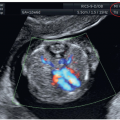
and PAPP-A at 11+0 to 13+6 weeks of gestation in 108,982 singleton pregnancies, T21, 18, and 13 were detected in 90%, 97%, and 92% respectively with a false-positive rate of 4%.6 Monosomy X was also detected in more than 90% of cases along with more than 85% of triploidies and more than 30% of other chromosomal abnormalities.6 In addition to NT, other sensitive first trimester ultrasound markers of T21 include absence or hypoplasia of the nasal bone (Fig. 6.1), cardiac malformations (atrioventricular septal defect) with or without generalized edema (Figs. 6.2 and 6.3), tricuspid regurgitation (Fig. 6.4A), aberrant right subclavian artery (Fig. 6.4B), echogenic intracardiac focus (Fig. 6.4C), and increased impedance
to flow in the ductus venosus (Fig. 6.5). First trimester features of fetuses with T21 are listed in Table 6.2. Additional first trimester findings in T21 fetuses are shown in images in various chapters of this book.
Table 6.1 • Biochemical and Sonographic Features of Trisomies 21, 18, and 13 | ||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||
 Figure 6.3: Transverse views of the fetal chest at the level of the four-chamber view in gray scale (A) and color Doppler (B) in a fetus with trisomy 21 at 12 weeks of gestation. Note the presence of an atrioventricular septal defect (asterisk) in A and B, which represents the typical cardiac anomaly of this syndrome. Also note the associated body edema (arrows), which resolved at 16 weeks upon follow-up. See Figure 6.4 for additional sonographic markers of trisomy 21 in the first trimester. LV, left ventricle; RV, right ventricle. |
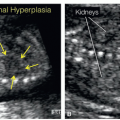
normal fetuses and 37 fetuses with T18, the first trimester ultrasound examination was found to be a good screening test for T18.7 The mean NT thickness was 5.4 mm in T18 fetuses as compared to 1.7 mm in euploid fetuses.7 Congenital heart defects were observed in 70.3% of T18 fetuses and in 0.5% of euploid fetuses and extracardiac malformations were identified in 35.1% of T18 fetuses and in 0.8% of euploid fetuses.7 Only one case of T18 demonstrated no sonographic markers of aneuploidy.7
Table 6.2 • First Trimester Features of Trisomy 21 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
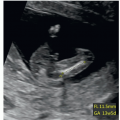
 Figure 6.6: Midsagittal view of the body of a fetus with trisomy 18 at 12 weeks of gestation showing several typical abnormalities. Note the short crown-lump length (1), the thickened nuchal translucency (2), the absence of an ossified nasal bone (3), the dilated fourth ventricle (4), the small omphalocele with bowel content (5), and the maxillary gap as a sign of cleft lip and palate (6). See Figures 6.7, 6.8, 6.9, 6.10 and 6.11 for associated fetal abnormalities with trisomy 18. |
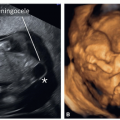
 Figure 6.8: Midsagittal view of the fetal face in three fetuses (A-C) with trisomy 18 at 13, 12, and 14 weeks of gestation, respectively. Note the presence of a normal nuchal translucency (NT) in A, a mildly increased NT in C, and a markedly increased NT in B. All three fetuses have an absent or poorly ossified nasal bone (NB). The posterior fossa is an interesting marker in trisomy 18 and can be normal as in fetus A, but is often dilated as seen in fetus B (open arrow) and occasionally compressed as in fetus C (double headed arrow) in the presence of an open spina bifida. Fetus A was diagnosed with trisomy 18 due to the presence of radius aplasia (see Fig. 6.14) and cardiac abnormalities. Fetus B has a cleft in the maxilla (arrow) suggesting the presence of a facial cleft.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|