Introduction
The development of focused assessment with sonography for trauma (FAST) over 30 years ago enabled clinicians to rapidly screen for injury at the bedside of patients, especially those hemodynamically unstable for transport to the computed tomography (CT) suite. The identification of free fluid within the peritoneal cavity, pericardium, and pleural spaces can be accomplished with point-of-care ultrasound (US) immediately upon patient arrival to the hospital. Other applications of FAST include detection of solid organ injury, pneumothorax, fractures, and serial examinations, as well as use in prehospital transport and multiple casualty settings as a triage tool. Before FAST, invasive procedures such as diagnostic peritoneal lavage and exploratory laparotomy were commonly utilized to diagnose intraabdominal injury (IAI). Today the FAST examination has evolved into a more comprehensive study of the abdomen, heart, chest, and inferior vena cava, and many variations in technique, protocols, and interpretation exist.
US was first utilized for the examination of trauma patients in the 1970s in Europe. It was not widely adopted in North America until the 1990s, during which time the FAST acronym was defined as “focused abdominal sonography for trauma.” As FAST evolved into a more comprehensive examination, the acronym was changed to “focused assessment with sonography for trauma.” Since then, FAST has become the common initial screening modality in trauma centers worldwide, and it is included in the Advanced Trauma Life Support (ATLS) program for evaluation of the hypotensive trauma patient. A unique aspect of FAST is that it is routinely utilized by radiologists, emergency physicians, surgeons, and paramedics with variable training and experience. Over time, a new role for FAST has evolved, in which its use in the evaluation of unstable, hypotensive trauma patients is emphasized. The most effective use of FAST has been rapid triage of hemodynamically unstable trauma patients to definitive intervention.
In the mid-2000s, the addition of US evaluation of the thorax to detect pneumothorax to the traditional FAST examination resulted in a new acronym, “e-FAST,” or extended FAST. Several other protocols have been developed for evaluation of shock, respiratory distress, and cardiac arrest, some of which feature echocardiography. The number of different protocols for evaluation of the critically injured or ill patient is a source of confusion, especially as even more protocols are developed with creative acronyms and abbreviations. In this chapter we will focus on the abdominal portion of the overall FAST examination, as point-of-care evaluation of the heart and lungs is covered in separate chapters.
Ultrasound Technique
The original FAST scan included views of the right upper quadrant, which included the perihepatic area and hepatorenal recess (Morison’s pouch), of the left upper quadrant encompassing the perisplenic view, the suprapubic view (pouch of Douglas), and later a subxiphoid pericardial view ( Fig. 15.1 ). The preferred initial site for detection of free fluid with FAST is the right upper quadrant view using a lower-frequency (3.5–5 MHz) curved array transducer. The liver serves as an acoustic window during insonation of the hepatorenal space and liver parenchyma. In the left upper quadrant view, the spleen is the target during examination of the splenorenal fossa and perisplenic area. Cephalad scanning enables visualization of the left pleural space. Moving the probe caudally brings the inferior pole of the left kidney and paracolic gutter into view. The perisplenic area may be inadequately scanned due to difficult physical access. Rolling the patient to the right side and/or having the patient take a deep breath is helpful in evaluating this area, as small amounts of free fluid may collect superiorly to the spleen. The suprapubic view enables visualization of the most dependent space in the peritoneal cavity. The transducer is placed above the pubic symphysis in a sagittal plane and swept side to side, then rotated transversely and repeated. Reverse Trendelenburg positioning may enhance the detection of free fluid in the pelvis. The visualization of small amounts of free fluid in the pelvis is aided by the presence of a full bladder. When free fluid is present, it is most frequently located posterior or superior to the bladder and/or the uterus. Free fluid in the pelvis can be missed when a Foley catheter is placed to empty the bladder, as the acoustic window for examining the pelvis is removed, limiting the sonographer’s ability to discern small amounts of pelvic fluid. Bowel gas, subcutaneous emphysema, and obesity represent common obstacles to full sonographic visualization.

The volume of free fluid necessary to enable detection with FAST is a well-known limitation. In one early study, the mean minimum detectable free-fluid volume in 100 patients undergoing diagnostic peritoneal lavage was 619 mL in the right upper quadrant view. Trendelenburg positioning may improve visualization of free fluid in the splenorenal and hepatorenal interface. FAST performed in the Trendelenburg position enables detection of smaller amounts of hepatorenal free fluid than supine. Even smaller volumes of free fluid are required for detection in the pelvic views of FAST, with median minimal volume of fluid of 100 mL. Scoring systems have been described in the past, and the common theme among these studies is the larger the amount and number of sites of free fluid, the greater the likelihood of injury or need for surgical intervention.
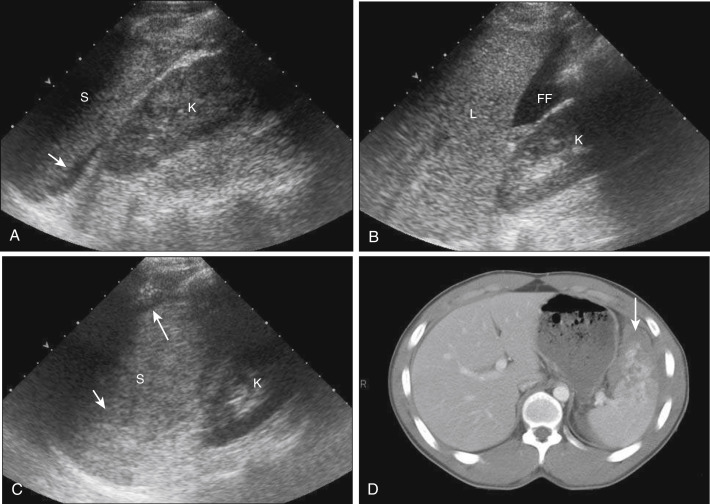
Hemoperitoneum
Free fluid detected by US is assumed to be hemoperitoneum, which usually appears anechoic or hypoechoic compared with adjacent solid organs. During prolonged periods, this hemorrhage may organize into clots and become more echogenic-appearing on US. In the absence of injury or other pathology, free fluid should not be found within the peritoneal cavity on US, with the exception of the suprapubic view: only small amounts of rectouterine (pouch of Douglas) free fluid in women of childbearing age should be detectable. These small free-fluid collections of up to 50 mL in the pouch of Douglas are considered physiologic, and amounts exceeding 50 mL should be regarded as pathologic in the setting of trauma. As the initial FAST represents a “snapshot” in time, serial examinations performed on stable blunt trauma patients may be useful ( Fig. 15.2 ). Examination after stabilization gives the sonographer more time for a comprehensive scan. With active intraperitoneal hemorrhage, the amount of free fluid should theoretically increase with time. Serial FAST examinations have been reported to decrease the false-negative rate by up to 50% and may be a logical alternative for stable trauma patients, patients with a sudden change in hemodynamic status or physical examination, and pregnant patients to mitigate radiation exposure.

False Negatives and Positives
The sensitivity of FAST ranges from 69% to 98% and specificity from 95% to 100% for detection of hemoperitoneum. The initial studies of FAST reporting high sensitivity compared FAST findings with patient outcome and not CT. Later studies comparing FAST with CT results showed lower sensitivity, largely due to the fact that CT detected isolated solid organ injuries without the presence of hemoperitoneum. Since then, more recent critical evaluations of FAST have appeared, highlighting its high false-negative rate in stable trauma patients. In hemodynamically stable patients, a negative FAST without follow-up CT may miss an IAI. Thus the potential for underdiagnoses of IAI with FAST is now well recognized. Clinical suspicion, mechanism of injury, and change in clinical examination or hemodynamic status should always be included in deciding upon further diagnostic testing in patients with negative initial FAST. For patients with negative FAST, observation, serial FAST, CT, or contrast-enhanced US may be chosen.
False-positive scans may result from detection of ascites, peritoneal dialysate, ventriculoperitoneal shunt outflow, polycystic ovarian disease, and ovarian cyst rupture. Massive intravascular volume resuscitation may result in a false-positive FAST examination from intravascular to intraperitoneal fluid transudation. Although free fluid detected by FAST in trauma patients is assumed to be hemoperitoneum, it can also represent injury-related urine, bile, and bowel contents. Patients with delayed presentation after trauma may have hemoperitoneum containing clots, which can have mixed echogenicity and be missed or misinterpreted. Perinephric fat, which widens the hepatorenal and splenorenal interface, may be misinterpreted as free fluid or subcapsular hematoma, also known as the “double-line” sign . Comparison views of each kidney may be helpful in these cases.
The Liver
Detection of liver injury, even in the absence of free fluid, is possible with point-of-care US. Although not included in the FAST protocol, careful insonation of the normally homogenous liver parenchyma for any irregularities may detect injuries such as lacerations, contusions, and hematomas. Ultrasound has been shown to have very high sensitivity for detection of grades III and higher liver injury. For parenchymal injuries detected with US, three distinct patterns are identified. The most common sonographic pattern is a discrete hyperechoic area visualized within the hepatic architecture, followed by a diffuse hyperechoic pattern ( Fig. 15.3 ). The least common pattern is a discrete hypoechoic focus. Hepatic injuries may be difficult to detect when the liver capsule remains intact. The liver has a greater volume than the spleen; thus small intraparenchymal lesions may be missed with the rapid FAST technique.

The Spleen
Rapid identification of spleen injuries is important due to the highly vascular nature of this organ and the potential for extensive and life-threatening intraperitoneal hemorrhage. The majority of spleen injuries have associated hemoperitoneum. However, if the capsule of the spleen remains intact after trauma, hemoperitoneum may not be detected. In these situations several distinct patterns of parenchymal appearance have been identified on US for spleen injuries. The most common sonographic patterns are diffuse heterogeneous (both hyperechoic and hypoechoic), discrete hyperechoic, discrete hypoechoic, and perisplenic crescent ( Figs. 15.4–15.6 ). More recently, contrast-enhanced US has been shown to be more sensitive in detecting spleen and other solid organ injuries compared with conventional sonography.


The Kidneys
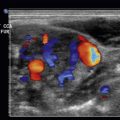
The kidneys are retroperitoneal structures, and unless significant trauma occurs directly to the kidney, it is unlikely that free fluid would be observed in the abdomen. In one study of isolated renal injury, free fluid was detected in only 7 of 20 patients. The majority of renal injuries occurs with concomitant other major organ injuries, such as splenic rupture, liver laceration, or tears of the bowel or mesentery that require operative repair. However, careful interrogation of the renal parenchyma may reveal hyperechoic, hypoechoic, and mixed abnormalities representing lacerations, contusion, and hematomas ( Figs. 15.7–15.10 ). Such findings, especially when hematuria is concurrently detected, should prompt further imaging with CT. The most common pitfall on US is interpretation of perinephric fat, which widens the hepatorenal and splenorenal interface. Perinephric fat may be misinterpreted as free fluid or subcapsular hematoma, also known as the “double-line” sign . Comparison views of each kidney may be helpful in these cases.