A blind date: Things are going well, but really, this person could be a serial killer for all you know. How do you get to know him? Sometimes it’s easy, but more often it takes time and attention to look for telling signs about his personality and values. Reading mammograms for women with dense breast tissue is likewise a process. Relax. Take your time. Dig in and find that little cancer that will save her life.
Women with dense breast tissue have two strikes against them. They are more likely to be diagnosed with breast cancer, and we are less likely to detect it. Dense tissue is a moderate independent risk factor for breast cancer and is associated with a four- to sixfold increase in breast cancer risk compared with that of women with fatty replaced breasts. The sensitivity of mammography for women with dense tissue is reduced to about 60%. Cancers are most likely to develop within the dense fibroglandular tissue rather than in the surrounding fat, where they might be easier to detect. Our level of concern as radiologists must be heightened for these women because they are at higher risk and have more difficult mammograms to interpret.
Factors Associated with Dense Tissue
In this chapter, “dense” tissue refers to heterogeneously dense and extremely dense fibroglandular tissue composition, as defined in the ACR BI-RADS Atlas. Mammographically dense tissue typically occurs in slightly less than half of screened populations. Younger age is strongly associated with increased mammographic density. In one study, 55% of women under 50 had dense tissue, compared with about 30% of women who were age 50 and older ( Box 12-1 ).
- •
Younger age
- •
Lower body mass index
- •
Later menarche
- •
Later age of first birth
- •
Lower parity
- •
Genetic tendency
- •
Use of hormone replacement therapy
Limitations of Mammography
All of the mammographic signs of malignancy tend to be more difficult to detect in dense tissue, and the reduced sensitivity of mammography in these women has been well established. In a series of over 460,000 women, the sensitivity of screening mammography was 62% when the tissue was extremely dense and 88% when it was almost entirely fatty. Other studies have even worse results, with sensitivity ranging from 29% to 50% for women with dense breast tissue.
Interpreting these dense mammograms is difficult but not impossible. We need to work really hard for these women to find their cancers! Keep in mind that many nonpalpable cancers remain detectable even when the tissue is extremely dense. For example, cancers that develop within the retromammary fat, are located at the border of the fibroglandular tissue, or are associated with calcifications are often readily perceived.
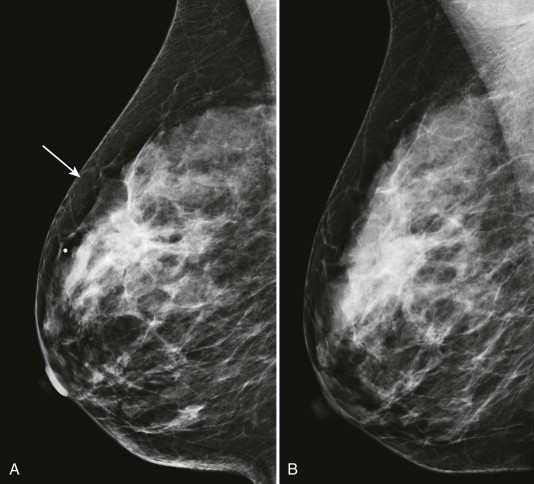
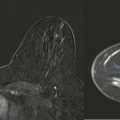
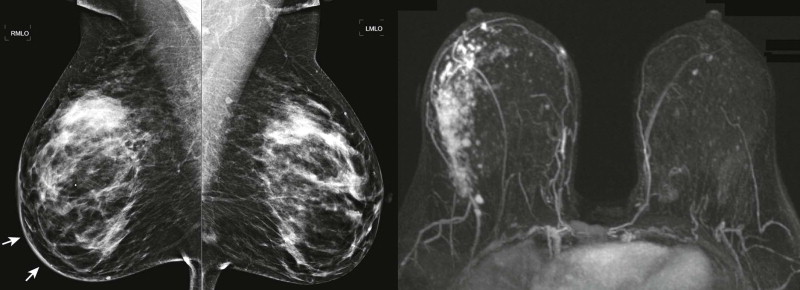
Detection of malignant lesions by ultrasonography (US) and magnetic resonance imaging (MRI) is less limited by dense tissue, and their use, according to established indications, will also provide your patients with dense tissue the chance for earlier cancer detection ( Fig. 12-1 ).
Evaluating Findings in Dense Tissue
Technical Considerations
You can’t get to know someone if you never meet the person. When the tissue is dense, it is particularly important to insist on a study of at least good technical quality, with proper exposure, compression, and absence of significant motion. The signs of cancer are often subtle even with the highest quality imaging; they may become undetectable on a technically limited study. Of course, poor positioning also reduces our ability to find cancer. As the saying goes, “If it’s not on the image, you can’t make the diagnosis.” Don’t let your ability to interpret a study be compromised by positioning or other technical factors. Recall the patient to have the limited views repeated.
Digital mammography has been shown to be superior to film-screen mammography in diagnostic accuracy in a screened population of women with heterogeneously dense or extremely dense tissue. Therefore, for facilities with both digital and film-screen mammography equipment, triaging women with dense tissue for imaging using the digital equipment may be beneficial.
Tomosynthesis is a digital mammographic technique that acquires multiple images from different angles that are processed for three-dimensional review. The first commercial unit received Food and Drug Administration (FDA) approval in 2011. This technique overcomes many of the limitations caused by tissue overlap. Although the most appropriate clinical use of this technology remains to be defined, it shows particular promise in improving the detection and characterization of soft tissue density lesions within dense tissue.
Screening US detected 3 additional cancers per 1000 high-risk women also screened with mammography in the ACRIN 6666 trial. Because of low specificity, the use of screening US remains controversial for women with the indication of dense breasts without other risk factors. The positive predictive value for cancer when biopsy was recommended was only 7% in the ACRIN 6666 trial and may be lower for women of moderate risk. We will focus on mammography in this chapter. For more information on nonmammographic screening, please see Chapter 13 , Measuring and Managing Breast Cancer Risk.
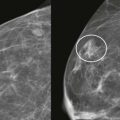
Callback Threshold
In dense tissue, masses are often obscured and calcifications may be less conspicuous. The findings that are visualized may represent the “tip of the iceberg”—part of a more extensive lesion that is mostly obscured. It therefore makes sense to lower your threshold for recalling screening patients for diagnostic evaluation, to more fully evaluate subtle findings that are not well characterized on the screening views alone.
Getting to Know You
Let’s think about that first date again. What are your techniques for getting to know someone? What is your first impression? Are there any apparent red flags? If not, then you are probably going to do the easy stuff, like finding out about common interests. What is his job? What are his hobbies? Things are going well. We’ve made it to the second date. Now you are going to dig deeper by assessing personality traits. Is he going to make you crazy by leaving off the toothpaste top? Or is he going to make you arrange 18 pillows on the couch correctly? Assuming that he makes it past that point, now you really need to know if he is a “keeper.” You need to go very deep by understanding his values. Is family important? Is he honest and kind? Oh my, did he really just damage that person’s car and keep driving?
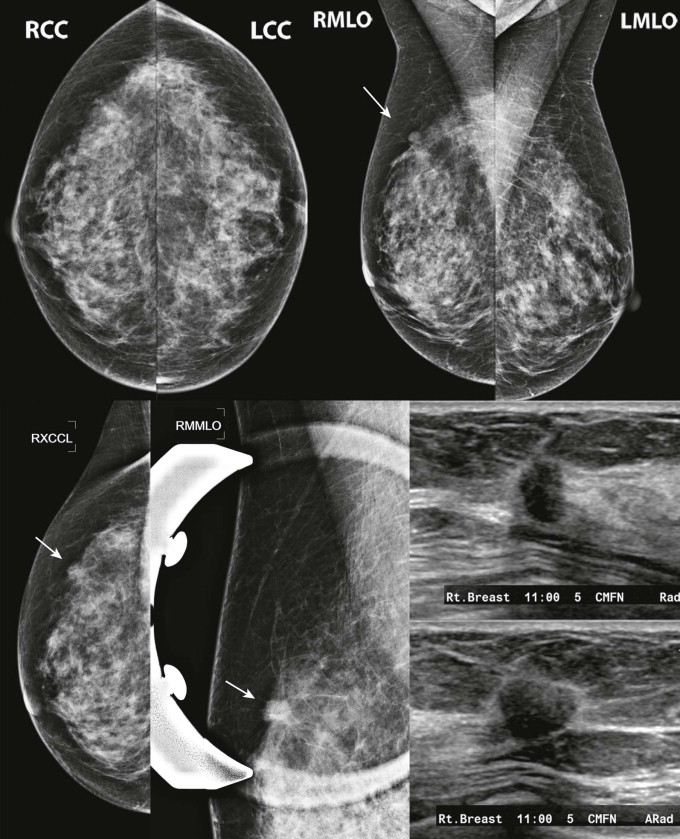
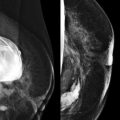
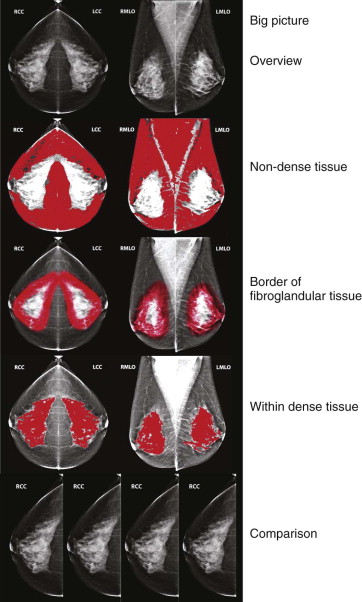
Interpretation of dense mammograms is similar ( Fig. 12-2 ). We’ll start with that first impression. Lean back in your chair and get the big picture. Next, start with the easy stuff—the retroglandular fat (one of the “wrong neighborhoods” discussed in the Chapter 3 , Screening Mammography 101 and Beyond). Then we dig in deeper. Look at the border between the fibroglandular tissue and fat. Then comes the really hard part: focus on the dense tissue, looking for subtle masses, calcifications, distortion, and asymmetries. Finally, compare the study carefully with mammograms that are at least 2 years older.
While interpreting these studies, remember to keep using all of the good habits you have already developed (reviewed in Chapter 3 ); minimize interruptions and use consistent hanging protocols and search patterns. The use of computer-aided detection is also a good strategy for reviewing these difficult mammograms.
First Impressions
Let’s look at each step in a little more detail. We’ll start with the first impression. At our biopsy review conference, we sometimes have a case in which the resident cannot see the lesion to save his soul. His face is inches from the screen as he searches and sweats. Meanwhile, the resident in the back of the room immediately sees the finding and wonders why her colleague is struggling.
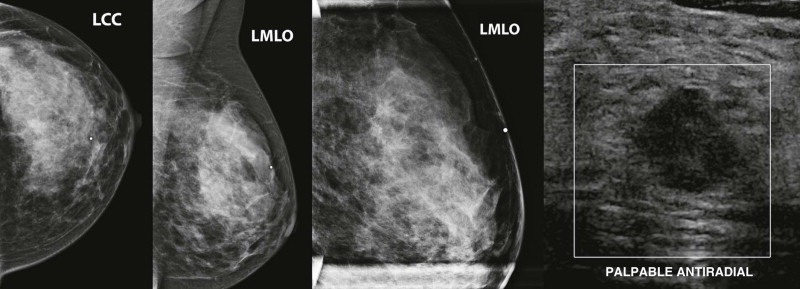
Start the review of every mammogram by looking at the big picture. Findings that may be easier to see when leaning back in your chair include abnormalities of the skin and nipples ( Figs. 12-3 and 12-4 ), differences in breast size and compressibility, and large asymmetries. Asymmetry of breast size on mammography—reflecting reduced compressibility of the tissue—is a sign of invasive lobular carcinoma (ILC) that may be detected on the overview interpretation of the images (see Fig. 12-4 ).
The Easy Part (What Do You Like to Do in Your Spare Time?)
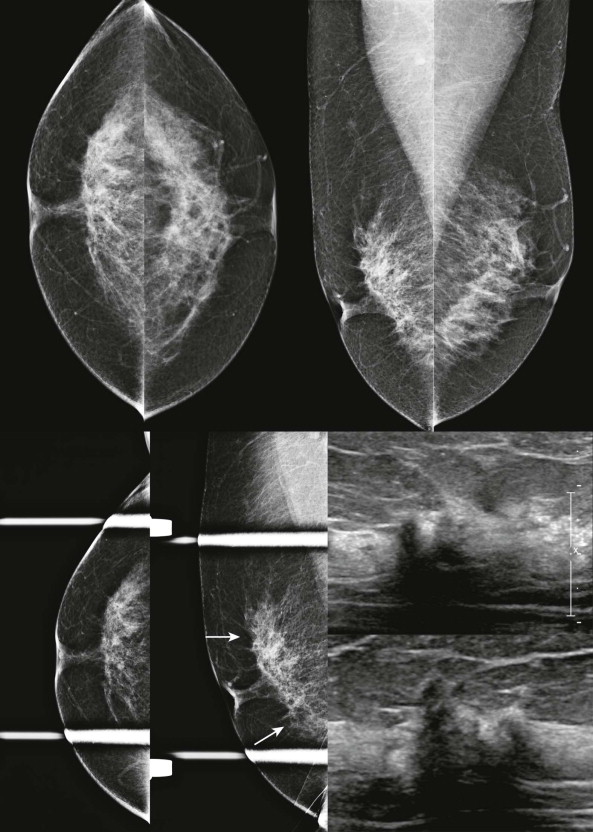
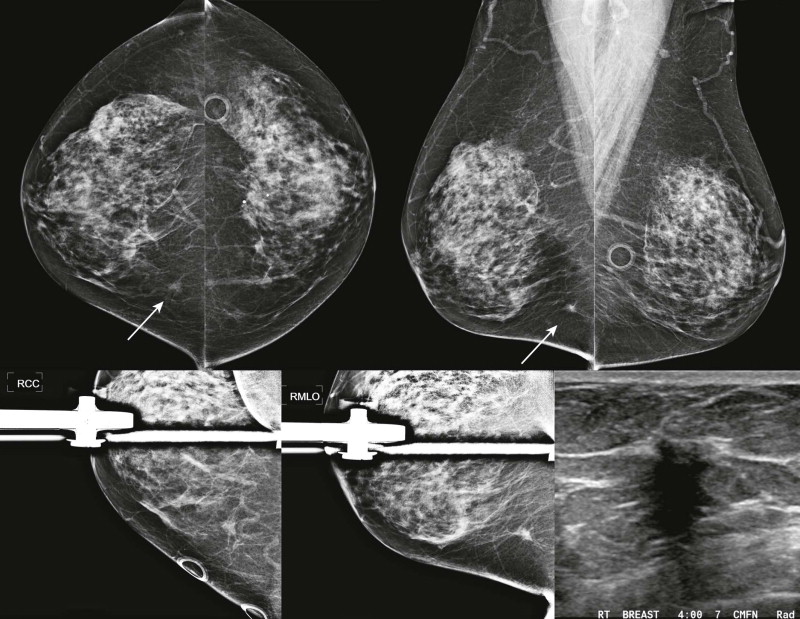
The easy areas of the dense mammogram are those that are fatty. Even when the fibroglandular tissue is extremely dense, there are usually regions that contain enough fat to allow detection of small lesions ( Fig. 12-5 ). These areas include the subcutaneous and retroglandular tissues, the axillary tail, and the axilla. Asymmetries in the posterior breast that are outside the fibroglandular tissue deserve careful scrutiny, since they are frequently found to be malignant. Axillary masses or adenopathy are often well visualized in women with dense fibroglandular tissue.
Going a Little Deeper (What Kind of Personality and Values Does He Have?)
Now we are going to dig in a little. Let’s work our way into the tissue by looking at the fibroglandular border—the interface of the dense tissue with the subcutaneous and retroglandular fat. The fat adjacent to this border provides contrast that can make malignancies that develop in this region more conspicuous. The contour of this border should be closely examined and compared with the contralateral breast and with previous mammograms as part of the standard routine.
Although the mammographic appearance of the fibroglandular border varies greatly among patients and is affected by positioning, abrupt changes in this contour can be a sign of malignancy. Look at this border as though it were a road ( Box 12-2 ). Are there potholes? Retraction of the fibroglandular border can be caused by desmosplastic reaction that is commonly associated with invasive malignancies ( Fig. 12-6 ). Are there speed bumps? Soft tissue density protrusions into the fat that alter the contour of the fibroglandular border can also signify the presence of a partially obscured mass ( Fig. 12-7 ). A fallen tree in the way? Even if a cancer is mostly obscured by dense tissue, spicules may be visible extending from the fibroglandular border into the adjacent fat ( Figs. 12-8 and 12-9 ).
- •
Retraction (pot hole)
- •
Protrusion (speed bump)
- •
Straightening or spicules (road hazard)