Fig. 20.1
Gross pathology of the IRE lesion at 24 h. The right side of the gland is hemorrhagic (pulses = 8, Kv = 1)
We believe the underlying basis for this phenomenon is the preservation of the microvasculature, down to the arteriolar level, throughout IRE lesion. IRE lesions are therefore able to heal throughout their volume whereas cryoablation and RFA lesions, which are completely de-vascularized shortly after lesion creation, must resolve from the edges of the lesion inwards.
In the prostate this has major implications other than just lesion monitoring. Many older patients with prostate cancer have some measure of BPH causing significant urinary flow symptoms. The immediate and midterm effect of cryoablation, therefore, can often be to initially increase the patient’s urinary flow problems. With an IRE lesion and its rapid decrease in the volume of the prostate, in a matter of weeks we might expect actually an improvement in symptoms over the short and long term. This also raises the possibility that IRE might be an excellent treatment for BPH where cryoablation has not been used with success due to the unfavorable characteristics of its lesion resolution.
20.3.2 Uniform Necrosis Within the IRE Lesion
IRE produces a lesion within the prostate with uniform necrosis throughout and to the very margin of the lesion (Fig. 20.2). Since the pulse occurs in microseconds the variability of blood flow has no effect on the destruction within the lesion. The field effect is uniform within the lesion, and therefore the necrosis is uniform, making a distinct margin where the magnitude of the field falls below the irreversible electroporation range. This is in marked contrast to cryoablation lesions, which have a zone of variable destruction as the lesion margin is approached. In the prostate, where so many important structures are packed closely together, this creates a situation in which greater freezing may have to be carried out in order to insure tumor destruction. However, this sets up a potential dilemma: either stop the freeze prematurely to avoid injury to the rectum (possible undertreatment) or risk complications such as impotence when the NVB is included in the cryoablation lesion in order to assure destruction of a nearby cancer (possible overtreatment).
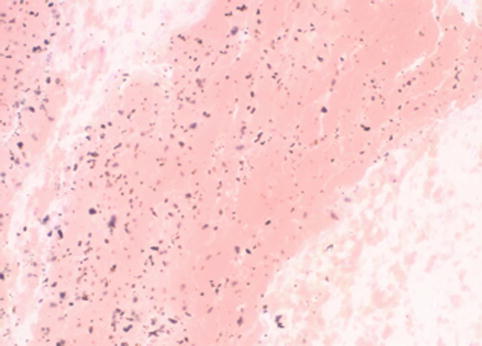
Fig. 20.2
Photomicrograph of prostate tissue that has been electroporated at 24 h. No glandular elements are visible (pulses = 8, Kv = 1)
20.3.3 Lack of Heat Sink Effect
All thermal ablation methods have a significant limitation due to the vessel heat sink effect. This vessel heat sink effects protects cancer adjacent to major vessels resulting in high local recurrence rates in this clinical setting. In contrast, IRE lesions show complete destruction of tissue extended directly up to the vessel wall, without sparing of tissue adjacent to the vessel. In addition, this is accomplished without vessel destruction or occlusion. This characteristic has major implications, particularly in the prostate, where preservation of blood flow is a critical component of maintaining potency. Based on this characteristic, tumor infiltrating the NVB area should be treatable without damage to the associated vessels (Fig. 20.3).
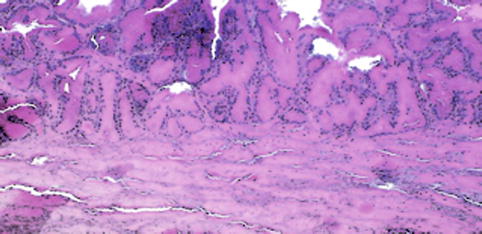
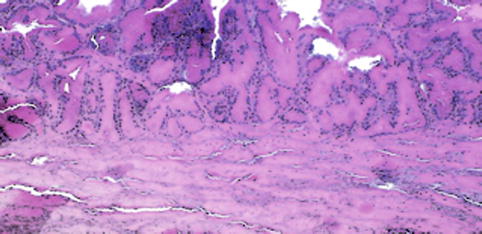
Fig. 20.3
Photomicrograph at the margin of the IRE lesion. A very narrow zone of transition between normal and necrotic tissue is noted at the margin (pulses = 8, Kv = 1)
20.3.4 Preservation of Collagenous and Neural Structures
Another major limitation of thermal ablation technologies has been the nonselective nature of the destructive process. RFA and to a somewhat lesser extent cryoablation cause complications to normal structures that are encompassed within the ablation zone. Gross and microscopic pathology of IRE lesions, however, show preservation of the prostatic urethra (Fig. 20.4) as well as the periprostatic nerves (Fig. 20.5




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree