints that are oriented in the sagittal plane are more prone to developing osteoarthritis and are commonly associated with degenerative spondylolisthesis. Facet joint osteoarthritis is a common finding associated with low back pain in a community-based practice. The prevalence of lumbar facet osteoarthritis increases with advancing age, is slightly greater in women, and is most common at the L4-5 level, followed by L5-S1 and L3-4.
The transition between a normally aging facet joint and a “degenerated” facet joint is not clearly defined. Multiple etiologic processes interact or may contribute to the end result we know as facet degeneration or osteoarthritis , including age, a genetic predisposition, trauma (acute or repeated microtrauma), metabolic factors, repeated biomechanical stress, and sometimes infection.
The histopathologic events that cause osteoarthritis in any synovial joint are usually cyclic, and if symptoms occur with this process, these tend to be episodic as well. In an active phase, something triggers an inflammatory response within the synovial joint. The synovial lining of the joint becomes inflamed, thickened, and redundant, and the cells in the synovium malfunction resulting in a joint effusion. The inflammation usually extends to involve the adjacent articular capsular tissues and adjacent bone. The capsules and adjacent tissues become inflamed, thickened, and redundant as well. As a result of this process, articular cartilage becomes degraded and erosions develop in the articular cartilage and subsequently in the adjacent bone ( Fig. 35-6 ) .