Normal First-Trimester Ultrasound Appearance
Pelvic ultrasound is the key imaging modality in the diagnosis of early pregnancy and its associated complications. Both transabdominal and transvaginal sonography (TVS) techniques are used.
Gestational Sac
Intradecidual Sign
The intradecidual sign refers to an eccentric, extraluminal, rounded, cystic structure located within the endometrium. It is the earliest imaging sign of an intrauterine pregnancy (IUP) on TVS and is observed as early as 4½ weeks of menstrual age.
Double Decidual Sac Sign
The hyperechogenic peripheral decidua vera and the inner decidua capsularis with intervening anechoic endometrial lumen is seen on TVS at about 5 menstrual weeks ( Fig. 24.1 ).

The gestational sac (GS) is composed of anechoic amniotic fluid and chorionic extraembryonic coelom, which may contain low-level echoes.
Yolk Sac
With TVS, the yolk sac (YS) is usually visualized within the extraembryonic coelom at approximately 5½ weeks or 8-mm mean sac diameter (MSD). It appears as a thin-walled, circular structure with an anechoic center. A normal YS measures less than 5.6 mm internal diameter between 5 and 10 weeks and starts to regress by 11 weeks. The YS is no longer seen after the amniotic cavity expands to obliterate the chorionic cavity by 14 to 16 weeks.
Embryo
The embryo is first visible at approximately 6 weeks of gestational age as a 1- to 2-mm structure at the periphery of the YS. The length of the embryo is measured from the head (crown) to the buttocks (rump), hence the term crown–rump length (CRL), which is the most accurate measurement of gestational age through the first 12 weeks of pregnancy. The embryo should be visualized when the MSD is at least 25 mm ( Fig. 24.2 ).

The embryo resides within the amniotic cavity. It is possible to observe cardiac activity in embryos as small as 1 to 2 mm. However, absence of cardiac activity in embryos smaller than 4 mm may also be normal. The embryonic heart rate accelerates over the first 6 to 8 weeks of gestation, with the lower limit of normality near 100 beats per minute at 6.2 weeks of gestation and 120 beats per minute at 6.3 to 7.0 weeks of gestation.
Embryonic morphology is rather featureless until 7 to 8 weeks, when the spine can be visualized. At approximately 8 weeks of gestation, the head curvature can be separated from the body and the four limb buds become apparent. The rhombencephalon, which is the developing hindbrain, is a prominent landmark at 8 to 10 weeks of gestation, appearing as an anechoic, round structure within the head.
Twin Pregnancy
It is important to determine the number of fetuses and their chorionicity and amnionicity in the first trimester, when it is easiest.
Dichorionic diamniotic: The twin peak sign is reliable evidence of dichorionicity. Both the amnions and the chorions reflect away from the placental surface, creating a potential space into which villi can grow. There is a thick intertwin membrane ( Fig. 24.3 ).

Fig. 24.3
Diamniotic dichorionic gestation. Thick intertwin membrane ( yellow arrow ) and twin peak sign ( white arrow ).
Monochorionic diamniotic: A single layer of continuous chorion limiting villous growth. There is a thin intertwin membrane separating the two amniotic cavities ( Fig. 24.4 ).

Fig. 24.4
Diamniotic monochorionic gestation. Thin intertwin membrane ( arrow ).
Monochorionic monoamniotic: No intertwin membrane ( Fig. 24.5 ).

Fig. 24.5
Monoamniotic monochorionic gestation. No intertwin membrane.
Chorionic Bump
The chorionic bump is a focal solid or complex protuberance from the choriodecidual region bulging into the GS ( Fig. 24.6 ). Harris et al. identified this sign in 0.7% of 2178 early obstetrical sonograms and noted that 50% of these pregnancies aborted—a pregnancy failure rate four times that of the general population control group.

Based on the sonographic evolution of the chorionic bump on follow-up studies and pathologic investigation of abortuses, the chorionic bump likely represents a small subchorionic bleed.
Subchorionic Hemorrhage
Intrauterine hematomas, a common ultrasound finding associated with first-trimester bleeding, have a reported incidence between 4% and 22%. Subchorionic hemorrhage is the most common type of intrauterine chorionic bleed and is thought to result from partial detachment of the trophoblast from the uterine wall, with blood dissecting between the chorion and the decidual layer of endometrium. When the hematoma dissects into the endometrial cavity, the patient can present with vaginal bleeding.
Subchorionic bleeds are graded into small, medium, and large according to their sizes relative to GS circumference. One large retrospective review reported a rate of pregnancy loss of 7.7% for small hematomas (less than one-third the circumference of the GS), 9.2% for medium hematomas (encompassing one-third to one-half the circumference of the GS), and 18.8% for large hematomas (encompassing at least two-thirds the circumference of the GS).
Subchorionic hemorrhage has a worse prognosis when associated with advanced maternal age or early gestational age. A subchorionic hemorrhage may progress into an abruption when the bleed extends behind the placenta.
Subchorionic hemorrhage can be crescentic, ovoid, linear, or curvilinear, and its echogenicity is dependent on the stage of the hemorrhage. It is echo-poor in the hyperacute setting, transitioning to hyperechogenic as the hematoma organizes and subsequently decreasing in echogenicity as the hematoma undergoes hemolysis and liquefaction ( Fig. 24.7 ).

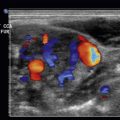
Due to its variable appearance, a first-trimester subchorionic hematoma can be confused with normal first-trimester incomplete chorioamniotic fusion, an intrauterine mass, a vanishing twin, or slow flow within perigestational veins. The latter condition may be recognized by detection of slow-moving particles on grayscale or color Doppler imaging.
The majority of subchorionic hematomas are small, regress spontaneously, and do not result in pregnancy loss. Larger or persistent hemorrhages tend to have worse prognoses.
Miscarriage
The sonographic appearance of a normal IUP follows a predictable pattern during the 5- to 7-week period. Any substantial deviation from this pattern raises concern that the pregnancy has already, or will soon, fail. An important aspect of ultrasound in early pregnancy is distinguishing between the abnormal sonographic findings that are definitive for pregnancy failure and those that are suspicious but not definitive, requiring follow-up testing to establish a definitive diagnosis.
Current criteria for definitive pregnancy failure on transvaginal ultrasound are the following:
- •
Nonvisualization of cardiac activity in an embryo whose CRL is at least 7 mm ( Fig. 24.8 )

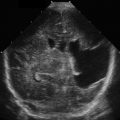
Fig. 24.8
Embryonic demise. No cardiac activity in this embryo with a CRL of 22 mm.
- •
Nonvisualization of an embryo in a GS whose MSD is at least 25 mm
- •
Nonvisualization of an embryo at least 2 weeks after a scan that showed a GS without a YS
- •
Nonvisualization of an embryo at least 11 days after a scan that showed a GS with a YS
Findings that are suspicious but not diagnostic of pregnancy failure include:
- •
Failure to visualize cardiac activity in an embryo whose CRL is less than 7 mm
- •
Failure to visualize an embryo in a GS whose MSD is 16 to 24 mm
- •
Enlarged YS >7 mm ( Fig. 24.9 )