9 Facial Skeleton and Skull Base
Fundamentals
Clinical Aspects
Computed tomography (CT), with its high spatial resolution and detailed portrayal of bony anatomy, plays a special role in the diagnosis of diseases of the skull base, maxillofacial skeleton, and especially the petrous bone. The high-contrast visualization of soft-tissue structures that is possible with CT, combined with the use of densitometry for tissue discrimination, can often provide a definitive diagnosis even without the use of additional modalities such as magnetic resonance imaging (MRI). CT is the method of choice in examinations of the petrous pyramid, especially its osseous structures, and in screening for craniofacial fractures. Conventional tomography has become largely obsolete for this application.
If the patient has adequate flexibility of the cervical spine, direct coronal or even sagittal CT head images can be acquired in addition to axial scans. In other body regions, these views can be obtained only with MRI.
Common Indications
Inflammatory sinus diseases are among the most common indications for CT imaging of the midfacial region. Mucosal swelling, retained secretions, polyps, or bony abnormalities (erosion due to chronic sinusitis or bony deformities) may be responsible for the obstruction of sinus drainage. Coronal scanning is ideal for detecting these lesions, and it is better than axial scans for defining the relationship of sinus lesions to the orbit and excluding involvement of the skull base and neurocranium. Axial scans are preferred only for evaluating the pterygopalatine fossa and in cases in which coronal scans are difficult to interpret due to beam-hardening artifacts from nonremovable denture material or fillings. If necessary, the axial scans can be processed to generate reformatted images. The choice of slice thickness is governed by the general principles of CT imaging. Thin slices allow detailed evaluation of osseous structures, particularly by reducing partial volume effects, while somewhat thicker slices are often better for detecting soft-tissue abnormalities.
Another important indication for CT is in evaluating for osseous involvement or penetration of the bony skull base by a primary intracranial or extracranial tumor, such as meningioma or sinus carcinoma. CT is often performed as an adjunct to existing magnetic resonance images in this type of investigation.
In addition to showing bone destruction, CT can also demonstrate invasion through the foramina of the skull base. This is best appreciated on direct coronal scans or images reformatted from thin axial slices. Intravenous contrast administration will sometimes detect intracranial involvement by demonstrating enhancement of the meninges.
CT is an important tool for three-dimensional planning of surgical procedures, the planning of corrective or reconstructive procedures, and the fabrication of prosthetic bone implants and appliances used in oromaxillofacial surgery. Another application in this context is the use of CT data sets to carry out virtual endoscopy of the paranasal sinuses and image-guided surgical navigation.
The ability to generate suitable two-dimensional reformatted images of the maxilla and mandible is particularly useful for planning implantation procedures in oral surgery. The nonsuperimposed images provided by “dental CT” can be used to determine the dimensions of the alveolar crest and the cortical bone thickness with very high accuracy. Lesions can also be localized to specific dental regions with greater confidence, making it easier to compare CT findings with standard panoramic radiographs (Figs. 9.1 9.2).
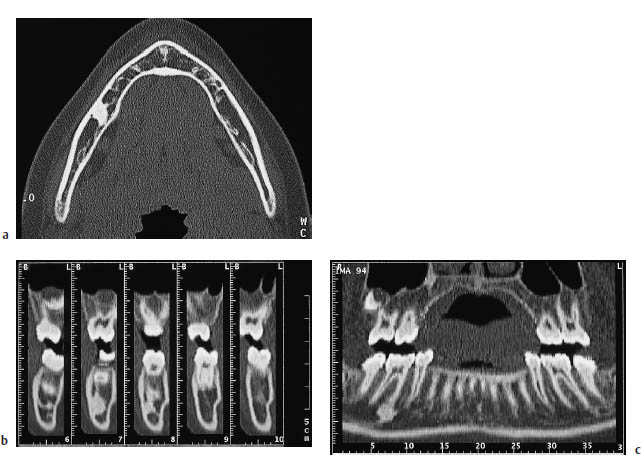
Fig. 9.1a–c Osteoma of the mandible.
a Conventional axial CT scan of a woman with a mandibular osteoma.
b, c Semiautomated software is used to generate reformatted images perpendicular (b) and tangential (c) to the mandibular ramus. This technique, called dental CT, can document the precise relationship of the osteoma to the root of the right first molar using a scale at the bottom of the image (L: lingual; B: buccal).

Malformations and Functional Disturbances
The nasal cavity, and the paranasal sinuses in particular, are subject to such extensive anatomic variation that diagnostic evaluations have to center on the question of whether demonstrable sinonasal changes have functional significance. Particularly in patients with chronic inflammatory sinus disease, CT can significantly advance the diagnosis by detecting impairment of sinus drainage due to normal anatomic variants or abnormal masses. These changes are best appreciated on direct coronal scans, although sagittal images reformatted from thin-slice axial data sets are helpful or necessary for some indications.
Inflammatory Sinus Disease (Fig. 9.3)
Frequency: very common.
Suggestive morphologic findings: mucosal thickening, retained secretions, possible bone erosion.
Procedure: coronal imaging. Some cases may require sagittal images reformatted from axial data.
Other studies: conventional radiographs.
Checklist for scan interpretation:
 Osteomeatal complex?
Osteomeatal complex?
 Outflow obstruction due to normal anatomic variant?
Outflow obstruction due to normal anatomic variant?
 Bone destruction?
Bone destruction?
 Mucocele formation?
Mucocele formation?
 Pathogenesis
Pathogenesis
Inflammatory sinus disease is perhaps the most frequent indication for midfacial CT examinations. Direct coronal scanning (coronal sinus CT) is generally best for this purpose. It may be possible to reduce radiation exposure by acquiring noncontiguous thin slices, depending on the requirements of the referring physician. For presurgical assessment, however, contiguous thin-slice coverage should be obtained. The essential role of sinus CT is to define the ostia of the paranasal sinuses and identify possible outflow obstructions.
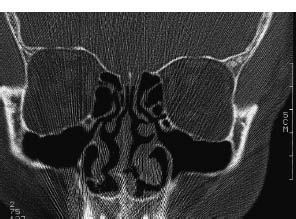
Fig. 9.3 Coronal sinus CT scan at the level of the osteomeatal complex defines the drainage tract of the maxillary sinus, frontal sinus, and anterior ethmoid cells.
Based on these discoveries, the concept of treating chronic inflammatory sinus disease with an old-fashioned fenestration procedure has given way to minimally invasive techniques in which the goal is to restore the natural routes of sinus drainage. Some of these techniques are already using image-guided navigation, in which an instrument is manipulated within a CT-based stereotactic space while its position is visualized in real time within the data set.
 Frequency
Frequency
Very common.
 Clinical Manifestations
Clinical Manifestations
Inflammatory sinus disease presents with facial pain and headache that are aggravated by activities causing increased sinonasal pressure (e.g., coughing). Other symptoms are a feeling of pressure and nasal or postnasal drainage.
 CT Morphology
CT Morphology
In addition to the detection of mucosal thickening and accumulated secretions, special attention should be given to the sinus drainage routes, in view of the pathophysiology described above. Of key interest is the “osteomeatal complex,” which is the route by which the anterior ethmoid cells, frontal sinus, and maxillary sinus are drained. As a result, anything causing obstruction of the osteomeatal complex can cause obstruction and disease in these three sinuses. (The drainage route of the sphenoid sinus and possible constrictions of the frontal sinus are best displayed in sagittal images reformatted from thin axial data sets.) Causes of obstruction in the osteomeatal complex include normal anatomic variants such as concha bullosa, ethmoid bullae, Haller cells of the maxillary sinus, and deviation of the bony nasal septum.
Choanal Atresia (Figs. 9.4, 9.5)
Frequency: the incidence of choanal atresia is one in 5000–8000 live births, with a female preponderance.
Suggestive morphologic findings: obstruction of the choanae by bone or connective tissue.
Procedure: evaluate with thin CT slices (2 – 3 mm) angled at approximately 5° to the hard palate.
Other studies: CT is the imaging procedure of choice.
Checklist for scan interpretation:
 Bony atresia?
Bony atresia?
 Membranous atresia?
Membranous atresia?
 Pathogenesis
Pathogenesis
Choanal atresia is a congenital anomaly in which one or both choanae are obstructed by bone or connective tissue. It occurs when a mesenchymal tissue membrane between the neurocranium and viscerocranium fails to disappear during embryonic development. Bilateral choanal atresia can be life-threatening in neonates, because the relatively high position of the larynx impedes oral breathing. These cases require immediate intervention to establish a nasal airway.
Choanal atresia sometimes occurs in association with other anomalies, which have been designated with the acronym CHARGE (coloboma, heart disease, atresia choanae, retarded growth, genital hypoplasia, ear anomalies).
Females are more commonly affected. Hereditary factors have been identified. In approximately 75% of cases, choanal atresia is associated with other congenital defects or anomalies of the facial skeleton. The incidence is estimated at one in 5000–8000 births.
 Clinical Manifestations
Clinical Manifestations
Nasal airway obstruction in the neonate, which can be life-threatening.
 CT Morphology
CT Morphology
CT is the imaging modality of choice, and the CT results direct the choice of surgical treatment. While a membranous obstruction can be perforated endoscopically, bony atresia usually requires a partial transpalatal resection of the vomer, which appears thickened posteriorly on axial CT scans (Fig. 9.4). Sagittal reformatted images can also help to define the choanal obstruction (Fig. 9.5). Choanal width should be at least 3.7 mm by 2years of age and at least 3.4 mm by 8years of age.
Tornwaldt Cyst
Frequency: a relatively common incidental finding.
Suggestive morphologic findings: midline cystic mass in the upper nasopharynx.
Procedure: may require thin-slice scanning.
Other studies: sagittal T2-weighted MRI is the method of choice.
Checklist for scan interpretation:
 Differentiation is required from other nasopharyngeal masses, especially neoplasms.
Differentiation is required from other nasopharyngeal masses, especially neoplasms.
 Pathogenesis
Pathogenesis
Known also as pharyngeal bursitis, this anomaly results from persistence of the median fissure of the pharyngeal tonsil, which may close secondarily, leading to the formation of a pouch or cyst known as a Tornwaldt cyst. The cyst is filled with secretions and debris, and can produce a foul-smelling discharge when not completely closed. Inflammation of surrounding tissues is common.

Fig. 9.4 Bilateral bony choanal atresia. Posterior thickening of the vomer is clearly visible in this axial CT scan.
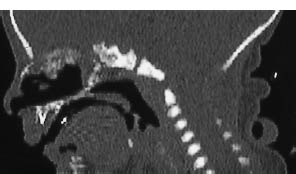
Fig. 9.5 Bilateral bony choanal atresia. Sagittal image reconstructed from the axial data set clearly demonstrates the obstructing bony membrane.
 Frequency
Frequency
Tornwaldt cyst is a relatively common incidental finding.
Foul-smelling discharge, surrounding inflammatory reaction.
 CT Morphology
CT Morphology
CT demonstrates a midline cystic mass arising from the pharyngeal tonsil.
Otosclerosis
Frequency: the clinically overt form is somewhat rare, but otosclerotic lesions are found in up to 8% of autopsies. Women predominate by a ratio of about 2:1.
Suggestive morphologic findings: thickening of the stapes footplate, low-density resorption halo surrounding the cochlea.
Procedure: high-resolution CT, if necessary combined with densitometry; follow-ups.
Other studies: thin-slice MRI with intravenous contrast medium. Radionuclide bone scanning shows increased bone turnover during the active phase of otosclerosis.
Checklist for scan interpretation:
 Acuteness of the disease.
Acuteness of the disease.
 Differentiate from focal manifestations of other systemic skeletal diseases with petrous bone involvement.
Differentiate from focal manifestations of other systemic skeletal diseases with petrous bone involvement.
 Pathogenesis
Pathogenesis
Otosclerosis is a primary focal disease of the bony otic capsule. Its etiology is unknown, but its familial occurrence and tendency to progress during pregnancy suggest a multifactorial etiology based on a combination of genetic and hormonal factors. Histologically, the active phase of the disease is characterized by abnormally increased activity of histiocytes and osteocytes in the otic capsule. This leads to resorption of the dense capsular bone, which is subsequently replaced by more vascularized spongy bone. This is followed by a reparative phase in which the spongy bone is replaced by dense, relatively avascular and acellular bone. The foci may progressively increase in size and eventually project into the middle ear cavity.
The most common site of occurrence is the otic capsule near the oval window. Usually, the sclerotic lesions cause fixation of the stapes footplate, and CT will often demonstrate thickening of the footplate in the oval window. The result is progressive conductive hearing loss. Involvement of the cochlea by otosclerotic foci can lead to sensorineural hearing loss.
The disease usually takes an undulating course, marked by alternating periods of remission and exacerbation. Early manifestation generally implies a poor prognosis.
Involvement of the middle ear and inner ear by Paget disease, osteogenesis imperfecta, or manifestations of other skeletal diseases are important differential diagnoses that may require further imaging studies or even laboratory tests, to distinguish them from otosclerosis.
 Frequency
Frequency
Otosclerosis is a relatively rare disease with an obscure, multifactorial etiology that appears to involve both genetic and hormonal causes. Women predominate by a ratio of about 2: 1, and Europeans are affected more often than Japanese and Africans. The clinically overt form is relatively rare, but otosclerotic foci are discovered in up to 8% of autopsies.
 Clinical Manifestations
Clinical Manifestations
Otosclerosis presents clinically with conductive hearing loss, sometimes accompanied by a sensorineural component. The pure-tone audiogram usually indicates pure conductive hearing loss, and the stapedius reflex may be abolished. The treatment of choice consists of stapedectomy with stapes reconstruction.
 CT Morphology
CT Morphology
There are two characteristic CT findings in otosclerosis. With fenestral otosclerosis, the oval window may be narrowed from its normal size of approximately 3 × 2 mm, and there may be appreciable thickening of the stapes footplate. With cochlear otosclerosis, a low-density resorption halo can be seen surrounding the cochlea during the active phase of the disease. Both findings can be seen only with high-resolution CT.
High-resolution CT can also be used to perform densitometry of the cochlear capsule. This is done by measuring the attenuation values at a number of defined points and comparing them with measurements in a normal population. Densitometry is also useful for following the progression of the disease and assessing its response to treatment.
Another important role for CT lies in documenting the postoperative findings after stapes reconstruction.
Tumors and Other Mass Lesions
This section deals with tumors of the skull base, petrous bone, and midfacial region that are important because of their frequency, imaging features, or potential importance in CT differential diagnosis. This listing is by no means complete. Several entities, such as meningioma and acoustic schwannoma, are discussed in Chapter 5 above, and are mentioned here only for completeness.
Odontogenic Tumors
Odontogenic tumors are mostly neoplasms that develop from the dental lamina. Generally, they are benign and rarely undergo malignant transformation. Because of their initial paucity of symptoms, these tumors are usually diagnosed only after they have produced significant facial deformity or asymmetry. The most important odontogenic tumors include ameloblastoma and odontoma, both of epithelial origin, and cementoma, which has a mesodermal origin. There are also numerous mixed forms, for which the varying proportions of tissue components are usually designated by the prefix “fibro-” or “myxo-,” depending on whether the tumor has a high content of fibrous or connective tissue, or is mucus-forming. Conventional radiography is still the best method for the detection and differential diagnosis of lesions.
Ameloblastoma (Fig. 9.6)
Frequency: the most common jaw tumor. Most prevalent in the fourth and fifth decades of life, with no predilection for either sex.
Suggestive morphologic findings: CT shows an expansile mass associated with thinning of the cortex. The mass is occasionally multilocular and may contain a tooth bud. An extraosseous mass may develop.
Procedure: evaluate with thin-slice bone-window CT scans.
Other studies: MRI, panoramic radiograph.
Checklist for scan interpretation:
 Consider range of differential diagnoses.
Consider range of differential diagnoses.
 Risk of fracture?
Risk of fracture?
 Degree of destruction?
Degree of destruction?
 Pathogenesis
Pathogenesis
Ameloblastoma is the most common jaw tumor. It is slow-growing, but locally destructive. The solid forms tend to be locally invasive, while the cystic forms show a more benign growth pattern. Recurrence is common after surgical removal, and up to 2% undergo malignant transformation. Approximately one-third are associated with a follicular cyst.
 Frequency
Frequency
Ameloblastoma is the most common tumor of the maxillomandibular region. It usually occurs in the fourth or fifth decade of life, and shows no predilection for either sex. The mandible is affected in 75% of cases, the maxilla in 25%.
 Clinical Manifestations
Clinical Manifestations
Ameloblastomas often grow for some time without causing symptoms, and are usually diagnosed only after causing appreciable jaw deformity.
 CT Morphology
CT Morphology
CT shows a unilocular or multilocular “honeycomb” lytic lesion with expansile margins. Because ameloblastomas are sometimes derived from a follicular cyst, they may contain a rudimentary or complete tooth. Their tendency to erode through the cortex can produce an extraosseous soft-tissue mass (Fig. 9.6).
Odontoma
Frequency: rare.
Suggestive morphologic findings: amorphous calcified mass or malformed tooth bud. Procedure: evaluate with thin-slice CT scans. Dental CT may also be used.
Other studies: conventional panoramic radiograph.
Checklist for scan interpretation:
 Differential-diagnostic classification.
Differential-diagnostic classification.
 Pathogenesis
Pathogenesis
Odontomas contain all the tissue elements of a complete tooth: enamel, dentine, cement, and pulp. Consequently, they are more accurately described as malformations rather than tumors. There are numerous mixed forms, however, such as ameloblastic fibro-odontoma. Odontomas are of two basic types: complex odontomas, in which all the dental tissues occur in a disorderly pattern, and compound odontomas, in which the dental tissues show a high degree of differentiation. Numerous transitional forms also occur.
 Frequency
Frequency
Rare.
Nonspecific.
 CT Morphology
CT Morphology
There are no specific CT features of odontomas. They may appear as amorphous calcified masses or as malformed tooth buds.
Cementoma
Frequency: rare.
Suggestive morphologic findings: apical densities, usually located in the mandible. Mixed lytic-sclerotic patterns may occur.
Procedure: evaluate with thin-slice bone-window scans. Dental CT may also be used.
Other studies: panoramic radiograph.
Checklist for scan interpretation:
 Differentiate from ossifying fibroma and fibrous dysplasia.
Differentiate from ossifying fibroma and fibrous dysplasia.
 Pathogenesis
Pathogenesis
Cementoma is a collective term for a number of lesions that cannot be distinguished from one another by imaging studies, particularly CT. These lesions include:
• Cementoblastoma
• Cement-forming fibroma
• Periapical cemental dysplasia
Although cementomas are usually sclerotic, imaging may show periapical or even cystic hypodensities, depending on the specific entity and the stage of the disease.
 Frequency
Frequency
Rare.
 Clinical Manifestations
Clinical Manifestations
Nonspecific.
 CT Morphology
CT Morphology
The typical CT appearance is that of an apical density, which may be quite small and is usually located in the mandible. Multicentric lesions are common. Mixed patterns with a combination of lytic and sclerotic features are also seen. Differentiation is required from ossifying fibroma and, with extensive involvement, from fibrous dysplasia.
Cystic Lesions of the Maxilla and Mandible
Frequency: small, clinically insignificant lesions are common.
Suggestive morphologic findings: cystic lesions in the maxilla or mandible, often developing around a single devitalized tooth, but occasionally involving a whole quadrant. Follicular cysts with tooth buds have a CT attenuation of approximately 5–15 HU. Odontogenic cysts have a peripheral calcified rim.
Procedure: evaluate with thin CT slices. Use dental CT as required.
Other studies: panoramic radiograph. Dental spot films are useful for smaller lesions. Other options: dental CT, MRI.
Checklist for scan interpretation:
 Differentiate from other entities.
Differentiate from other entities.
 Pathogenesis
Pathogenesis
Since the majority of these lesions are not distinguishable by CT, and as differential diagnosis usually requires a panoramic radiograph or dental spot films, we shall briefly review only the most important entities.
True cysts, which have an epithelial lining, are distinguished from pseudocysts, which lack this lining. Their imaging appearance is marked by a slow, expansile growth pattern, usually resulting in well-defined margins or even a sclerotic rim if there is no inflammatory component inciting a perifocal reaction.
A further distinction is made between odontogenic and nonodontogenic cysts.
Odontogenic cysts. These include the following:
• Radicular cysts, which form around the apex of a diseased tooth, and lateral cysts, which project into the bone from lateral pulpal defects.
• Follicular cysts, which result from aberrant differentiation of the dental lamina. A primordial cyst can develop at the site of a supernumerary tooth bud. The primordial cyst can subsequently develop into a keratocyst through active keratinization of its epithelial lining. Other follicular cysts develop around the crown of an impacted or unerupted tooth (e.g., an eruption cyst around a wisdom tooth). The mandibular angle is a frequent site of occurrence (Figs. 9.7, 9.8).
Nonodontogenic cysts. Often located on the midline, nonodontogenic cysts develop from epithelial rests of the nasopalatine duct or from heterotopic elements of the palatine suture. In a broader sense, the nonodontogenic cysts include mucocele, aneurysmal bone cyst, and solitary bone cyst. While aneurysmal and solitary bone cysts are indistinguishable by conventional radiography, CT can sometimes demonstrate heterogeneous densities within an aneurysmal bone cyst, caused by blood-filled spaces within the lesion. In addition, internal portions of an aneurysmal bone cyst may enhance after intravenous contrast administration.
 Frequency
Frequency
The most common cystic jaw lesions are radicular cysts that develop around a devitalized tooth. The other entities are somewhat rare.
 Clinical Manifestations
Clinical Manifestations
Besides their direct effects on involved teeth, cystic jaw lesions produce symptoms by their local mass effects on adjacent structures. These include mandibular nerve compression within the alveolar canal or involvement of the paranasal sinuses.
 CT Morphology
CT Morphology
CT demonstrates cystic lesions in the maxilla or mandible, which may surround individual tooth roots (often devitalized teeth), or may affect a whole quadrant. Follicular cysts may contain partial or complete tooth buds. Internal attenuation values range from 5 to 15 HU. Different types of cyst are indistinguishable by CT. Keratocysts can grow very large, expanding into the maxillary sinus. These large cysts are often septated or lobulated.
Odontogenic cysts frequently have a typical peripheral calcified rim along with central tooth buds.
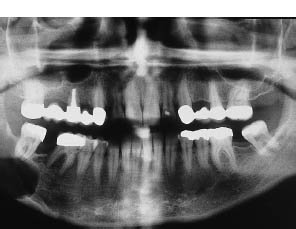
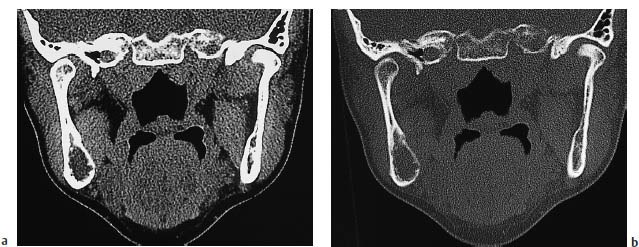
Fig. 9.7 Cystic lucency. Panoramic radiograph demonstrates a cystic lucency of the right mandibular angle with no visible tooth bud. Radicular cyst.
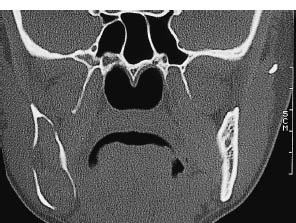
Fig. 9.8 Follicular cyst (keratocyst). Coronal bone-window CT shows the typical appearance of a follicular cyst at its most common site of occurrence.
Mucocele, Pyocele (Fig. 9.9)
Frequency: the most common cause of an expansile paranasal sinus mass; frequent in cystic fibrosis.
Suggestive morphologic findings: expansile soft-tissue mass of the paranasal sinuses; may be associated with bone erosion and ingrowth (e.g., into the orbit).
Procedure: evaluate with thin-slice axial scans or coronal bone-window CT.
Other studies: the lesions display a high signal intensity on T1-weighted and T2-weighted MRI. Conventional radiographs show extensive bone erosion.
Checklist for scan interpretation:
 Degree of expansion?
Degree of expansion?
 Compression of important structures (e.g., optic nerve) or central nervous sytem (CNS) pathways?
Compression of important structures (e.g., optic nerve) or central nervous sytem (CNS) pathways?
 Signs of superinfection?
Signs of superinfection?
 Pathogenesis
Pathogenesis
Mucoceles and pyoceles result from obstruction of the excretory duct of a paranasal sinus and from the retention of secretions within the sinus. The obstruction may be caused by an inflammatory process, trauma, or neoplasm. Rising intrasinus pressure tends to erode the bony wall, eventually transforming it into a fibrous capsule. Various mass effects can develop, such as exophthalmos caused by a mucocele in the frontal sinus (Fig. 9.9).
The most commonly affected sinuses are as follows (in descending order of frequency):
• Frontal sinus
• Ethmoid sinus
• Maxillary sinus
The sphenoid sinus is very rarely affected. A special form is a mucocele of the lacrimal sac, which is sometimes bilateral.

Fig. 9.9a–c Mucocele. These images show a mucocele that arose from the anterior ethmoid cells and has invaded the orbit secondarily, presenting clinically as exophthalmos. The lesion is particularly well demonstrated by coronal magnetic resonance imaging (c).
 Frequency
Frequency
Mucocele is the most frequent cause of an expansile paranasal sinus mass. Its incidence is increased in cystic fibrosis.
 Clinical Manifestations
Clinical Manifestations
 CT Morphology
CT Morphology
CT demonstrates a soft-tissue mass that may be associated with paranasal sinus expansion or bone erosion. Usually the mass does not enhance after contrast administration, but a mucocele may cause an accompanying inflammatory reaction that appears as a peripheral enhancing ring. Internal attenuation values depend on the degree of inspissation of the contents, and usually range from 40 to 50 HU.
Papilloma
Frequency: relatively rare. The two forms (inverted and exophytic) are about equally common.
Suggestive morphologic findings: inverted papilloma: lobulated surface, projects into paranasal sinus from nasal cavity; always unilateral. Exophytic papilloma: wart-like mass arising from the septum.
Procedure: coronal and axial scans.
Other studies: MRI is better than CT for distinguishing the papillomatous component from possible squamous-cell carcinoma located within the papilloma.
Checklist for scan interpretation:
 Surface structure? Extent of destruction?
Surface structure? Extent of destruction?
 Compression of CNS pathways?
Compression of CNS pathways?
 Malignant transformation?
Malignant transformation?
 Pathogenesis
Pathogenesis
Papillomas are masses that arise from the mucosa lining the nasal cavity or paranasal sinuses. Several types are distinguished:
• Exophytic papilloma
• Inverted papilloma
• Cylindrical cell papilloma (rare)
Exophytic papillomas almost always arise from the nasal septum and have a wart-like gross appearance. Generally, they do not undergo malignant change.
Inverted papillomas arise from the lateral nasal wall and typically project into the ethmoid cells or maxillary sinus. They consist of a hyperplastic epithelium that is “inverted” into the underlying stroma. Inverted papillomas are always unilateral and have an extremely high recurrence rate after excision. Up to 15% of these lesions are associated with squamouscell carcinoma, underscoring the importance of early detection and complete surgical removal.
 Frequency
Frequency
Inverted papilloma is the most common of all epithelial papillomas. Men are predominantly affected. The most common site of occurrence is the lateral nasal wall, from which the lesion projects into the paranasal sinuses. Some sources state that inverted and exophytic papillomas occur with approximately equal frequency.
 Clinical Manifestations
Clinical Manifestations
Besides local symptoms, progressive nasal airway obstruction is the dominant feature in most patients.
 CT Morphology
CT Morphology
Exophytic papilloma arises from the nasal septum, while inverted papilloma arises from the lateral wall of the nasal cavity and projects into the paranasal sinuses. A lobulated surface structure is considered typical of inverted papilloma.
Frequency: the neurocranium or viscerocranium is involved in 15–20% of cases.
Suggestive morphologic findings:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





