Fig. 1
Transvaginal ultrasound scan (TVUS) showing a transverse view through the uterus (U). There is a large, well marginated subserosal fibroid (F) posteriorly which is heterogeneous and hyperechoic to surrounding myometrium
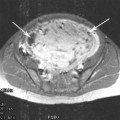
At MRI, fibroids are well defined and of markedly low T1 and T2 signal intensity. Given its improved soft tissue resolution, fibroids are best defined using T2 weighted sequences (Fig. 2). Areas of cystic degeneration are seen as fluid signal intensity, low on T1 and high on T2 weighted sequences. Areas of high T1 signal intensity due to the T1 shortening effect of methaemoglobin indicate haemorrhagic degeneration (Fig. 3).
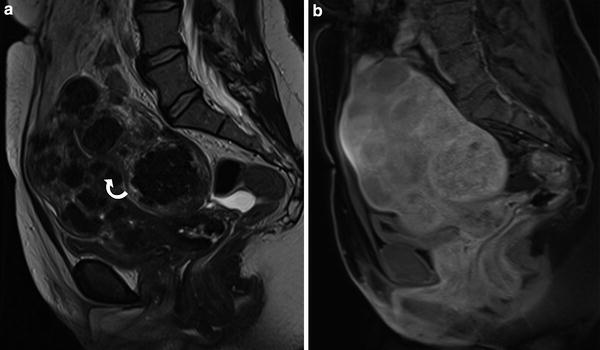
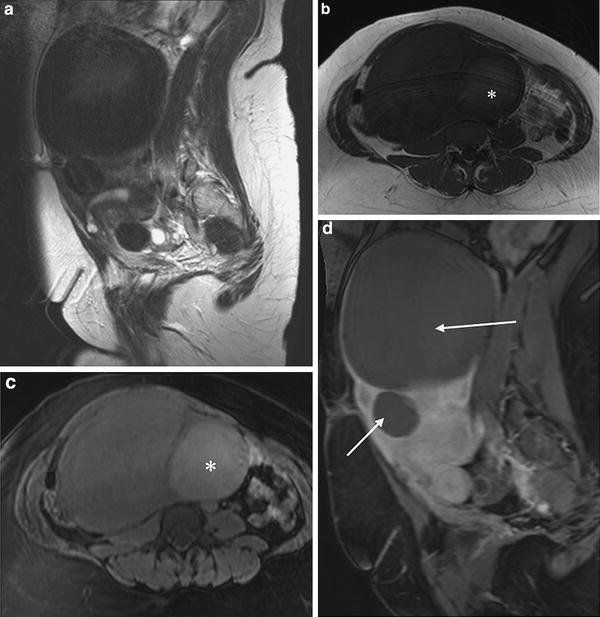
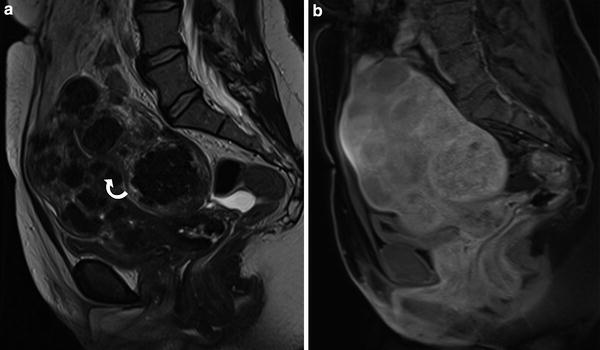
Fig. 2
MRI a T2 sagittal and b T1 fat saturated (T1FS) following contrast medium administration showing enlarged uterus with multiple fibroids. Note the submucosal fibroids indenting the endometrium (curved arrow). Although small these are often the cause of menorrhagia. Following contrast medium administration all of the fibroids enhance avidly, similar to the surrounding myometrium
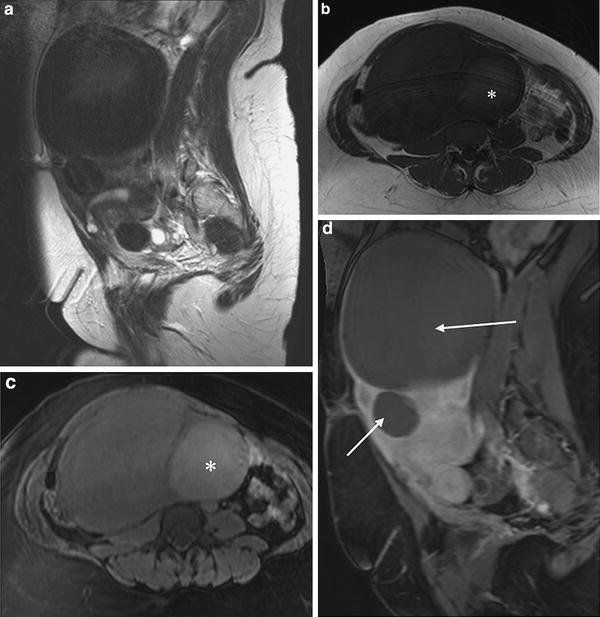
Fig. 3
MRI in a patient referred for assessment for UAE. a T2 sagittal, b T1 axial, c T1 axial with fat saturation (T1FS) before and d after contrast medium administration. Images show well marginated intramural and subserosal fibroids which are low signal intensity on T2 and T1 images. There is T1 hyperintensity in at least one of the fibroids in keeping with haemorrhagic degeneration (*). Following contrast medium administration the dominant fibroids do not enhance at all (arrows) and this patient was therefore unsuitable for treatment with UAE
Fibroid vascularity can be accurately assessed using contrast enhanced MRI. This involves the use of fast dynamic scanning before and at least 3 time points after the intravenous administration of Gadolinium. Three-dimensional volumetric sequences with fat suppression are used and obtained in either a coronal or sagittal plane Fibroids typically enhance avidly, usually iso or hyperintense to surrounding myometrium (Fig. 2). Degeneration within fibroids is visualised as complete or heterogeneous areas of non-enhancement (Figs. 3, 4). Patients with a significant volume of non-vascular fibroids are clearly unsuitable for UAE.
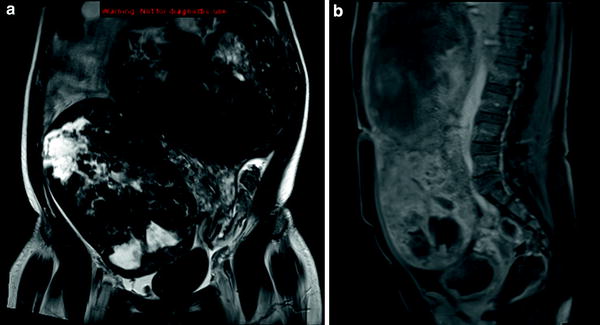
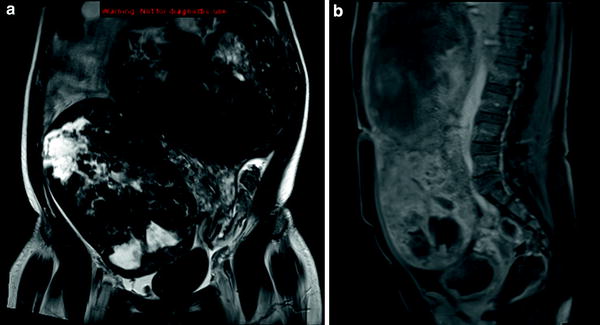
Fig. 4
MRI a T2 coronal and b sagittal T1FS after contrast administration in a patient with large, broad-based pedunculated fibroids. There are prominent areas cystic degeneration which are of high T2 signal intensity and contrast enhancement is patchy
2.2 Fibroid Mapping
In order to measure post-embolisation response, it is important to accurately assess the volume and location of dominant fibroids prior to treatment. Volume measurements of the dominant fibroids can be readily made with both US and MRI. However, for the purpose of post-embolisation assessment, MRI provides more standardised and easily comparable images for follow up. Fibroid location as well as volume should be correlated with patient’s symptoms. For example, submucosal fibroids, even when small, are typically responsible for abnormal uterine bleeding (Buttram and Reiter 1981; Spies et al. 2002a), whereas large intramural or subserosal fibroids are typically responsible for pressure symptoms (Fig. 4).
Pedunculated subserosal fibroids, defined as those having a stalk diameter 50 % narrower than the fibroid diameter (Goodwin et al. 2001) have long been recognised as a relative contraindication to UAE (Fig. 5). Primarily there is potential risk of the stalk undergoing infarction causing either fibroid torsion or detachment and potential peritonitis. This risk however is rare. More commonly however, pedunculated fibroids, which may have a dual blood supply parasitised from adjacent organs, have been shown to respond less well to UAE and be a cause of treatment failure (Katsumori et al. 2005; Toor et al. 2008). It is important therefore for radiologists to identify pedunculated subserosal fibroids in the context of the other fibroids present and patient’s symptoms. If there are widespread fibroids in all locations, the patient may still benefit from UAE. Conversely, a patient with mainly pressure symptoms and a dominant pedunculated subserosal fibroid might be best treated with myomectomy. Pedunculated subserosal fibroids, particularly in a large uterus can be significantly under reported with US. If transvaginal US alone is performed, subserosal fibroids located outside of the pelvis will not be visualised. MRI however, provides a large imaging field of view in multiple planes and thus, pedunculated subserosal fibroids and their stalks can be accurately identified (Fig. 5).
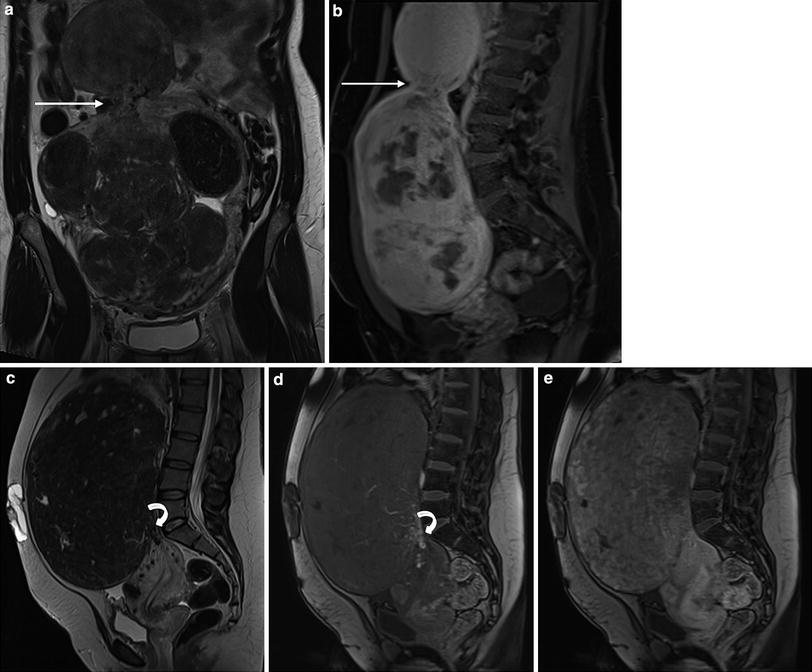
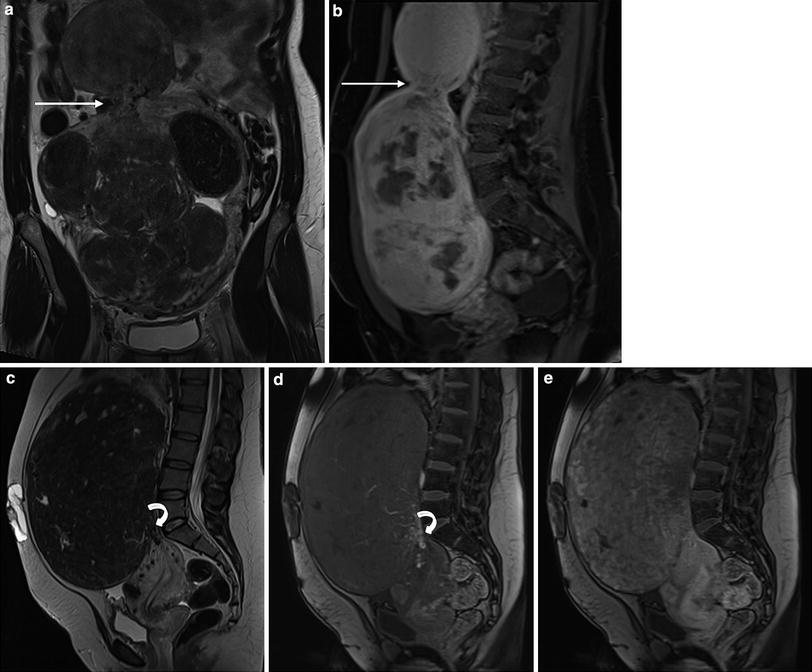
Fig. 5
a Coronal T2 and b Sagittal T1FS contrast-enhanced MRI in a patient with multiple fibroids. There is a dominant pedunculated fibroid on a narrow stalk (arrow) arising from the uterine fundus which is markedly vascular. Despite this, the patient was referred for UAE given the presence of multiple other fibroids and a combination of bleeding and pressure symptoms. c T2 sagittal MRI in a different patient with a large, almost solitary pedunculated fibroid. There is a very narrow (1 cm) vascular pedicle (curved arrow) which is well demonstrated on the early arterial post-contrast MRI (d) and the fibroid enhances avidly (e). Myomectomy might be considered a more favourable treatment option for this patient given the lack of other fibroids and predominance of pressure symptoms
Fibroid location may also provide prognostic information regarding potential complications or side effects of embolisation. Submucosal fibroids or intramural fibroids with a submucosal component are at risk of becoming endocavitary and sloughing off, reported in up to 3 % of dominant submucosal fibroids in one study (Verma et al. 2008). In particular, fibroids which have a higher ratio between their endometrial interface and longest dimension are more at risk of becoming endocavitary (Fig. 6). Fibroid passage, although a consequence rather than true complication of the procedure, can be accompanied by pain and infection which may require hospital admission for treatment. It can therefore be useful to identify these potential higher risk patients prior to embolisation.
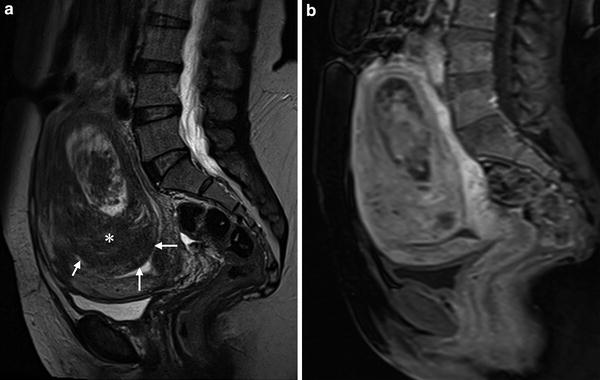
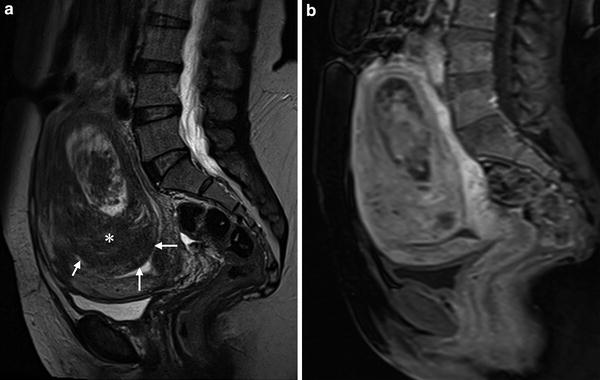
Fig. 6
Intracavitary fibroid. a Sagittal T2 and b Sagittal T1FS with contrast enhancement MRI showing a dominant submucosal fibroid (*) with a large intracavitary component. Compressed endometrium is seen indented by the fibroid (short arrows). Although there is some central degeneration, the remainder of the fibroid enhances avidly and would be suitable for UAE, although risk of sloughing off is high and the patient should be informed of this possible outcome
2.3 Making the Diagnosis
Fibroids are a common cause of menorrhagia but may also present with dysmenorrhoea, irregular uterine bleeding or pelvic pain. Given that fibroids are common and their symptoms non-specific it is important to consider alternative or concurrent pathologies prior to embarking on treatment.
2.3.1 Adenomyosis
Adenomyosis is defined as the presence of heterotopic endometrial glandular and stromal tissue within the myometrium with surrounding smooth muscle hypertrophy and hyperplasia. It can result in uterine enlargement and abnormal uterine bleeding and be clinically, demographically and sonographically indistinguishable from fibroid disease, with which it may co-exist. Differentiation between the two conditions however can be achieved with almost 100 % accuracy with MRI (Togashi et al. 1989; Ascher et al. 1994). With T2 weighted MRI, adenomyosis is visualised as either focal or diffuse widening of the innermost layer of myometrium (the junctional zone). This low signal intensity interface between the endometrium and deep myometrium is normally symmetrical in appearance and less than 8 mm in thickness (Fig. 7). Greater than 12 mm is highly suggestive of adenomyosis. In many cases quite marked areas of ill-defined low signal intensity within the myometrium can be seen. In contrast to fibroids, the areas are less well demarcated and are in contact with the endometrial interface. Foci of T2 high signal intensity in keeping with dilated endometrial glandular tissue is frequently present. Less commonly, T1 hyperintense foci corresponding to areas of haemorrhage may also be seen.
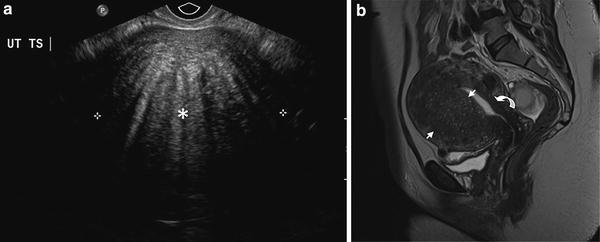
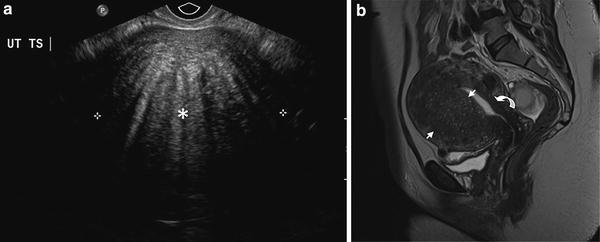
Fig. 7
Adenomyosis a TVUS showing what appears to be a heterogeneous circumscribed mass. There are multiple area of linear posterior shadowing, a typical feature of adenomyosis. b Sagittal T2 weighted MRI confirms myometrial enlargement anteriorly, containing areas of T2 hyperintensity (between arrow heads), characteristic of adenomyosis. There is marked widening of the junctional zone anteriorly which is within normal limits posteriorly (curved arrow)
Adenomyosis was previously thought of as a cause of failed UAE for fibroids. However, following UAE, reduction in junctional zone thickness and corresponding improvement in patients’ symptoms occurs, at least in the short term. More recent evidence suggests that UAE can also be an effective long-term treatment for adenomyosis in a proportion of patients (Kim et al. 2007). Therefore now in most institutions, where fibroids and adenomyosis co-exist, UAE is still considered.
2.3.2 Endometriosis
Endometriosis, defined as the presence of ectopic endometrial tissue outside of the uterus, commonly manifests as symptoms of pelvic pain, dysmenorrhoea and bloating similar to that of symptomatic fibroid disease. Repeated bleeding into endometriotic implants can lead to the formation of endometriomas within the ovary. These gelatinous and haemorrhage filled cysts are well visualised with TVUS (Fig. 8). However, tiny peritoneal implants throughout the pelvis will not be visualised with TVUS and require either MRI or laparoscopic examination for diagnosis. T1 weighted sequences with fat saturation have high sensitivity for the demonstration of tiny haemorrhagic foci which are seen as markedly hyperintense to surrounding tissue (Fig. 8). Using this technique, even tiny foci of superficial endometriosis can be demonstrated non-invasively. Repeated bleeding leading to chronic inflammation in these areas can lead to pelvic fibrosis and adhesions between the pelvic organs, bladder and sigmoid colon. The resulting symptoms can be severe and surgical intervention can be difficult. As fibroids may co-exist in these patients it is important to identify the primary cause of the symptoms as management of the two conditions is greatly different. The multiplanar imaging ability of MRI readily enables demonstration of areas of fibrosis and adhesions.
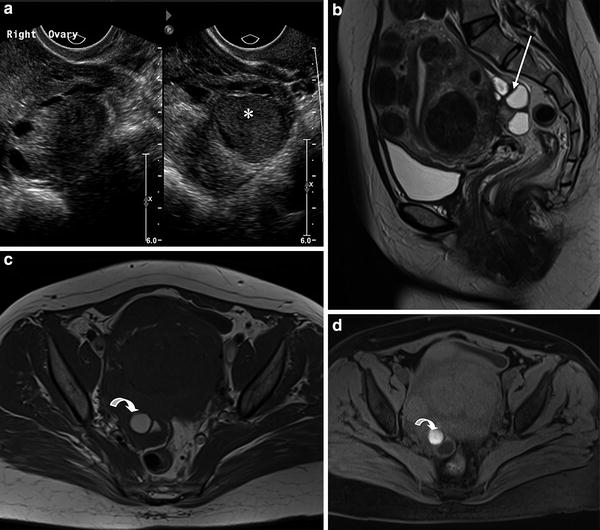
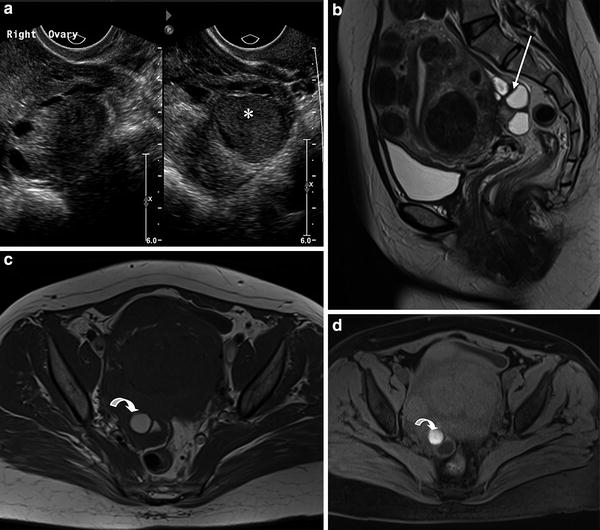
Fig. 8
Endometriosis. a TVUS showing a slightly hypoechoic rounded lesion (*) within the right ovary which contains homogeneous low level internal echoes throughout. There is posterior acoustic enhancement, confirming the lesion is cystic rather than solid. b Sagittal T2 weighted c axial T1 weighted and d axial T1FS MRI in a second patient. In addition to the multiple uterine fibroids, there is a multiloculated cystic adnexal mass posterior to the uterus (arrow). It contains high signal intensity material on both the T1 and T1FS sequences, confirming the presence of blood products in this endometrioma
Other causes of irregular menstrual bleeding and menorrhagia include polycystic ovarian syndrome, endometrial polyps and hyperplasia and TVUS can aid the non-invasive diagnosis of these conditions.
2.3.3 Uterine Sarcoma
Uterine sarcomas are rare, accounting for less than 3 % of all uterine malignancy. Carcinosarcoma is the commonest histological subtype, followed by leiomyosarcoma, and rarely, endometrial stromal sarcoma and adenosarcoma. Leiomyosarcomas can arise de novo or from malignant degeneration, however, this is rare, occurring in less than 1 % of benign fibroids. Malignant degeneration, in the early stages can be multifocal, with benign and malignant elements combined. Differentiation from a benign fibroid with imaging may not be possible. Similarly, due to sampling error, histological evaluation following biopsy is also unreliable. MRI features including loss of the normal low T2 signal intensity, areas of high T2 cystic change and avid contrast medium enhancement have been described (Tanaka et al. 2004) (Fig. 9




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree