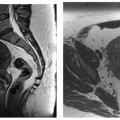
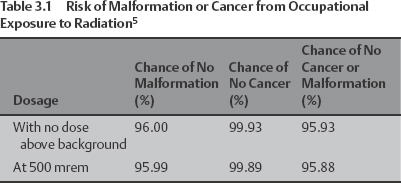
3 Female Physicians in Interventional Radiology Meridith Englander What justifies a chapter in this book about women in interventional radiology? What makes us so special? It is unlikely that anybody has ever been asked to write a chapter entitled “Male Physicians in Interventional Radiology” or that one even needs to be written? Yet one about women seems timely and necessary. Who are we? How did we get here? Where are we going? Only 8% of the people practicing interventional radiology (IR) today are women and only 2% of practicing women radiologists list themselves as interventional radiologists. That is 400 women in the United States.1 This number is so small that it is quite possible that one practicing female interventionalist may not even know another practicing female interventionalist. What we share in common is that we have all chosen a career that is challenging, exciting, demanding, and very satisfying. We are researchers, clinicians, and teachers. Importantly, we are also daughters, mothers, wives, and partners. So again, why do we need a chapter about women in IR? This chapter was written to give a voice to all of the women in IR and to all women thinking about a career in IR. When the Society of Cardiovascular and Interventional Radiology (SCVIR) was founded in 1973, there were 57 founding fellows. Three of these individuals were women, including Helen Redman, Ethel Finck, and Renate Soulen. They loved their jobs, yet faced many challenges because of their gender. They were different because they were women in a field dominated by men. In the early days of SCVIR, gender was not a significant issue. Everyone was involved in a revolutionary career, which was defining a new specialty. Therefore, individuals were valued based on their contribution to the field. At home institutions, however, the environment was not as accepting. Male colleagues earned more money for similar work, doctors’ bathrooms were for men only, and child care responsibilities were not understood. Despite these challenges, the early female interventionalists had productive careers and subsequently served as important role models for the next generation, including Arina van Breda, who served as the first female president of SCVIR in 1992. It seems that as a medical specialty, IR is quite accepting of women. This may be due to the unique nature of this field. Just past its infancy, the old boy network within IR is actually not that old. Also, because the current Society of Interventional Radiology (SIR) is small, many women have access to the network of people that are at its center. SIR is relatively blind to a member’s gender and in fact, does not track gender on any membership materials. Despite the fact that women attend national society meetings and genuinely feel that they are active contributors to the specialty of interventional radiology, they are still often facing difficulties in the comfort of their own practices. When trying to understand why there are so few women entering IR, one only has to look at the issues facing women today and wonder why, at this time, issues that should not be issues are issues. Women interventional radiologists face challenges including pregnancy and child rearing, social issues, and occupational issues such as salary inequity, obstacles to promotion, and relationships with patients and staff. Some of these challenges are unique to IR; nevertheless, some are shared by female physicians from many different specialties. In this chapter, I will discuss these challenges and others that may be serving as a barrier to women considering entering the field of IR. Women get pregnant and men do not. This clear, single fact underlies many of the different work-related issues facing men and women. Childbearing is a woman’s responsibility and it is being pregnant, having children, and raising them that create a great deal of gender-related tension in the workplace. During pregnancy, there are many potential threats to a woman and her fetus in the IR suite, including exposures to radiation, chemicals, and blood-borne pathogens. Despite the rumors and misconceptions, the risks to a pregnant interventionalist are minimal and should not prompt a woman with plans for a future pregnancy from avoiding IR as a career. To put the risk of radiation exposure into perspective, one must first consider the normal background exposure in our environment that all people are exposed to on a regular basis. Radon alone contributes a mean exposure of ~200 millirem (mrem)/year; some areas have considerably higher levels. Cosmic radiation contributes an additional 100 mrem/year. Consumer products including building materials, luminous watches, and smoke detectors contribute ~9 mrem/year. A single cross-country flight from New York to Seattle exposes an individual to 6 mrem.2,3 The difference between living in Miami and living in Denver adds ~50 mrem/year. When one considers this normal exposure, it is estimated that the average fetal dose over the course of a pregnancy approaches 75 mrem from these background sources. Radiation risks fall into two categories: stochastic and nonstochastic. Nonstochastic risks are predictable and include miscarriage, mental retardation, congenital malformations, and growth restriction. The dose threshold for these effects is much higher than 2 rem. This dose is assumed, but there has been no definitive data demonstrating fetal harm at radiation dose levels below 2 rem. The stochastic risks occur unpredictably and later in life. Cancer, and specifically childhood leukemia, is the concerning outcome from fetal radiation exposure. Unfortunately, there are no clear threshold doses for these effects. The U.S. Nuclear Regulatory Commission Regulatory Guide (NRCP) has issued guidelines, setting the limit for occupational exposure to ionizing radiation for pregnant women at 500 mrem for the duration of the pregnancy, with a one monthly equivalent dose of 50 mrem (0.5 millisievert [mSv]).4 Table 3.1 is helpful for estimating the additional risk from occupational exposure to radiation. There is an increased probability of malformation or childhood cancer with a significant radiation dose to the fetus. From the data in this table, there is a 4.07% chance of childhood cancer or congenital defect. With radiation exposure, this percentage chance increases to 4.12%, which translates to a risk of 0.05%. Wagner et al5 considered the above data and offered the opinion that irrational exaggeration of the potential effects of prenatal radiation will significantly alter the contribution that women will make to the radiologic profession, and it could conceivably be used as a basis for reproachable practices of job discrimination. Wagner et al5 also evaluated the gonadal dose associated with standard radiologic procedures, as outlined in Table 3.2. The conceptus dose is assumed to be one-half the gonadal dose based on literature examining computed tomography (CT), which shows internal radiation to be one-half of skin dose. Faulkner et al6 used phantom data to show that actual fetal dose is about one-half of underapron exposures.
Pregnancy Issues
Radiation Exposure
| Procedure | Radiation Exposure |
| Cardiac catheterization | 0.2–10 mrem |
| Renal angiogram | <0.12 mrem |
| Cerebral angiogram | 0.20 mrem |
| Venogram | 0.33 mrem |
Marx et al7 performed a prospective study looking at radiation exposure in 30 interventional radiologists over a 2-month period. The mean projected yearly dose (PYD) overlead was 49.1 mSv. For radiologists performing more than 1,000 cases per year, this dose increased to 66.6 mSv. The underlead PYD was 0.9 mSv on average. For radiologists wearing 0.5-mm-thick lead, the underlead PYD was 1.3 mSv. For those wearing 1.0-mm-thick lead, the underlead PYD was only 0.4 mSv. When converted to mrem, the average underlead exposure in this population was 40 mrem. This study demonstrates that wearing an extra layer of lead significantly reduces the underapron radiation exposure.
Nikalson et al8 further evaluated Marx’s data in 28 interventional radiologists, looking at the effective dose resulting from exposure to radiation. Their evaluation showed that the mean annual effective dose is 3.16 mSv (316 mrem), far below the NCRP limits. The maximum dose received by one of the study subjects was 10.1 mSv (1010 mrem). Assuming that these evaluations can be projected onto the general population of interventional radiologists, it is clear that radiation doses are generally small. Even so, there are outliers. Individuals should therefore keep careful track of their own exposures, before and during a pregnancy.
Other than monitoring exposure, there are proactive ways to minimize radiation exposure, which are well known to most interventional radiologists. Schueler et al9 evaluated operator exposure during IR procedures. She found that operator dose is largely a factor of scatter, which increases with input dose and the use of image filters. Patient size is most important as the scatter dose is 2 to 4 times higher with an obese patient. Decreasing the pulse rate directly lowers radiation exposure. The use of undertable skirts and ceiling shields, as well as increasing the distance from the beam decrease operator dose.
Adler et al10 authored a position article for the American Association of Women Radiologists (AAWR) in 1986. The authors stated that radiation risk for a conceptus is theoretical, but they recommended counseling for all women entering radiology as a profession and that they should be willing to accept the theoretical risks involved in fluoroscopy.
Methylmethacrylate Exposure
For women performing vertebroplasty and kyphoplasty procedures, methylmethacrylate exposure may be concerning due to its potential harmful effects during pregnancy. Polymethylmethacrylate (PMMA) is a volatile acrylic monomer. It has proven to be toxic to many organ systems of laboratory animals exposed to extremely high doses.
In the early 1970s, Singh et al11 studied the effects of intraperitoneal exposure of methacrylic acid in gestational rats. These rats showed slightly worse outcomes than those exposed to saline. McLauglin et al12 exposed pregnant mice to PMMA vapor for 2 hours twice daily from day 6 to day 15 of their pregnancy. No statistically significant difference between the two groups was detected. There was no increase in miscarriage rate or rate of subsequent malformations. Despite these conflicting studies, pregnant women have been virtually banished from operating rooms when PMAA is being mixed and used during surgical procedures. The Occupational Health and Safety Administration (OSHA) has set standards for occupational exposure. For any 8-hour work shift, exposure shall not exceed 100 ppm. Cloft et al13 measured methylmethacry-late (MMA) vapors in the room during the mixing of 20 mL of PMMA for vertebroplasty procedures. Ten samples were obtained during five procedures and all values were below detectable levels of 4.8 ppm.
Linehan looked at the serum and breast milk concentrations in orthopaedic surgeons after exposure to PMMA during a hip arthroplasty.14 No serum or breast milk samples demonstrated evidence of methacrylic acid at the 0.5-part-per-million level and no levels were higher than in the control group without immediate PMMA exposure. PMMA is rapidly cleared from blood through the lungs. Despite this, these authors reported the results of a survey of female orthopedic surgeons showed that 38% left the operating room during the cement phase of surgery while pregnant and 16% left while breastfeeding.
So what does this mean to an interventional radiologist? Again, there is a very low risk to a fetus if an interventional radiologist is involved in a vertebroplasty or kyphoplasty procedure during pregnancy.
General Anesthesia Gases Exposure
The gases used in general anesthesia can pose a threat to a pregnant woman who is occupationally exposed. Nitrous oxide is a known teratogen. This is based on studies that have shown a significantly higher rate of miscarriages in operating room nurses as compared with general duty nurses and in anesthesiologists as compared with pediatricians.15,16
Today, all anesthesia carts are installed with scavenging devices. These are filters on the outgoing ventilation tube that capture the exhaled anesthetic gases. The result is significantly decreased exposure for personnel in the room. In fact, the levels of toxic anesthetic gases can be brought to essentially nothing. However, there are many factors that undermine the effectiveness of these devices. If the endotracheal tube cuff is not inflated, gases will leak out. This is almost always the case with pediatric patients. In addition, there are a few times during a case when the inflow gases are disconnected from the patient, but the anesthetics are not turned off. This most often happens when the patient is being moved, if the patient needs to be manually ventilated, or when a case has been completed.
Fortunately, exposure to an interventional radiologist working with a general hospital population should be minimal and occasional. To minimize exposures, pregnant women should make sure that the anesthesiologist knows that she is pregnant and does not leave the nitrous oxide on if there is a chance for someone other than the patient to be exposed. Many anesthesiologists will avoid caring for pediatric patients when pregnant. Therefore, when feasible, it may be a good practice for a pregnant interventionalist to avoid general anesthesia cases on pediatric patients.
Blood-borne Pathogen Exposure
Exposure to blood-borne pathogens is a risk that physicians assume every time they work with a needle that is entering or has entered a patient. Human immunodeficiency virus (HIV) and hepatitis B and C viruses (HBV and HCV) are documented to be spread from patient to health care provider through needle sticks. The risk of transmission of HIV from a percutaneous exposure is estimated to be 0.3%. An increased risk is associated with large bore needles, whether the needle had been in a blood vessel, the depth of penetration of the needle, and the patient’s viral load. Postexposure prophylaxis is recommended for health care workers exposed to infected or potentially infected patients, with two or three agents for a course of 4 weeks. The most common side effects of these agents include nausea and vomiting, fatigue, and serious drug interactions.
The data regarding the safety of antiretroviral agents used during pregnancy are limited. Some agents are documented teratogens. Others are associated with increased risks of hyperbilirubinemia and renal stones, in the mother and fetus. Neurologic disease and death has been reported in uninfected children whose mothers had taken antiretrovirals to prevent perinatal transmission.17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree