Functions
• Special visceral efferent (SVE). Branchial motor innervation to muscles of facial expression (including orbicularis oculi, orbicularis oris, zygomaticus major, levator anguli oris, risorius, depressor anguli oris, mentalis, buccinator, frontalis, occipitalis, corrugator supercilii, and platysma), stapedius, stylohyoid, and posterior belly of digastric.
• General visceral efferent (GVE). Visceral motor (parasympathetic) innervation to lacrimal gland (via greater superficial petrosal nerve; GSPN), oral and nasal mucosa (via GSPN), and submandibular and sublingual glands (via chorda tympani).
• General sensory afferent (GSA). Somatic sensory from external auditory meatus, auricle and retroauricular area
• Special afferent special sensory (SA) for taste from anterior two thirds of tongue and hard and soft palate (via chorda tympani) .
Anatomy
Motor Division
• SVE
• Facial motor nucleus lies in caudal pontine tegmentum, anterolateral to cranial nerve (CN) VI nucleus (Figs. 7.1, 7.2). It sends axons dorsally toward the fourth ventricle; these axons loop around the CN VI nucleus (forming the genu of the facial nerve) and then travel ventrolaterally to emerge from the pontomedullary junction just above CN VIII. The facial colliculus is formed by this genu of the facial nerve and refers to a smooth hump that protrudes into the fourth ventricle.
• Supranuclear control is via corticobulbar fibers from the lower one third of the precentral gyrus via corona radiata, genu of internal capsule, and medial cerebral peduncle to the facial motor nucleus in the pons. Corticobulbar fibers project bilaterally to upper face motor neurons and contralaterally to lower face motor neurons. The peripheral course of CN VII is discussed below.
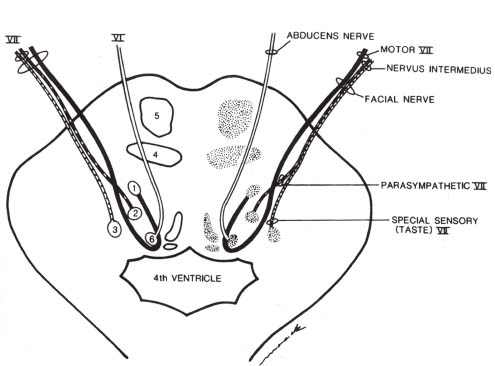
Fig. 7.1 Axial view of the lower pons. The branchial motor portion (solid line) of the facial nerve originates in the motor nucleus (1) in the pontine tegmentum, loops dorsally around the abducens nucleus (6), then turns to exit the ventrolateral pons at the pontomedullary junction. The nervus intermedius carries the parasympathetic fibers (dashed line) originating in the superior salivatory nucleus (2) as well as the special sensory fibers (dotted line) that convey taste information from the anterior two thirds of the tongue to the rostral nucleus solitarius (3). (4, medial lemniscus; 5, corticospinal tract.) (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.]. St. Louis, MO: Mosby, 1995. Reprinted with permission.)
Nervus Intermedius (of Wrisberg)
• GVE, GSA, and SA (parasympathetic, somatic sensory, and special sensory).
• Exits the pons between the motor branch of CN VII (medially) and CN VIII (laterally), traverses the cerebellopontine angle cistern, and enters the internal auditory canal (IAC).
• GVE. The superior salivatory nucleus and associated lacrimal nucleus in the dorsal pons send preganglionic parasympathetic axons to the nervus intermedius and from there to (1) the greater superficial petrosal nerve (GSPN) to the pterygopalatine ganglion to the lacrimal gland and the mucosa of the nose and mouth (palatal and nasal glands); and (2) the chorda tympani nerve that joins with the lingual nerve (CN V3) and goes to the submandibular ganglion and on to the submandibular and sublingual glands for salivation (see below regarding taste function). The olfactory areas and the limbic system send input to the hypothalamus, which influences the superior salivatory nucleus by way of the dorsal longitudinal fasciculus.
• The geniculate ganglion is located in the petrous temporal bone lateral and posterior to the petrous internal carotid artery (ICA), posterior and medial to the foramen spinosum, and anterior to the superior semicircular canal. It consists of sensory nerve cell bodies for taste (from chorda tympani) and external ear sensation (from sensory auricular branch). Motor and parasympathetic fibers of CN VII pass through the geniculate ganglion without synapsing.
• GSA. Sensory information from the external auditory meatus, and the auricle and retroauricular area is carried via the sensory auricular branch to the geniculate ganglion (where cell bodies lie, at the facial genu in the petrous bone) to the nervus intermedius and back to the spinal trigeminal tract and spinal trigeminal nucleus in the medulla.
• SA. See below under Chorda Tympani Nerve.
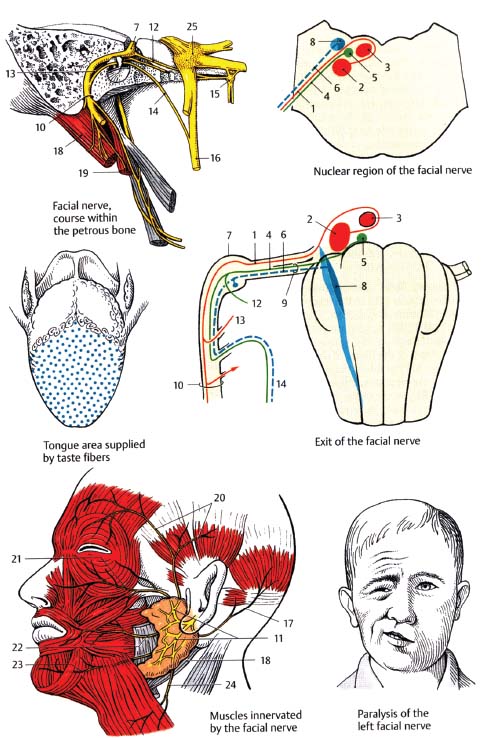
Fig. 7.2 Integrated view of the facial nerve. Motor fibers (1), originate from the motor nucleus (2), arch around the abducens nucleus (3), and emerge at the pontomedullary junction. Parasympathetic fibers (4), originate from the superior salivatory nucleus (5). Special sensory fibers for taste (6), transmit information from the geniculate ganglion (7), to the rostral nucleus solitarius (8). The parasympathetic and sensory fibers together form the nervus intermedius (9). After passing through the internal acoustic meatus and traversing the temporal bone through the facial canal, the nerve exits the skull through the stylomastoid foramen (10), and then ramifies in the parotid gland (11). The GSPN (12), to stapedius (13), and chorda tympani nerve (14), branch within the facial canal. The GSPN traverses the pterygoid canal to the pterygopalatine ganglion (15). The chorda tympani nerve pierces the petrotympanic fissure to join the lingual nerve (16). Other branches include the posterior auricular nerve (17), and branches to the posterior belly of the digastric muscle (18), and to the stylohyoid muscle (19). The parotid plexus gives off temporal branches (20), zygomatic branches (21), buccal branches (22), the marginal mandibular branch (23), and the cervical branch (24). 25, trigeminal ganglion.
Anatomy of Peripheral Course of Facial Nerve
• After emerging from the ventrolateral pons, the motor division and nervus intermedius traverse the cerebellopontine angle cistern with CN VIII and then enter the IAC in the petrous temporal bone, along with the labyrinthine artery and vein (Fig. 7.3). Four intratemporal segments of the nerve are described (Fig. 7.4):
 Meatal (intracanalicular) segment. Within the IAC, the motor division of CN VII is located anterosuperior, the cochlear nerve anteroinferior, the superior vestibular nerve posterosuperior, and the inferior vestibular nerve posteroinferior. The nervus intermedius travels between CN VII and CN VIII at the porus acusticus and then joins CN VII to travel in the anterosuperior quadrant (superior to the crista falciformis and anterior to the Bill bar) (Fig. 7.3).
Meatal (intracanalicular) segment. Within the IAC, the motor division of CN VII is located anterosuperior, the cochlear nerve anteroinferior, the superior vestibular nerve posterosuperior, and the inferior vestibular nerve posteroinferior. The nervus intermedius travels between CN VII and CN VIII at the porus acusticus and then joins CN VII to travel in the anterosuperior quadrant (superior to the crista falciformis and anterior to the Bill bar) (Fig. 7.3).
 Labyrinthine segment. The bony fallopian canal courses anterolaterally from the fundus of the IAC and carries the labyrinthine segment of CN VII to the geniculate ganglion. The GSPN arises from the apex of the geniculate ganglion.
Labyrinthine segment. The bony fallopian canal courses anterolaterally from the fundus of the IAC and carries the labyrinthine segment of CN VII to the geniculate ganglion. The GSPN arises from the apex of the geniculate ganglion.
 Horizontal (tympanic) segment. From the geniculate ganglion, CN VII travels posteriorly and horizontally just inferior to the lateral semicircular canal. No branches arise from this segment of the facial nerve.
Horizontal (tympanic) segment. From the geniculate ganglion, CN VII travels posteriorly and horizontally just inferior to the lateral semicircular canal. No branches arise from this segment of the facial nerve.
 Mastoid (vertical) segment. At the posterior aspect of the middle ear, CN VII turns inferiorly to form the mastoid segment. Three branches arise from this segment of CN VII: the nerve to the stapedius muscle, the chorda tympani nerve (see above), and the sensory auricular branch (innervates external auditory meatus and the auricle and retroauricular area). CN VII then exits the bony facial canal at the level of the stylomastoid foramen and immediately gives off the posterior auricular nerve (to occipitalis, posterior auricular, and oblique auricular muscles), the digastric branch (to the posterior belly of the digastric muscle), and the stylohyoid branch (to the stylohyoid muscle).
Mastoid (vertical) segment. At the posterior aspect of the middle ear, CN VII turns inferiorly to form the mastoid segment. Three branches arise from this segment of CN VII: the nerve to the stapedius muscle, the chorda tympani nerve (see above), and the sensory auricular branch (innervates external auditory meatus and the auricle and retroauricular area). CN VII then exits the bony facial canal at the level of the stylomastoid foramen and immediately gives off the posterior auricular nerve (to occipitalis, posterior auricular, and oblique auricular muscles), the digastric branch (to the posterior belly of the digastric muscle), and the stylohyoid branch (to the stylohyoid muscle).
 CN VII then enters the parotid gland and divides into temporofacial and cervicofacial branches. These then divide into temporal, zygomatic, buccal, marginal mandibular, and cervical branches (TEN ZEBRAS B IT MY CLOCK), which innervate the many muscles of facial expression (listed at beginning of chapter).
CN VII then enters the parotid gland and divides into temporofacial and cervicofacial branches. These then divide into temporal, zygomatic, buccal, marginal mandibular, and cervical branches (TEN ZEBRAS B IT MY CLOCK), which innervate the many muscles of facial expression (listed at beginning of chapter).
 The distribution and functions of CN VII are summarized in Fig. 7.5.
The distribution and functions of CN VII are summarized in Fig. 7.5.
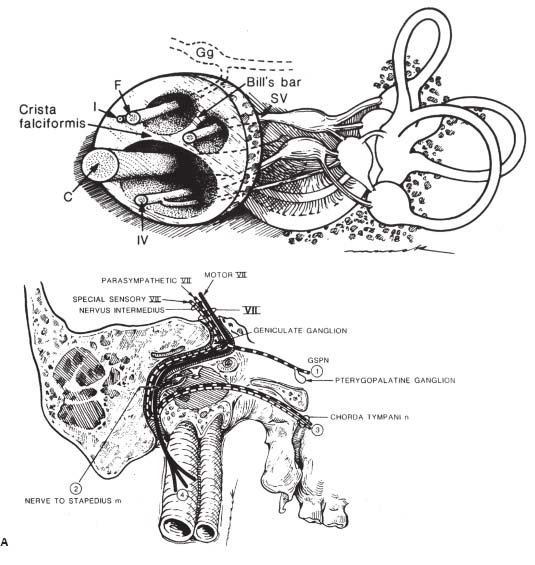
Fig. 7.3 Internal auditory canal. The facial nerve (F) and nervus intermedius (I) are found in the anterior-superior quadrant, the cochlear nerve (C) in the anterior-inferior quadrant, the superior vestibular nerve (SV) in the posterior-superior quadrant, and the inferior vestibular nerve (IV) in the posterior-inferior quadrant. The crista falciformis (falciform crest) is a horizontal bony strut separating the superior and inferior halves of the fundus of the IAC. Bill’s bar is a surgical landmark separating CN VII from the superior vestibular nerve. (Gg, geniculate ganglion.) (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.]. St. Louis, MO: Mosby, 1995. Reprinted with permission.)
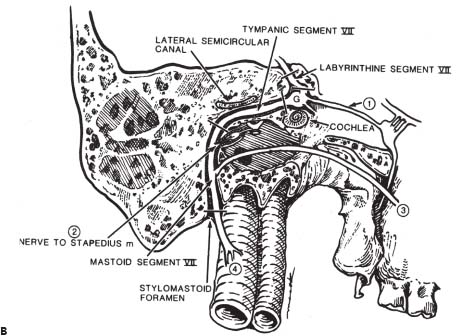
Fig. 7.4 Detailed course of the facial nerve through the temporal bone. (A) The parasympathetic portion (dashed line) branches at the anterior genu to supply the lacrimal gland via the GSPN (1) before continuing as part of the chorda tympani nerve to supply secretomotor function to the submandibular and sublingual glands. Special sensory fibers (dotted line) comprise the majority of the chorda tympani nerve (conveying taste) (3), with cell bodies in the geniculate ganglion. The branchial motor portion (solid line) gives off the nerve to the stapedius muscle (2) before continuing to innervate the muscles of facial expression (4). (B) Segments of the facial nerve within the temporal bone in order: meatal or intracanalicular (not shown), labyrinthine, tympanic (also called horizontal segment), and mastoid (also called vertical segment). (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.]. St. Louis, MO: Mosby, 1995. Reprinted with permission.)
Greater Superficial Petrosal Nerve
• GVE (parasympathetic).
• GSPN arises from the geniculate ganglion, courses anteromedially, and exits the petrous temporal bone via the greater petrosal foramen (facial hiatus) to the middle fossa.
• GSPN passes deep to the trigeminal (gasserian) ganglion in Meckel’s cave and down the foramen lacerum to the pterygoid canal (vidian canal), where it joins with the deep petrosal nerve (sympathetic fibers from ICA plexus; cell bodies in superior cervical ganglion) to form the nerve of the pterygoid canal (vidian nerve).
Nerve of the Pterygoid Canal (Vidian Nerve)
• GVE (parasympathetic) + sympathetic.
• Traverses pterygoid (vidian) canal to the pterygopalatine fossa, where the parasympathetics synapse in the pterygopalatine (sphenopalatine) ganglion.
• Other postganglionic parasympathetics travel with other CN V2 branches (nasal and palatine nerves) to the oral and nasal mucosa to innervate nasal and palatal glands.

Fig. 7.5 Schematic of functions of the facial nerve. See text for details. (From Harnsberger HR. Handbook of Head and Neck Imaging [2nd ed.]. St. Louis, MO: Mosby, 1995. Reprinted with permission.)
Chorda Tympani Nerve
• GVE (parasympathetic) + SA (taste).
• Arises from the mastoid segment of CN VII (see below).
• Traverses the middle ear cavity medial to the tympanic membrane, then exits the cranium via a part of the petrotympanic fissure known as the canal of Huguier to join the lingual branch of CN V3 ~1 cm below the foramen ovale at the submandibular ganglion.
• Preganglionic parasympathetics synapse in the submandibular ganglion.
• Postganglionic parasympathetics then travel with the lingual nerve to the submandibular and sublingual glands (for salivation).
• Taste sensation (SA) from the anterior two thirds of the tongue and hard and soft palates is transmitted via the chorda tympani nerve to the geniculate ganglion, then via nervus intermedius to the rostral nucleus solitarius (also called “gustatory nucleus”) in the medulla.
• Taste information then ascends via the central tegmental tract to the ventropostereomedial nucleus (VPM) of the thalamus, synapses, and terminates in the gustatory cortex located in the postcentral parietal operculum and insula.
Facial Nerve: Normal Images
• Both computed tomography (CT) and magnetic resonance imaging (MRI) play an important role in the assessment of facial nerve disorders, and appropriate indications for each are discussed below and summarized in Table 7.1. CT is generally done with thin sections (1.25 mm or less) and a high-resolution bone algorithm. This allows for precise assessment of the bony facial canal, as well as adjacent temporal bone structures. For MR, in addition to the routine T1- and T2-weighted images that would generally be done as part of any MR scan of the brain, head and neck, or skull base, thin-section high-resolution heavily T2-weighted sequences such as fast imaging employing steady-state acquisition (FIESTA) or constructive interference in steady-state (CISS) should be performed. These sequences produce a “myelographic effect” with the nerve in sharp contrast to surrounding high signal intensity cerebrospinal fluid (CSF) and allow a high-resolution assessment of the cisternal and intracanalicular segments of the nerve. Post-gadolinium T1-weighted images with fat saturation are performed to assess for pathology of the brainstem and meninges, as well as abnormal enhancement of the nerve itself.
| CT Indications | MR Indications | |
|---|---|---|
| Congenital anomalies (e.g., EAC atresia) | Suspected brainstem disease | |
| Cisternal or intracanalicular disease | ||
| Inflammatory disease/cholesteatoma | Atypical Bell’s palsy | |
| Temporal bone fracture | Parotid mass or history of parotid cancer | |
| Hemangioma | Intracranial complications of inflammatory disease |
Note: in many cases, CT and MR are complementary.
Normal CTs
• (Figs. 7.6, 7.7, 7.8, 7.9, 7.10, 7.11, 7.12 and 7.13)

Fig. 7.6 An axial CT image in bone window shows normal bilateral temporal bone anatomy. Labeled on the right: IAC (*), horizontal semicircular canal (black straight arrow), middle ear cavity with ossicles (white arrow) and well-aerated mastoid antrum and mastoid air cells (mac). The fallopian canal (black concave arrow) courses anteriorly from the apex of the IAC and contains the labyrinthine segment of the facial nerve.

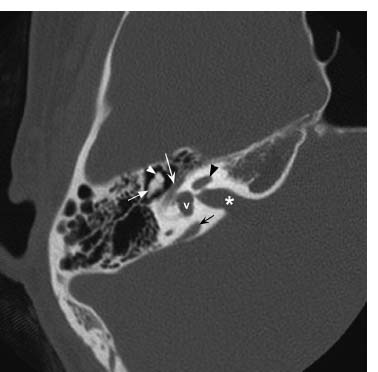
Fig. 7.8 More inferiorly but still at the level of the internal auditory canal (*), an axial CT image in bone window further defines the course of the tympanic segment of the facial nerve canal (white concave arrow) as it travels posteriorly. Visualized inner ear structures include the cochlea (black straight arrowhead) and vestibule (v). The normal “ice cream cone” appearance of the head of the malleus (white straight arrowhead) and body of the incus (white straight arrow) is seen in the middle ear cavity. A mildly enhanced vestibular aqueduct (black concave arrow) is present.
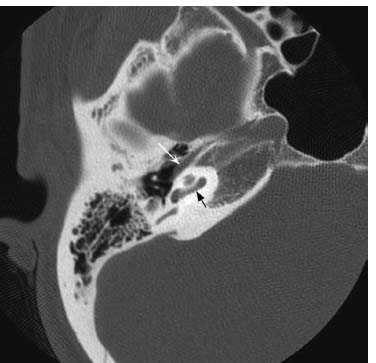
Fig. 7.9 An axial CT image in bone window at the level of the basal turn of the cochlea (black arrow) shows the tensor tympani muscle (white arrow), which can mimic the tympanic segment of the facial nerve. This is a common pitfall that is easily avoided by reviewing the images immediately above and below to confirm it is separate from the facial nerve canal.
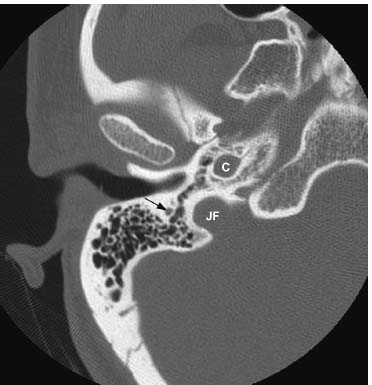
Fig. 7.10 More inferiorly, the nerve has turned 90 degrees and the vertical mastoid segment of the facial nerve canal (arrow) is shown. Normal jugular foramen (JF) and vertical segment of petrous carotid canal (C) are indicated.

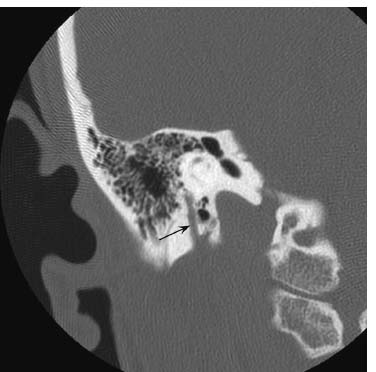
Fig. 7.12 More posteriorly, a coronal CT image in bone window shows the normal descending (vertical) mastoid segment of the facial nerve canal (arrow) extending inferiorly to the stylomastoid foramen.
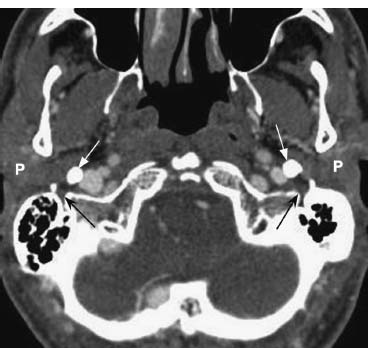
Fig. 7.13 An axial postcontrast CT in soft tissue window through the lower skull base shows the normal stylomastoid foramina bilaterally (black arrows), posterolateral to large styloid processes (white arrows). Normal parotid glands (P).
Normal MRIs
• (Figs. 7.14, 7.15, 7.16, 7.17 and 7.18)
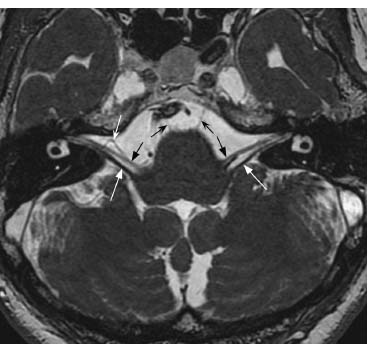
Fig. 7.14 An axial FIESTA image through the posterior fossa shows normal CN VII and CN VIII exiting the lateral aspect of the pontomedullary junction (black straight arrows: CN VII; white straight arrows: CN VIII, vestibular division) and coursing into the internal auditory canal. Bilateral VI nerves (small black arrows) exit the ventral pontomedullary junction and traverse the prepontine cistern. Note the small flow void on the right (white concave arrow) that typically represents a loop of AICA and is commonly seen in asymptomatic patients.
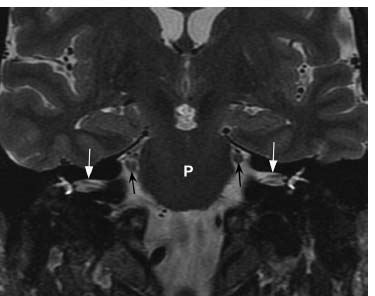
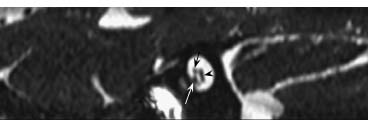
Fig. 7.16 An oblique parasagittal high-resolution FIESTA image through the internal auditory canal shows the normal positions of CNs VII and VIII. CN VII (black cconcave arrow) is located anterosuperiorly and is slightly smaller in size than the anteroinferiorly located cochlear nerve (white arrow). Posteriorly, the vestibular component of CN VIII (black arrowhead) is starting to divide into superior and inferior divisions.
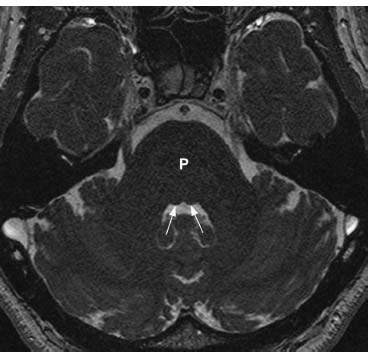
Fig. 7.17 An axial FIESTA image through the posterior fossa at the level of the midpons (P) shows normal facial colliculi bilaterally (arrows). The facial colliculus is a small bulge of the dorsal pons into the fourth ventricle at the site where the facial nerve loops around the abducens nucleus.
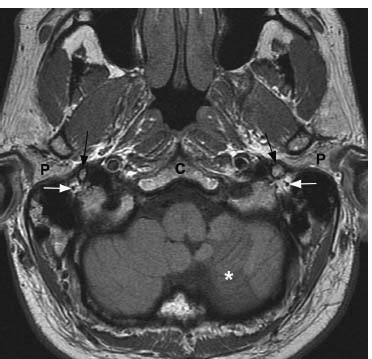
Fig. 7.18 An axial T1-weighted image through the lower skull base demonstrates normal bilateral stylomastoid foramina filled with fat. The centrally located dot of dark signal (white arrows) is the normal CN VII traversing the foramen prior to entering the parotid glands. Normal parotid tissue (P) is noted anterolaterally. Dark signal lateral to the foramina represents air within the inferior mastoid air cells. Anteromedial to the foramina, the normal styloid processes (black arrows) are seen: a rim of dark signal represents cortical bone and the central hyperintensity represents fatty marrow. A remote left inferior cerebellar infarct (asterisk) is present. (C, clivus.)
Facial Nerve Lesions
Types
Supranuclear Lesions
• Lead to contralateral paresis/palsy of lower portion of face (“central CN VII” lesion).
• Upper part of the face is spared due to bilateral supranuclear innervation.
Nuclear and Fascicular Lesions
• Lead to ipsilateral paresis/palsy of entire face (“peripheral CN VII” lesion).
• Lesion within pons may affect nearby structures, for example, CN V, CN VI, paramedian pontine reticular formation (PPRF), corticospinal tract (CST), spinothalamic tract (STT).
• Millard-Gubler syndrome. Lesion in ventral pons affecting CN VI, CN VII, CST. CN VII involvement is due to involvement of the fascicles of CN VII, not the more dorsally located CN VII motor nucleus. Characterized by ipsilateral peripheral CN VII paralysis, ipsilateral abducens palsy, contralateral hemiplegia.
• Foville syndrome. Lesion in pons affecting CN VII, CN VI, PPRF, CST. Characterized by ipsilateral peripheral CN VII paralysis, ipsilateral conjugate gaze paralysis, contralateral hemiplegia.
• See Appendix A (The Brainstem) for a review of anatomical details .
Cerebellopontine Angle Lesions
• In the cerebellopontine angle (CPA) cistern, CN VII travels with nervus intermedius and near CN VIII. Masses of the CPA cistern (e.g., acoustic neuroma, meningioma) result variably in ipsilateral peripheral CN VII paralysis, loss of taste over anterior two thirds of tongue, hyperacusis, ipsilateral tinnitus, hearing loss, and/or vertigo. CPA masses affect CN VIII function far more commonly than CN VII function.
• Lesions in CPA may displace or compress pons, cerebellum, or other CNs (e.g., CN V, CN VI).
• Hemifacial spasm. Usually due to neurovascular compression of the motor root of CN VII in the CPA (see Case 7.8).
• Geniculate neuralgia (also called nervus intermedius neuralgia or Hunt neuralgia). Neuralgia affecting the sensory root of CN VII (nervus intermedius), causing paroxysmal otalgia similar to the ear form of glossopharyngeal neuralgia (see Chapter 9). Attributed to vascular—usually anterior inferior cerebellar artery (AICA)—compression of nervus intermedius. Treatment is with carbamazepine, microvascular decompression, or sectioning of the nervus intermedius and/or geniculate ganglion.
More Peripheral Lesions
• Most common causes of unilateral complete facial paralysis are Bell’s palsy, trauma, and Ramsay Hunt syndrome (herpes zoster oticus).
• Bell’s palsy (idiopathic facial palsy). Unilateral CN VII dysfunction with sudden onset (see case discussion below).
• Ramsay Hunt syndrome (herpes zoster oticus) (see Case 7.6).
• Posttraumatic facial palsy. The facial nerve is the most commonly injured motor CN (see Case 7.13).
• Möbius syndrome. Congenital bilateral CN VI and CN VII palsies due to neural underdevelopment.
• Additional causes of peripheral facial palsy include
 Malignancy (e.g., parotid, temporal bone).
Malignancy (e.g., parotid, temporal bone).
 Infectious/inflammatory (e.g., varicella-zoster virus [VZV], Lyme disease, syphilis, acquired immunodeficiency syndrome [AIDS], mononucleosis, Guillian-Barré syndrome [Miller-Fisher variant]).
Infectious/inflammatory (e.g., varicella-zoster virus [VZV], Lyme disease, syphilis, acquired immunodeficiency syndrome [AIDS], mononucleosis, Guillian-Barré syndrome [Miller-Fisher variant]).
 Iatrogenic (e.g., parotid surgery, temporal bone surgery).
Iatrogenic (e.g., parotid surgery, temporal bone surgery).
 Granulomatous and connective tissue diseases (e.g., sarcoidosis, Wegener granulomatosis).
Granulomatous and connective tissue diseases (e.g., sarcoidosis, Wegener granulomatosis).
• Facial nerve dysfunction is most commonly described using the House-Brackmann classification scheme (Table 7.2).
| Grade | Definition | |
|---|---|---|
| I | Normal facial function | |
| II | Slight weakness noticeable on close inspection | |
| II | Forehead—moderate-to-good function | |
| Eye—complete closure with minimal effort | ||
| Mouth—slight asymmetry | ||
| III | Obvious weakness, but not disfiguring | |
| Forehead—slight-to-moderate movement | ||
| Eye—complete closure with effort | ||
| Mouth—slightly weak with maximum effort | ||
| IV | Obvious weakness and/or disfiguring asymmetry | |
| Forehead—no motion | ||
| Eye—incomplete closure | ||
| Mouth—asymmetric with maximum effort | ||
| V |