Outline
Assignment of Gestational Age, 119
First Trimester Dating, 119
Second and Third Trimester Dating, 119
Fetal Weight Estimation and Weight Percentiles, 123
Abnormal Fetal Growth, 126
Fetal Growth Restriction and Small for Gestational Age Fetuses, 126
Macrosomic and Large for Gestational Age Fetuses, 127
Fetal Anomalies Associated With Abnormal Biometry, 127
Conclusion, 128
Summary of Key Points
- •
In the first trimester, gestational age should be assigned to the pregnancy based on sonographic findings or mean sac diameter prior to the visualization of the embryo and by embryonic or fetal crown-rump length (CRL) thereafter.
- •
In the second trimester, gestational age should be assigned based on head measurements that take into account head shape—namely, the corrected biparietal diameter or head circumference (HC)—or a composite age formula.
- •
By the latter part of the third trimester, neither dating by ultrasound nor dating by last menstrual period (LMP) is very accurate.
- •
Once gestational age has been assigned by an accurate method, such as sonography, the pregnancy should not be redated nor should the estimated due date be changed, because the earlier the gestational age is determined, the more accurate the dating of the pregnancy.
- •
Estimating fetal growth is best performed through estimating fetal weight and weight percentile, starting in the latter part of the second trimester and during the third trimester.
- •
The diagnosis of fetal growth restriction (FGR) should be suspected if the estimated weight falls below the 10th percentile for gestational age.
- •
The diagnosis of fetal macrosomia is suspected when the estimated fetal weight (EFW) is greater than 4000 g in a diabetic patient and above 4500 g in a nondiabetic patient.
- •
The diagnosis of a large for gestational age fetus is suspected when the EFW is above the 90th percentile for gestational age.
- •
In addition to its role in assessing gestational age and monitoring growth, fetal biometry is also important for identifying fetal abnormalities that are characterized by abnormal size of specific body parts, such as long bones with skeletal dysplasias.
Sonographic measurements of fetal structures provide an accurate means of determining the age of a pregnancy, estimating fetal weight, and assessing the normality of a number of fetal body parts. This chapter will discuss various fetal measurements and how they are used to date pregnancy, monitor fetal growth, diagnose fetal growth disturbances, and diagnose fetal abnormalities that are characterized by abnormal size of specific fetal structures.
Gestational age is the term most commonly used for specifying the age of a pregnancy. Prior to the advent of sonography, gestational age referred to the time elapsed since the first day of the woman’s last menstrual period (LMP). This is also termed menstrual age . With the development of means of dating pregnancies that are often more accurate than LMP, the term gestational age is no longer tied to the LMP. Instead, it refers to the time since the estimated conception date plus 2 weeks. Because women typically conceive at or close to 2 weeks after their LMP, gestational age and menstrual age are generally the same, but gestational age is a more accurate measure of the age of the pregnancy than is menstrual age in a woman with irregular cycle length. Full term is 40 weeks’ gestational age. The estimated due date (EDD) or estimated date of confinement (EDC) is calculated as the date at which the gestational age of a pregnancy will reach 40 weeks.
Another term sometimes used to date pregnancy is conceptional age , defined as the time since the date of conception. In some situations, such as in patients conceiving through assisted reproductive techniques (ART), conceptional age can be determined very accurately. In these cases, gestational age is equally accurate, because it is equal to the precisely known conceptional age plus 2 weeks. To avoid using different terms for dating pregnancies in ART patients, the term gestational age is the preferred term for dating all pregnancies, regardless of the mode of conception.
Accurate dating of pregnancy is extremely important for managing the obstetric patient, as many clinical decisions during pregnancy are dependent on gestational age. In the first trimester, the timing of prenatal testing for fetal chromosomal abnormalities is gestational age dependent. For assessment of some fetal structures, gestational age must be taken into account when distinguishing some normal from abnormal findings. For example, protrusion of intra-abdominal contents into the base of the umbilical cord can be a normal finding prior to 12 weeks’ gestation (physiologic bowel herniation) but is abnormal in the second trimester, when it represents an omphalocele. In the second trimester, selecting the best time to perform the sonographic fetal survey to assess for anomalies requires knowledge of the gestational age. Accurate dating is also important to determine if a fetal structure is abnormal in size. For example, if the femur is small for gestational age, concern for Down syndrome or a skeletal dysplasia should be raised. In the third trimester, accurate dating is needed to diagnose and manage preterm labor and to diagnose postterm pregnancies and determine when intervention is required.
Accurate assignment of gestational age is also essential for assessing fetal growth, because a key method for assessing growth is determining whether the EFW is within the normal range for gestational age or abnormally low or abnormally high. Abnormally small fetuses may require increased prenatal surveillance and possibly early delivery. Cesarean delivery may be appropriate for fetuses measuring abnormally large for gestational age.
Assignment of Gestational Age
The gestational age of a pregnancy can be assigned based on either clinical factors or sonographic findings. In general, clinical factors, such as LMP or uterine size estimation, are less accurate than ultrasound for dating pregnancies. Dating based on LMP is fraught with inaccuracies, including incorrect recall, irregular menstrual cycles, menstrual cycles longer or shorter than 28 days, and variable timing of ovulation during the cycle. Dating based on physical examination assessment of uterine size is even less accurate than LMP, because the assessment of uterine size is affected by body habitus as well as myomas and other uterine abnormalities.
Dating by ultrasound, particularly before the third trimester, is generally more accurate than clinical dating by LMP or physical examination. One exception in which clinical information is more accurate than ultrasound for dating is in pregnancies conceived by ART. Such pregnancies can be dated very accurately because the exact date of conception is known. Based on that date of conception, gestational age is assigned as the number of weeks since known conception plus 2 weeks.
Once gestational age has been assigned by sonography or by clinical information in an ART patient, the pregnancy should not be redated nor should the EDD be changed. This is because the earlier in pregnancy the gestational age is determined, the more accurate the dating of the pregnancy. Selecting the appropriate sonographic method for dating pregnancy depends on how far along the pregnancy is, and therefore, dating for each trimester will be discussed separately.
First Trimester Dating
Early in the first trimester, before the embryo is visible, gestational age can be assigned based on transvaginal sonographic findings. The earliest sonographic finding of pregnancy is a small rounded intrauterine fluid collection in the central portion of the uterus. The fluid collection may or may not demonstrate the intradecidual sign or the double sac sign. When ultrasound demonstrates an intrauterine fluid collection with no visible yolk sac or embryo, the pregnancy can be accurately assigned a gestational age of 5.0 weeks. When the fluid collection contains a yolk sac but no embryo, the pregnancy can be accurately assigned a gestational age of 5.5 weeks. The presence of a small embryo, less than 2 mm in size, with the embryonic heartbeat visible adjacent to the yolk sac, can be accurately dated as 6.0 weeks’ gestation ( Fig. 6-1 ). The accuracy of these early sonographic milestones for dating pregnancy is ±0.5 week.

An alternate method for dating early pregnancy is to measure the mean sac diameter of the gestational sac. This is done by averaging the sagittal, coronal, and anteroposterior measurements of the fluid component of the gestational sac ( Fig. 6-2 ) and assigning gestational age based on published tables ( Table 6-1 ) or formulas. Dating by mean sac diameter very early in pregnancy has similar accuracy to dating by sonographic milestones. However, once the embryo is large enough to measure, dating based on the size of the embryo is more accurate than using the mean sac diameter.

| Mean Sac Diameter (mm) | Gestational Age (Weeks) * |
|---|---|
| 2 | 5.0 |
| 3 | 5.1 |
| 4 | 5.2 |
| 5 | 5.4 |
| 6 | 5.5 |
| 7 | 5.6 |
| 8 | 5.7 |
| 9 | 5.9 |
| 10 | 6.0 |
* Values from Daya S, Woods S, Ward S, et al: Early pregnancy assessment of transvaginal ultrasound scanning. Can Med Assoc J 144(4):441-446, 1991.
From the time the embryo is visible until the end of the first trimester, dating is based on the length of the embryo or fetus, measured from the top of the head to the bottom of the rump, the CRL. Gestational age is assigned based on CRL by using published formulas or tables ( Table 6-2 ). Dating by CRL is more accurate in the early first trimester, when accuracy is ±0.5 week, than toward the end of the first trimester, when accuracy approaches ±1.0 week. Care must be taken to measure the CRL correctly, particularly toward the end of the first trimester. The fetus should be in neutral position, neither hyperextended nor hyperflexed with the chin tucked against the chest. The calipers should be placed at the top of the fetal head and the bottom of the rump, making sure not to include the yolk sac or lower extremities in the measurement ( Fig. 6-3 ).
| CRL (mm) | Gestational Age (Weeks) * | CRL (mm) | Gestational Age (Weeks) * |
|---|---|---|---|
| 5 | 6.0 | 45 | 11.1 |
| 6 | 6.2 | 46 | 11.2 |
| 7 | 6.4 | 47 | 11.3 |
| 8 | 6.6 | 48 | 11.4 |
| 9 | 6.8 | 49 | 11.4 |
| 10 | 7.0 | 50 | 11.5 |
| 11 | 7.2 | 51 | 11.6 |
| 12 | 7.4 | 52 | 11.7 |
| 13 | 7.5 | 53 | 11.8 |
| 14 | 7.7 | 54 | 11.8 |
| 15 | 7.8 | 55 | 11.9 |
| 16 | 8.0 | 56 | 12.0 |
| 17 | 8.1 | 57 | 12.1 |
| 18 | 8.3 | 58 | 12.2 |
| 19 | 8.4 | 59 | 12.2 |
| 20 | 8.5 | 60 | 12.3 |
| 21 | 8.7 | 61 | 12.4 |
| 22 | 8.8 | 62 | 12.4 |
| 23 | 8.9 | 63 | 12.5 |
| 24 | 9.0 | 64 | 12.6 |
| 25 | 9.1 | 65 | 12.7 |
| 26 | 9.3 | 66 | 12.7 |
| 27 | 9.4 | 67 | 12.8 |
| 28 | 9.5 | 68 | 12.9 |
| 29 | 9.6 | 69 | 12.9 |
| 30 | 9.7 | 70 | 13.0 |
| 31 | 9.8 | 71 | 13.1 |
| 32 | 9.9 | 72 | 13.2 |
| 33 | 10.0 | 73 | 13.2 |
| 34 | 10.1 | 74 | 13.3 |
| 35 | 10.2 | 75 | 13.4 |
| 36 | 10.3 | 76 | 13.4 |
| 37 | 10.4 | 77 | 13.5 |
| 38 | 10.5 | 78 | 13.5 |
| 39 | 10.6 | 79 | 13.6 |
| 40 | 10.7 | 80 | 13.7 |
| 41 | 10.8 | ||
| 42 | 10.8 | ||
| 43 | 10.9 | ||
| 44 | 11.0 |
* Values derived from Robinson HP, Fleming JEE: A critical evaluation of sonar “crown-rump length” measurements. Br J Obstet Gynecol 82:702-710, 1975.

When dating a pregnancy during the first trimester, sonography is more accurate than LMP. However, it is acceptable to use the LMP to date a pregnancy if the LMP is certain and the difference between gestational age by LMP and gestational age by first trimester sonography is less than 7 days.
Second and Third Trimester Dating
Measurements
During the second and third trimesters of pregnancy, measurements of specified fetal parts can be used individually or in combination to estimate gestational age of the pregnancy. The most commonly used measurements for gestational age assignment are the biparietal diameter (BPD), occipitofrontal diameter (OFD), head circumference (HC), abdominal diameter (AD), abdominal circumference (AC), and femur length (FL).
The BPD, OFD, and HC are measured on an axial image of the fetal head at the level of the paired thalami, third ventricle, and cavum septum pellucidum ( Figs. 6-4 and 6-5 ). With a true axial view, the calvarium and intracranial contents appear symmetric on either side of the falx and paired thalami. The BPD is measured by placing the caliper closer to the transducer (i.e., at the top of the image) at the outer edge of the bony calvarium, while the caliper farther from the transducer should be placed on the inner edge of the bony calvarium. That is, the BPD is measured from leading edge to leading edge of the calvarium. Improper measurements, either from using an image at an incorrect plane of section through the fetal head or from misplacement of the sonographic calipers, will lead to errors in estimating gestational age and fetal weight.


The OFD and HC can be measured on the same view of the fetal head as the BPD, provided the image is a true axial view that includes the entire head from the frontal bone to the occipital bone. For the OFD measurement, one caliper is placed in the anterior midline in the middle of the echogenic line of the frontal bone, and the second is placed posteriorly in the middle of the echogenic line of the occipital bone. The HC is measured by using elliptical calipers to outline the outer edge of the skull (see Figs. 6-4 and 6-5A ). The HC can also be calculated from the BPD and OFD:
This formula is based on the circumference of an ellipse with diameters BPD and OFD with a correction factor because these diameters are not outer-to-outer.
The OFD is also used in conjunction with the BPD to take into account the shape of the fetal head. A standard-shaped fetal head has an OFD : BPD ratio of 1.265. When the OFD : BPD ratio is higher or lower than 1.265, a corrected BPD can be calculated with the formula:
The corrected BPD represents the BPD of a standard-shaped fetal head with the same cross-sectional area.
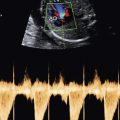
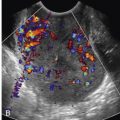
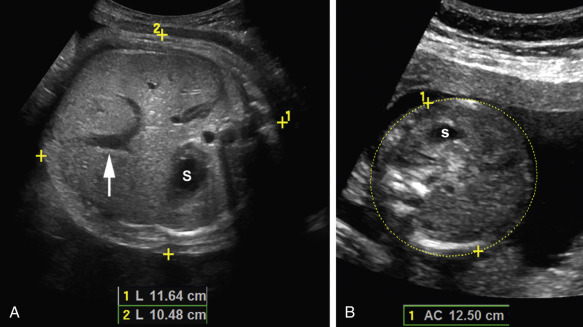
The AD and AC are measured on an axial image of the fetal abdomen at the level of the stomach and intrahepatic portion of the umbilical vein. The abdomen should be as round as possible, and the outer skin surface should be visible all the way around. For the AD, two perpendicular measurements are taken with the calipers placed on the outer surface of the skin. The anteroposterior AD is measured from the anterior midline to the posterior midline, the latter behind the spine. The transverse AD is measured perpendicular to the anteroposterior AD, with calipers placed on the skin surface on both sides of the fetal abdomen ( Fig. 6-6 ). The AC is measured via elliptical calipers outlining the outer surface of the skin around the abdomen ( Figs. 6-6 and 6-7 ). The AC can also be calculated from the two orthogonal AD measurements as:
When measuring the fetal abdomen, care must be taken to make sure the image is at the correct level, the entire abdomen is included on the image, the outer skin surface is visible, and the calipers are placed appropriately. Images showing part of a kidney are too low in the abdomen and will yield inaccurate estimations of fetal age and weight. Misplacement of the calipers inside the fetal skin layer or the abdomen will lead to underestimation of the gestational age and weight.

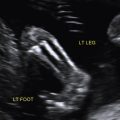
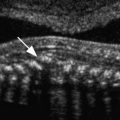
The measurement of the fetal femur is actually a measurement of the femoral diaphysis, because, for most of pregnancy, only the diaphysis of the bone is ossified. For most accurate femur measurements, an attempt should be made to image the femur as perpendicular to the ultrasound beam as possible. On the image, the femur is measured by placing the calipers at either end of the ossified diaphysis ( Figs. 6-8 and 6-9 ). It is important not to include any of the femoral epiphysis, which can appear as a linear projection from the proximal or distal end of the diaphysis.


Assigning Gestational Age in the Second and Third Trimesters
In the second and third trimesters, gestational age can be assigned based on a single measurement, such as the BPD, corrected BPD, HC, or FL ( Tables 6-3 through 6-5 ), or on a combination of measurements, such as with composite age formulas. Head measurements that take into account the shape of the fetal head—namely, the corrected BPD and the HC—are more accurate than the BPD alone or FL alone in the second trimester. Accuracy of the corrected BPD and the HC before 20 weeks is approximately ±1.2 weeks. As pregnancy progresses, the accuracy of all measurements decreases, such that, by the end of the third trimester, the accuracy of gestational age estimation by head measurements is about ±3.5 weeks ( Table 6-6 ). Although head measurements are more accurate than FL in the second trimester, by the third trimester, the accuracy of the FL is similar to that of head measurements. The AC is a poor predictor of gestational age, particularly later in pregnancy, and should not be used on its own to assign gestational age.
| BPD or BPDc (mm) | Gestational Age (Weeks) | BPD or BPDc (mm) | Gestational Age (Weeks) |
|---|---|---|---|
| 20 | 13.2 | 60 | 24.2 |
| 21 | 13.4 | 61 | 24.5 |
| 22 | 13.6 | 62 | 24.9 |
| 23 | 13.8 | 63 | 25.3 |
| 24 | 14.0 | 64 | 25.7 |
| 25 | 14.3 | 65 | 26.1 |
| 26 | 14.5 | 66 | 26.5 |
| 27 | 14.7 | 67 | 26.9 |
| 28 | 14.9 | 68 | 27.3 |
| 29 | 15.1 | 69 | 27.7 |
| 30 | 15.4 | 70 | 28.1 |
| 31 | 15.6 | 71 | 28.5 |
| 32 | 15.8 | 72 | 29.0 |
| 33 | 16.1 | 73 | 29.4 |
| 34 | 16.3 | 74 | 29.9 |
| 35 | 16.6 | 75 | 30.3 |
| 36 | 16.8 | 76 | 30.8 |
| 37 | 17.1 | 77 | 31.2 |
| 38 | 17.3 | 78 | 31.7 |
| 39 | 17.6 | 79 | 32.2 |
| 40 | 17.9 | 80 | 32.7 |
| 41 | 18.1 | 81 | 33.2 |
| 42 | 18.4 | 82 | 33.7 |
| 43 | 18.7 | 83 | 34.2 |
| 44 | 19.0 | 84 | 34.7 |
| 45 | 19.3 | 85 | 35.2 |
| 46 | 19.6 | 86 | 35.8 |
| 47 | 19.9 | 87 | 36.3 |
| 48 | 20.2 | 88 | 36.9 |
| 49 | 20.5 | 89 | 37.4 |
| 50 | 20.8 | 90 | 38.0 |
| 51 | 21.1 | 91 | 38.6 |
| 52 | 21.4 | 92 | 39.2 |
| 53 | 21.7 | 93 | 39.8 |
| 54 | 22.1 | 94 | 40.4 |
| 55 | 22.4 | 95 | 41.0 |
| 56 | 22.8 | 96 | 41.6 |
| 57 | 23.1 | > 97 | 42.0 |
| 58 | 23.5 | ||
| 59 | 23.8 |
| HC (mm) | Gestational Age (Weeks) | HC (mm) | Gestational Age (Weeks) |
|---|---|---|---|
| 80 | 13.4 | 225 | 24.5 |
| 85 | 13.7 | 230 | 25.0 |
| 90 | 14.0 | 235 | 25.5 |
| 95 | 14.3 | 240 | 26.1 |
| 100 | 14.7 | 245 | 26.6 |
| 105 | 15.0 | 250 | 27.1 |
| 110 | 15.3 | 255 | 27.7 |
| 115 | 15.6 | 260 | 28.3 |
| 120 | 16.0 | 265 | 28.9 |
| 125 | 16.3 | 270 | 29.4 |
| 130 | 16.6 | 275 | 30.0 |
| 135 | 17.0 | 280 | 30.7 |
| 140 | 17.3 | 285 | 31.3 |
| 145 | 17.7 | 290 | 31.9 |
| 150 | 18.1 | 295 | 32.6 |
| 155 | 18.4 | 300 | 33.3 |
| 160 | 18.8 | 305 | 33.9 |
| 165 | 19.2 | 310 | 34.6 |
| 170 | 19.6 | 315 | 35.3 |
| 175 | 20.0 | 320 | 36.1 |
| 180 | 20.4 | 325 | 36.8 |
| 185 | 20.8 | 330 | 37.6 |
| 190 | 21.3 | 335 | 38.3 |
| 195 | 21.7 | 340 | 39.1 |
| 200 | 22.2 | 345 | 39.9 |
| 205 | 22.6 | 350 | 40.7 |
| 210 | 23.1 | 355 | 41.6 |
| 215 | 23.6 | 360 | 42.4 |
| 220 | 24.0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree