FDG-PET-CT in Head and Neck Cancer
Christina M. Thuerl
Hugh D. Curtin
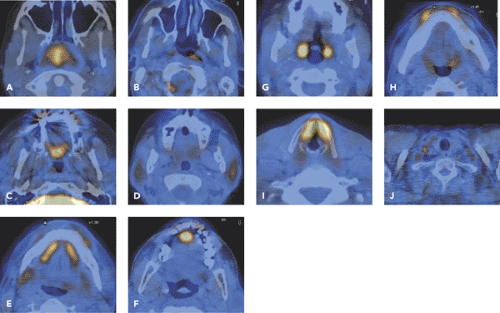
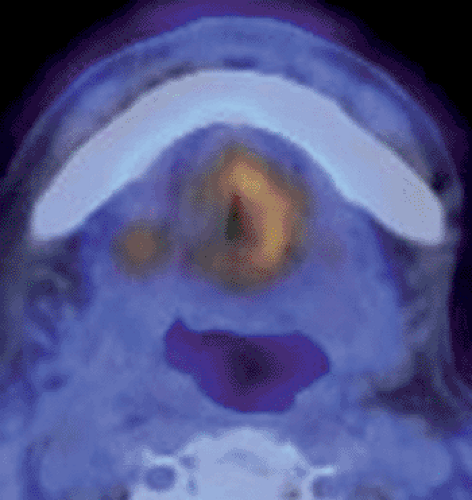
Head and neck cancer is an important topic in oncologic imaging, because imaging findings can aid significantly in the detection, staging, and treatment evaluation of these tumors. Positron emission tomography (PET) and PET–computed tomography (CT) have become routine imaging tools for the evaluation of patients with head and neck cancer, with fluorodeoxyglucose (FDG) as the most important tracer. For a correct evaluation of the head and neck region, knowledge about the physiological FDG uptake pattern (see Fig. 34.1), artifacts, and pitfalls is important. With the introduction of PET-CT, a spatially more accurate modality can localize increased FDG uptake in primary tumors with certainty. However, T staging of head and neck tumors seems to offer no advantage over conventional imaging methods. T staging by FDG-PET-CT has limitations in small T1 tumors and tumors with superficial spread. Perineural spread, which is common in adenoid cystic carcinoma, can be completely overlooked by FDG-PET-CT. Detection and staging of small tumors can be impaired in areas with physiological uptake of FDG, especially in areas with lymphoepithelial tissue (nasopharynx, palatine tonsils, tongue base).
The sensitivities and specificities of FDG-PET in detecting primary lymph node involvement range between 71% to 93% and 86% to 100% for PET and 53.1% to 82% and 57% to 87.8% for CT–magnetic resonance imaging (MRI). False-negative FDG-PET studies can occur if there is only a small tumor burden in metastatic nodes and also if necrotic nodes maintain only a small rim of viable tumor tissue, seen frequently in squamous cell carcinoma. These nodes can be completely missed by FDG-PET and unenhanced FDG-PET-CT alone.
A major advantage of whole-body FDG-PET-CT is that it improves the detection of distant metastases, second primary tumors, and local recurrence. As a rule, clinically detectable recurrent disease is extremely unlikely in the setting of an entirely negative PET-CT scan. False-positive findings are related to inflammation, infection, or radiation necrosis. First results suggest that the integration of FDG-PET-CT into the radiation treatment planning process may assist in better differentiating normal tissue from tumor-bearing tissues and in identifying areas of high risk for recurrence. An overview of the anatomy and the tumors of the oral cavity, pharynx, larynx, salivary glands, nasal cavity, and sinuses is provided, along with FDG-PET-CT examples of the different tumors.
Introduction
Head and neck cancer is the sixth most common cancer in the world, and in the United States it accounts for approximately 3% of all cancers in men and 2% of all cancers in women (1). Squamous cell carcinoma represents more than 90% of all head and neck cancers. The incidence rates are more than twice as high in men as in women and are greatest in men older than 50. The risk of malignancy is 6 times greater for smokers than nonsmokers. The synergistic effect of alcohol and smoking increases the risk of the disease 2.5 times more than the simple additive risk of either risk factor alone. Nasopharyngeal carcinoma is associated with Epstein-Barr virus. Human papillomavirus infection is another factor implicated in the development of oral cavity and oropharyngeal squamous cell carcinoma (2,3). Mutation of the tumor suppression gene p53 is one of the most common genetic alterations in squamous cell
carcinomas of the head and neck (4,5,6). Chewing betel nuts, particularly when mixed with tobacco, serves as a local irritant of oral mucosa and therefore a stimulant to the formation of malignancies. Wood dust and woodcarving have been implicated in the increased incidence of nasopharyngeal malignancies, as has the ingestion of smoked fish, particularly in parts of Asia.
carcinomas of the head and neck (4,5,6). Chewing betel nuts, particularly when mixed with tobacco, serves as a local irritant of oral mucosa and therefore a stimulant to the formation of malignancies. Wood dust and woodcarving have been implicated in the increased incidence of nasopharyngeal malignancies, as has the ingestion of smoked fish, particularly in parts of Asia.
Table 34.1 Overview of FDG Uptake in the Head and Neck | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||
Head and neck cancer is an important topic in oncologic imaging, because imaging findings can aid significantly in the detection, staging, and treatment evaluation of these tumors. Patients presenting with primary tumors that are confined at the time of initial diagnosis (T1-2NOMO) have an excellent cure rate. Unfortunately, at the time of initial diagnosis many patients already have regional nodal metastases (45%) or even distant metastases (10%) (7). For all stages combined, about 85% of persons with oral cavity and pharynx cancer survive 1 year after diagnosis. The 5-year and 10-year relative survival rates are 59% and 44%, respectively (1). Therefore, the major goals of the evaluation of patients with head and
neck cancer are locoregional staging, exclusion of distant metastases, and synchronous second primary tumors. Already in 1988, Minn et al. described increased uptake of fluorodeoxyglucose (FDG) in patients with tumors of the head and neck (8).
neck cancer are locoregional staging, exclusion of distant metastases, and synchronous second primary tumors. Already in 1988, Minn et al. described increased uptake of fluorodeoxyglucose (FDG) in patients with tumors of the head and neck (8).
Physiological FDG-Uptake and Artifacts in PET-CT of the Head and Neck
FDG is not specific for neoplastic processes in head and neck. It accumulates physiologically in various regions of head and neck (Table 34.1) (9). Low to strong FDG uptake occurs in the normal lymphoepithelial tissue of the nasopharynx and oropharynx (Fig. 34.1A,B), the palatine tonsils (Fig. 34.1H), and at the base of the tongue (Fig. 34.1I). Variable but usually low FDG uptake is visible in the salivary glands, which physiologically secrete low amounts of glucose (Figs. 33.21 and 34.1D,E). Muscular FDG uptake can be seen in the palate (Fig. 34.1C); in the floor of the mouth (Figs. 33.21G and 34.1E); in the tip of the tongue (Fig. 34.1F); in muscles of the face (Fig. 34.1H), including the masticatory muscles, neck (Fig. 34.1K), and larynx (Fig. 34.1J); in nervous patients; and in patients who speak during the FDG-uptake phase. However, physiological uptake in the laryngeal muscles is usually symmetric and can be discriminated from cancer. In patients with laryngeal nerve palsy, glottic muscle uptake on the healthy side can be observed (see Fig. 34.22). If patients do not close their eyes during the study, muscles of the eyes and eyelids will also show increased uptake.
Postsurgical changes that distort the normal anatomy after resection and surgical reconstruction can elicit atypical muscle activity (Fig. 34.2). Other reasons for FDG uptake not related to tumor are inflammation, infection, and radiation necrosis.
In patients with head and neck cancer, dental problems are common. If disease of the dental roots and/or periodontal space is present, the teeth will be surgically removed before starting radiation treatment. This will cause an inflammation reaction in the jaw, which can be visible in FDG-PET-CT for several weeks. Inflammation can mimic a malignant lesion, and it is important to interpret images in the light of adequate clinical information.
Dental metal work also causes artifacts. Nonremovable metal dentures, bridgework, and fillings will produce a defect in the emission image that can also be seen in the final attenuation-corrected image (9,10). However, most malignant lesions avidly take up FDG and therefore are usually identifiable without problems. In addition, attenuation correction by means of a CT scan can be deteriorated due to dental metalwork, which can mimic FDG
uptake in attenuation-corrected images (11). Measurement of SUV values can be influenced by these artifacts. Therefore, measurements of FDG concentrations in areas adjacent to nonremovable dentures may be of limited value. Based on our experience, we feel that additional viewing of the non-attenuation-corrected emission scans can render image interpretation of oral pathologies with PET more reliable.
uptake in attenuation-corrected images (11). Measurement of SUV values can be influenced by these artifacts. Therefore, measurements of FDG concentrations in areas adjacent to nonremovable dentures may be of limited value. Based on our experience, we feel that additional viewing of the non-attenuation-corrected emission scans can render image interpretation of oral pathologies with PET more reliable.
Imaging Goals
T Staging
The first goal of imaging studies is to determine the extent of the primary tumor, in particular with regard to structures whose involvement may alter the surgical approach. Since anatomical information is lacking, FDG-PET has only very limited value in T staging in head and neck cancer. But the introduction of PET-CT, which is a spatially more accurate modality, has meant that increased FDG uptake can be localized with certainty. However, in our experience T staging of head and neck tumors by FDG-PET-CT seems to offer no advantage over conventional imaging methods. Even in PET-CT, the exact size of the tumor is not demonstrated by the FDG uptake, since the elevated FDG activity appears as a spot with blurring.
Quantitative measurement of FDG uptake by means of the standard uptake value (SUV) or other indices is possible and is performed as part of a routine protocol in some institutions. No diagnostic threshold has been clearly established for distinguishing uptake in malignant tumors from that in benign tissues, and in cancer cases no cutoff has been established for defining subgroups of differing prognoses. Previous clinical series suggest a wide range of cutoff values (3.5 to 10) predicting a worse prognosis (12,13,14,15,16,17).
T staging of head and neck tumors by FDG-PET-CT has limitations in small T1-tumors and tumors with superficial spread. These tumors can be completely missed in FDG-PET-CT (18). Perineural spread, which is common in adenoid cystic carcinoma, can be completely overlooked by FDG-PET-CT. Detection and staging of small tumors can be impaired in areas with physiological uptake of FDG (see Fig. 34.1), especially in areas with lymphoepithelial tissue (nasopharynx, palatine tonsils, tongue base) (19). FDG-PET-CT has also limited value in defining intracranial extension of tumors because of the lack of contrast between the FDG avid brain and tumor tissue. For preoperative staging, which includes a depiction of the relationship of the tumor to vessels and the correct delineation of infiltrated structures in the complex head and neck region, contrast-enhanced CT or MRI is mandatory.
N Staging
An important goal of PET-CT is the assessment of the nodal status in the neck. The presence of nodal metastases is an independent prognostic factor for survival in patients with head and neck cancer. It decreases the overall survival by approximately one half (20). The prognosis worsens additionally with the number of lymph nodes involved (21), with extracapsular spread of nodal disease (22,23), and with metastases located in the lower neck (24). The presence and extent of nodal metastases may affect patient management. Therefore, an accurate nodal staging of the neck is important.
The sensitivities and specificities of FDG-PET in detecting lymph node involvement range between 71% and 93% and 86% and 100% for PET and 53.1% and 82% and 57% and 87.8% for CT and MRI (18,25,26,27). False-negative FDG-PET studies may occur if there is a small tumor burden in metastatic nodes and if also necrotic nodes maintain only a small rim of viable tumor tissue, which is common in squamous cell carcinoma. These nodes can be completely missed by FDG-PET and unenhanced FDG-PET-CT alone (Fig. 34.3). Therefore, FDG-PET-CT should be performed with contrast material to prevent the missing of small necrotic lymph nodes. In contrast, in patients who present large FDG avid lymph nodes in the neck without any central necrotic area, a differential diagnosis of lymphoma should be considered. Nodal metastases in close proximity to the primary tumor may not be detectable as separate hypermetabolic foci when the primary shows very intense tracer uptake (Fig. 34.4). We have observed that FDG-PET-CT cannot differentiate clearly between necrotic lymph node metastases and branchial cleft cysts, because branchial cleft cyst can contain lymphoid tissue (28), which is FDG avid.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree