Chapter 2 Fair Game
Maki DD, Grossman RI. Patterns of disease spread in metastatic breast carcinoma: influence of estrogen and progesterone receptor status. AJNR Am J Neuroradiol. 2000;21:1064-1066.
Walker R, Kessar P, Blanchard R, et al. Turbo STIR magnetic resonance imaging as a whole-body screening tool for metastases in patients with breast carcinoma: preliminary clinical experience. J Magn Reson Imaging. 2000;11:343-350.
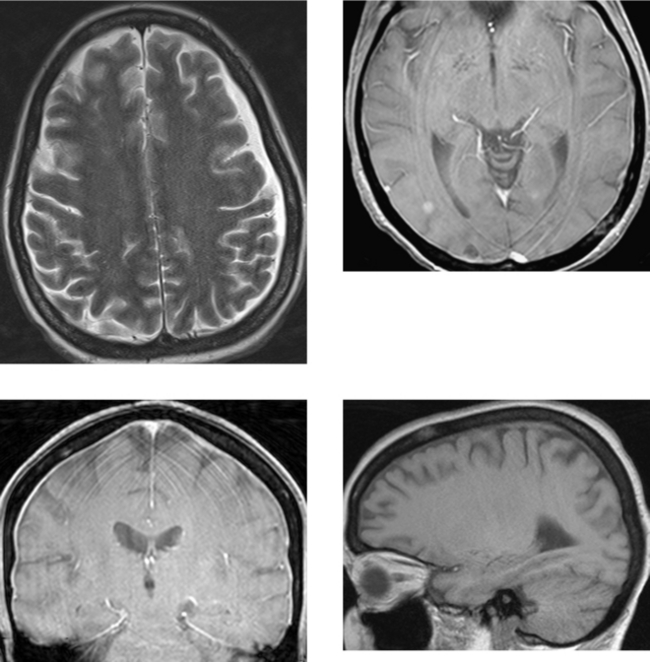
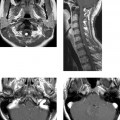
CASE 52 Aqueductal Stenosis
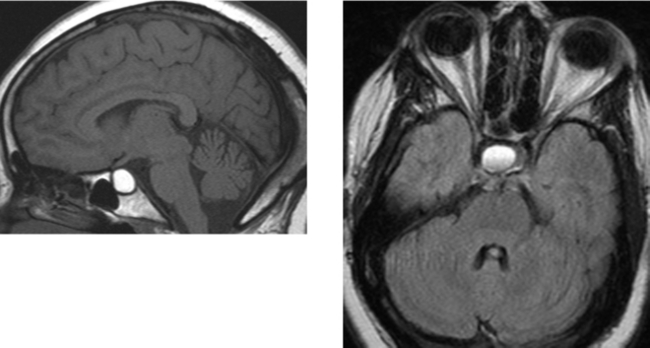
CASE 53 Rathke’s Cleft Cyst
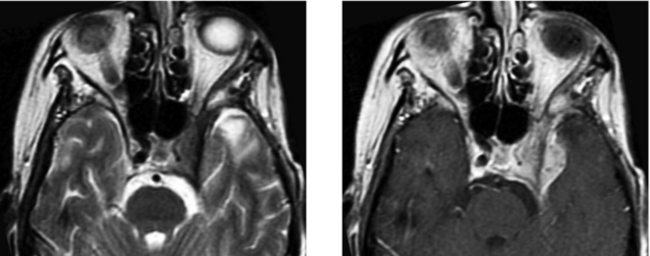
CASE 54 Optic Neuritis (Demyelinating Disease)
Al-Shafai, Mikulis DJ. Diffusion MR imaging in a case of acute ischemic optic neuropathy. Am J Neuroradiol. 2006;27:255-257.
Beck RW, Cleary PA, Trobe JD, et al. The effect of corticosteroids for acute optic neuritis on the subsequent development of multiple sclerosis. N Engl J Med. 1993;329:1764-1769.
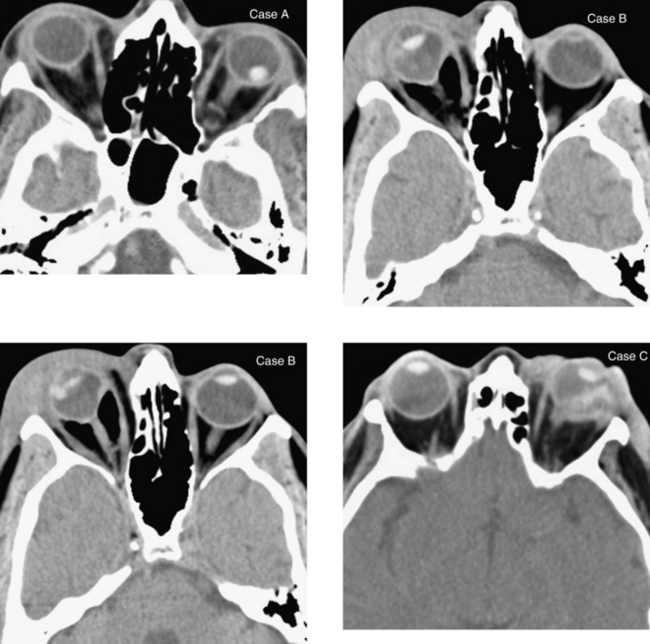
CASE 55 Ocular Trauma—Lens Dislocation and Globe Rupture
CASE 56 Developmental Venous Anomaly
CASE 57 Fibrous Dysplasia of the Calvaria
CASE 58 Cavernous Sinus Mass—Meningioma
Hirsch WLJr, Hryshko FG, Sekhar LN, et al. Comparison of MR imaging, CT, and angiography in the evaluation of the enlarged cavernous sinus. AJNR Am J Neuroradiol. 1988;9:907-915.
Hudgins PA. Imaging of the cavernous sinus: management of cavernous sinus pathology. Techniques in Neurosurgery. 2003;8:211-219.
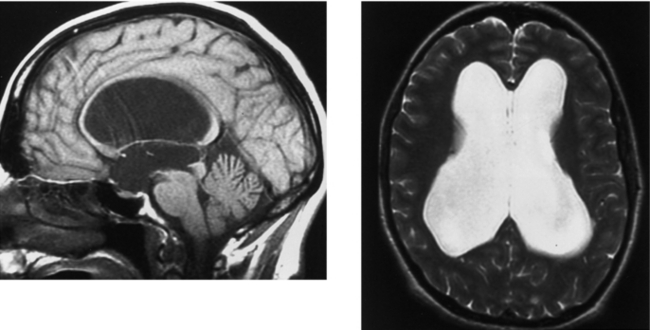
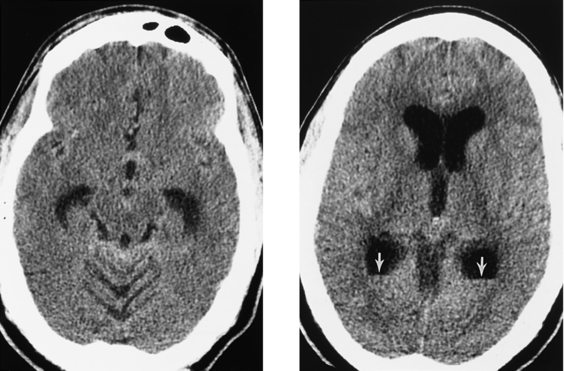
CASE 59 Pyogenic Ventriculitis with Acute Hydrocephalus
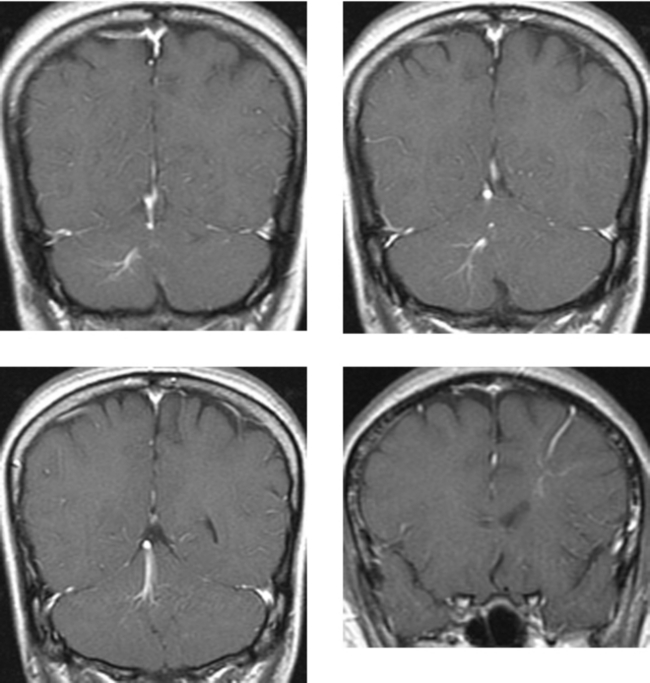
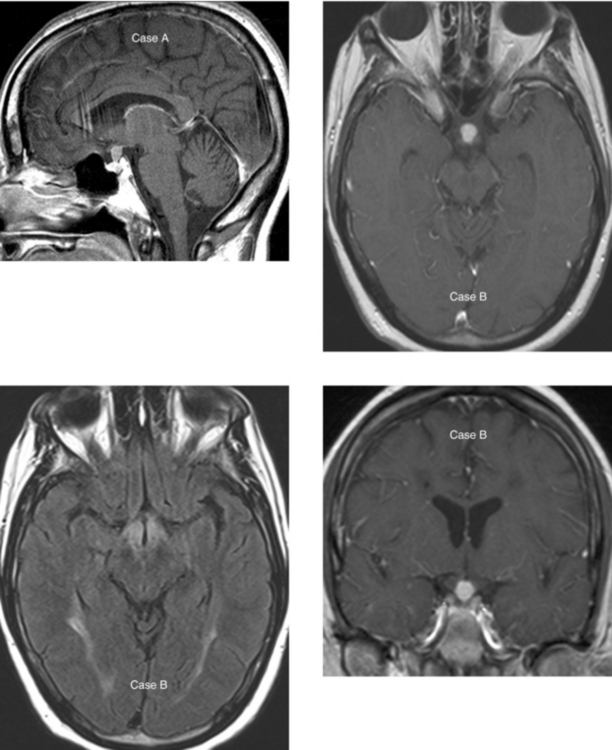
CASE 60 Lesions of the Pituitary Stalk and Hypothalamus: Case A—Sarcoidosis; Case B—Langerhans’ Cell Histiocytosis
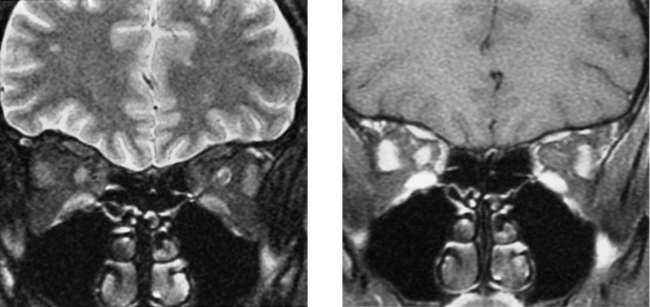
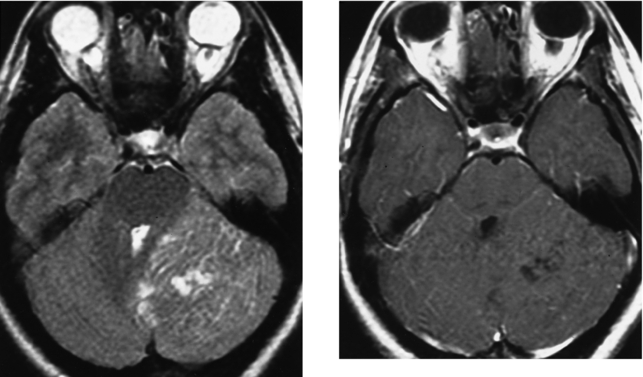
CASE 61 Lhermitte-Duclos Disease (Dysplastic Gangliocytoma of the Cerebellum)
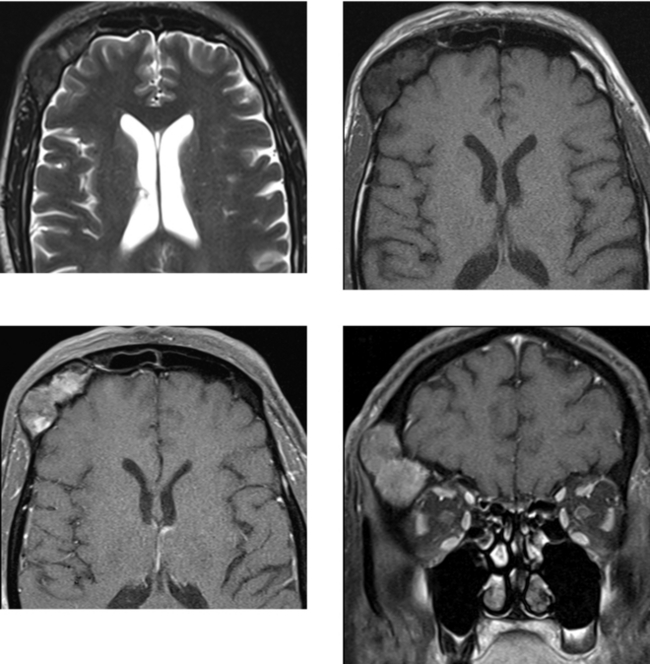
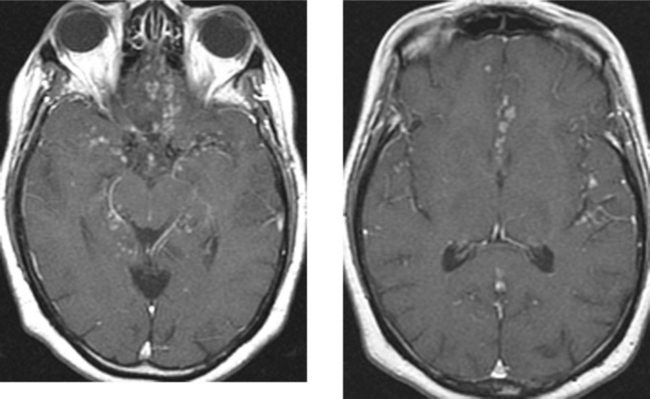
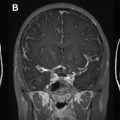
CASE 62 Basilar Meningitis—Sarcoidosis
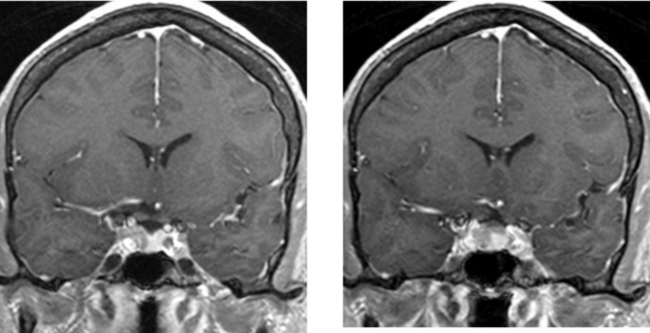
CASE 63 Pituitary Microadenoma
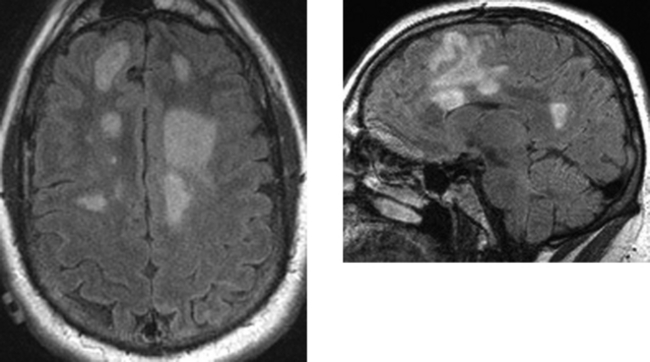
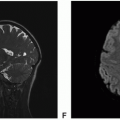
CASE 64 Multiple Sclerosis—Marburg Type
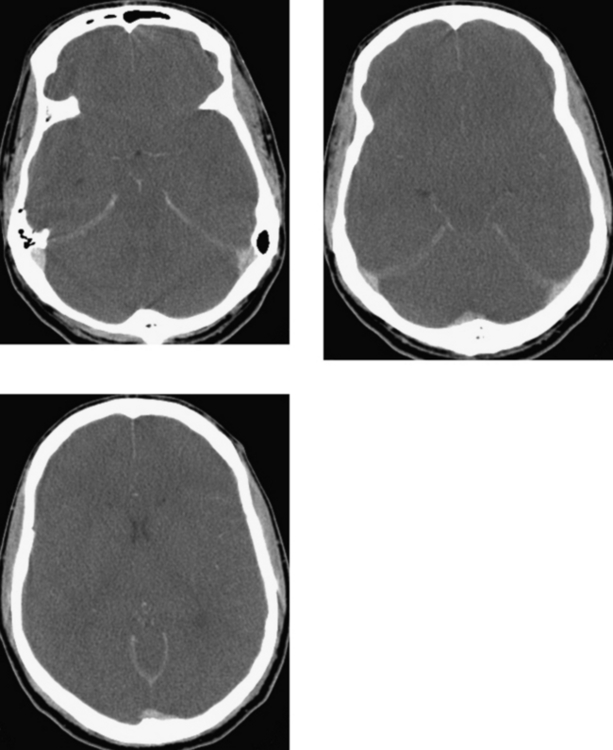
CASE 65 Transtentorial Herniation