How to Image the Foot and Ankle
See the protocols for foot and ankle MRI at the end of this chapter.
The foot and ankle are among the most difficult anatomic sites to image, simply because of the angle formed between the foot and ankle. Even the terminology for plane orientation in the foot and ankle is confusing and certainly not universal.
- •
Coils and patient position: Ideally, imaging of the ankle and foot should be done with the foot at right angles to the lower leg with the patient in a supine position. This positioning may require a support on the sole of the foot to maintain the alignment (special surface coils are now being made to accomplish this). A standard extremity coil generally is employed for the foot and ankle (the same one used for knee MRI), and such a precise position for the foot is not always possible to obtain or maintain. More importantly, the patient should be immobilized with padding and made comfortable to prevent movement that would degrade the images, and the radiologist should know the anatomy well enough so that it is easily interpretable, regardless of slight variations in the angle of the foot with the ankle. How to angle MR images properly with the anatomic planes of the foot and ankle to obtain images that are reproducible and most easily understood is shown in the protocols of how to image the foot and ankle. The lower extremity externally rotates when a patient is in a relaxed supine position, and the planes of imaging must be oriented to the anatomy of the foot, rather than to the magnet. True sagittal images of the foot and ankle are mandatory to show the Achilles tendon accurately. If a slice cuts through the tendon obliquely, it gives the false impression of abnormal thickening of the tendon. Imaging the forefoot or toes often is done with the patient prone to allow the toes to be in a neutral position, more easily immobilized, and better centered in the coil. Some centers routinely image the foot and ankle in the prone position to decrease the magic angle effect. Only the extremity with a suspected abnormality is imaged; the opposite normal side is never done simultaneously for comparison because it is unnecessary, and decreases the detail and resolution of the images owing to the larger field of view required. We try to employ a small field of view to increase resolution, so we divide the foot and ankle into one or the other and never scan both simultaneously. An ankle MRI does not include the toes and a forefoot examination does not include the ankle.
- •
Image orientation ( Box 16-1 ): Planes of imaging in the ankle are standard and identical to elsewhere in the body. The foot is more complicated. For purposes of this chapter, we consider the images that run parallel with the long axis of the foot and appear similar to an anteroposterior foot radiograph as either long-axis axial or long-axis coronal images. Images obtained perpendicular to the long axis of the foot so that the metatarsals are seen as five circles of bone cut transversely are referred to as short-axis axials . Sagittal images are self-explanatory and standard.
BOX 16-1
Foot and Ankle Structures to Evaluate in Different Planes
Sagittal
- •
Achilles tendon
- •
Sinus tarsi
- •
Plantar fascia
- •
Osseous structures (length of metatarsals)
- •
Ankle joint
Axial of Ankle and Long-Axis Axial (Coronal) of Foot
- •
Ankle tendons
- •
Sinus tarsi
- •
Tibiofibular ligaments
- •
Anterior and posterior talofibular ligaments
- •
Spring ligament
- •
Osseous structures (length of metatarsals)
Coronal of Ankle and Short-Axis Axial of Foot
- •
Deltoid ligaments, deep and superficial
- •
Calcaneofibular ligament
- •
Tarsal tunnel
- •
Sinus tarsi
- •
Ankle joint
- •
Osseous structures (metatarsals in cross section)
- •
Plantar fascia in cross section
- •
- •
Pulse sequences and regions of interest: Different pulse sequences are used, based on the clinical indications. Generally, we do a combination of T1 and some type of T2 sequences in all three orthogonal planes to show the different anatomic structures and pathologic entities well. The pulse sequences are chosen by selecting one of the following clinical categories:
- 1.
“Routine” (pain, trauma)
- 2.
Infection/mass
- 3.
Morton’s neuroma
We select from three anatomic regions for imaging:
- 1.
Ankle/hindfoot/midfoot
- 2.
Forefoot/toes
- 3.
Entire foot
- 1.
- •
Contrast: Gadolinium is used only in cases of suspected infection or for differentiating a solid from a cystic mass.
Normal and Abnormal
TENDONS
Tendon abnormalities affecting the foot and, particularly, the ankle are common because of the many tendons that are present and their close relationship to adjacent osseous structures that may cause irritation, and the frequent stresses and trauma affecting this anatomic location. Tendons generally are best evaluated on short axis axial images of the foot or axial images of the ankle where the tendons are depicted in cross section. Other imaging planes may help to substantiate findings in tendons, but do not show the tendons to greatest advantage because the tendons, with the exception of the Achilles tendon, run obliquely to these planes.
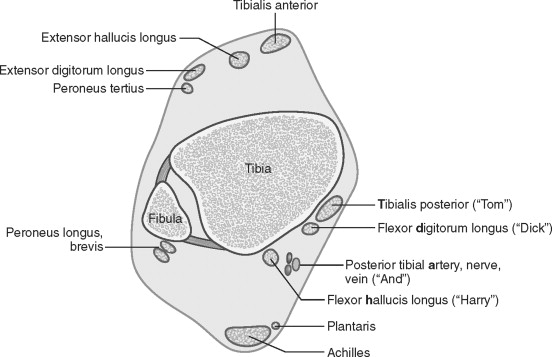
The general principles regarding the MRI appearance of normal and abnormal tendons are discussed in Chapter 3 . As a brief review, the abnormalities that may affect tendons are tenosynovitis, tendon degeneration, partial or complete tendon tears, subluxation or dislocation of certain tendons from their normal locations, xanthomas from hyperlipidemia, calcific tendinitis, uric acid tophi from gout, and, rarely, tumors. Tendons may tear as the result of chronic repetitive microtrauma; acute major trauma; and weakening secondary to myxoid degeneration, rheumatoid arthritis, chronic renal failure, diabetes, gout, steroids, and other medications. Abnormalities on MRI consist of fluid completely surrounding a tendon (tenosynovitis), abnormal tendon size, intratendinous high signal intensity (from partial tears), abnormal position (from dislocation), or complete absence of a segment of tendon (complete tear). Tendons of the ankle are conveniently divided into four groups, based on their location in the ankle: anterior, posterior, medial, and lateral ( Fig. 16-1 ).
POSTERIOR ANKLE TENDONS
Achilles and Plantaris ( Box 16-2 )
The Achilles tendon is located in the midline of the posterior ankle and is the largest tendon in the body, formed by the confluence of tendons from the gastrocnemius and the soleus muscles ( Fig. 16-2 ). The Achilles tendon is normally low signal intensity diffusely; however, there is a vertically oriented line of high signal intensity in many Achilles tendons that probably represents a normal interface between the two components of the tendon (gastrocnemius and soleus) or else small vessels within the tendon. The Achilles does not have a tendon sheath because it does not come into close contact with other structures along its length; it cannot have changes of tenosynovitis, but only of paratendinitis. There is a paratenon present on the dorsal, medial, and lateral aspects of the Achilles tendon that allows smooth gliding of the tendon in lieu of a tendon sheath. This may be seen on axial images as a thin line of intermediate signal intensity paralleling the posterior tendon. Anterior to the Achilles tendon is a triangular fat pad called Kager’s triangle .
- •
No sheath, but a posterior paratenon
- •
Xanthomas
- •
Tears at midpoint, and proximal or distal extremes
- •
Plantaris medially may simulate tear
- •
“Pump bumps” or Haglund’s deformity
- •
Retrocalcaneal bursitis
- •
Achilles tendon bursitis
- •
Thickened distal Achilles
- •

The Achilles tendon usually has a flat or concave anterior margin on axial images (see Fig. 16-2 ); if it becomes diffusely convex, an abnormally thickened tendon exists. The anterior margin of the Achilles tendon normally may have a focal convexity that starts on the lateral side of the proximal tendon and shifts to the medial aspect of the distal tendon. This focal anterior contour convexity is caused by the fibers of the soleus merging with those of the gastrocnemius in a spiral configuration as they extend to insert on the calcaneus. The posterior margin of the Achilles has a convex contour. The normal tendon measures about 7 mm in the anteroposterior dimension, and the anterior and posterior margins are parallel on true sagittal images through the tendon.
Ninety percent of individuals have a small plantaris tendon lying anteromedial to the Achilles tendon, which inserts onto the Achilles tendon, or to the posterior calcaneus, or to the flexor retinaculum ( Fig. 16-3 ). The high signal intensity plane between the plantaris and the Achilles tendons can be mistaken for a partially torn Achilles when none exists, or a completely torn Achilles may mistakenly be considered to have some remaining intact medial fibers, which are merely the fibers of the intact plantaris tendon. Evaluation of adjacent axial images distinguishes between a normal plantaris tendon and an abnormal Achilles tendon.

Degeneration and partial or complete tears of the Achilles tendon usually occur about 4 cm above its calcaneal insertion ( Fig. 16-4 ), but may exist anywhere along the length of the tendon. Tears also may occur at the musculotendinous junction ( Fig. 16-5 ), and the field of view must be large enough to include this region on sagittal images to look for hemorrhage and edema in the acute state, or muscle atrophy in the chronic setting.


Unconditioned, middle-aged athletes (“weekend athletes”) are most commonly affected with Achilles tendon abnormalities. Complete tears are usually easy to diagnose clinically, but some clinicians believe that there is still a valuable role for imaging in these patients to evaluate how close the tendon fragments are to one another and the condition of the tendon. Imaging may be done with a cast in place, which serves to hold the ankle in plantar flexion and cause increased apposition of tendon fragments. If there is a large gap between fragments, many orthopedists perform surgery to repair the tendon, whereas close apposition of tendon fragments can be treated with casting only. As with all things orthopedic, there is debate regarding the ideal method of treating these injuries.
Xanthomas occur from familial hyperlipidemia types II and III (hypercholesterolemia and hypertriglyceridemia) and have a predilection for the Achilles tendon (and the extensor tendons of the hands). Infiltration between the low signal intensity tendon fibers by intermediate signal intensity, lipid-laden foamy histiocytes causes a stippled pattern and either focal or diffuse enlargement of the tendon ( Fig. 16-6 ). The findings often are bilateral and cannot be distinguished from partial tendon tears on MRI. This must be remembered among the differential diagnostic possibilities for an abnormal Achilles tendon because the first manifestation of this deadly disease may be that of an Achilles xanthoma. The diagnosis may be proved with laboratory work-up.

Two bursae relate to the distal attachment of the Achilles tendon: the retrocalcaneal bursa and bursa of the Achilles tendon. The retrocalcaneal bursa is a teardrop-shaped structure that is normally located between the tendon and the posterior aspect of the upper calcaneus; it has little or no fluid within it when not inflamed. The bursa of the Achilles tendon (retro-Achilles) is an acquired or adventitious bursa, located just posterior to the distal Achilles tendon in the subcutaneous fat. Distention of these bursae with fluid or inflammatory thickening of the synovial linings indicates bursitis. If these bursae become inflamed, they may be a source of heel pain. Inflammation occurs with chronic overuse, especially from ill-fitting footwear, and from inflammatory arthropathies. The triad of retro-Achilles bursitis, retrocalcaneal bursitis, and thickening of the distal Achilles tendon is known as Haglund’s deformity, or as “pump bumps,” because wearing high-heeled or ill-fitting shoes is considered a predisposing factor ( Fig. 16-7 ).

MEDIAL ANKLE TENDONS
The flexor tendons are located on the medial side of the ankle (see Fig. 16-1 ). The position and names of these tendons can be easily remembered by using the mnemonic “ T om, D ick, A nd H arry” to represent the structures running from medial to lateral. “ T om” represents the posterior t ibial tendon; “ D ick” is the flexor d igitorum longus tendon; “ A nd” is the posterior tibial a rtery, nerve, and vein; and “ H arry” is the flexor h allucis longus tendon. The tendons are surrounded by separate tendon sheaths, and they pass through the tarsal tunnel, discussed subsequently.
Posterior Tibial Tendon ( Box 16-3 )
The posterior tibial tendon is the largest of the three medial flexor tendons. It has an oval shape and is approximately twice as large as the adjacent round flexor digitorum and flexor hallucis longus tendons. The posterior tibial tendon passes beneath the medial malleolus, which it uses as a pulley, and attaches to the medial navicular bone, the three cuneiforms, and the bases of the first to fourth metatarsals. The attachment to the navicular bone is generally the only portion of the attachment identified by MRI. Because of the orientation of the tendinous attachment and the multiple tendon slips that attach to the bone, the attachment often has the appearance of a thickened tendon with high signal intensity within it; this normal appearance must not be confused with a partial tendon tear.
- •
Most commonly abnormal medial tendon
- •
May tear or dislocate
- •
Tears lead to flat foot
- •
Tears associated with sinus tarsi syndrome
- •
Tears more common with accessory navicular
Most posterior tibial tendon tears occur at the level of the medial malleolus, rather than more distally. Generally, we disregard high signal in this tendon at its attachment site to the navicular because it typically is seen as a normal variant. High signal intensity or tendon thickening elsewhere in the length of the tendon is considered pathologic ( Fig. 16-8 ). A longitudinal split tear of this tendon is commonly seen, in which case the axial images appear to show two posterior tibial tendons ( Fig. 16-9 ). Fluid-bright T2 signal in the posterior tibial tendon, as in any tendon, indicates a partial tear ( Fig. 16-10 ), as does thinning or attenuation of the tendon ( Fig. 16-11 ).




The posterior tibial tendon is the most common abnormal tendon on the medial side of the ankle. This tendon provides a significant amount of support to the arch of the foot, and tears of the tendon can cause loss of the longitudinal arch, resulting in a flatfoot deformity. Middle-aged or older women and rheumatoid arthritis patients often have this abnormality.
There is a much higher incidence of posterior tibial tendon tears in individuals with accessory navicular bones or individuals with large medial tubercles of the navicular bone (the cornuate process), which result in altered stresses and premature tendon degeneration. Three types of accessory naviculars have been described. Type I is a small sesamoid bone within the posterior tibial tendon near its insertion onto the navicular. No increased incidence of tendon pathology is associated with a type I accessory navicular. Type II is a large secondary ossification center that is present in about 10% of the population and normally has a fibrous or cartilaginous attachment to the navicular. With trauma (either overt trauma or repeated microtrauma), it can separate and become painful. Bony edema and high T2 signal can be seen between the os naviculare and the navicular bone ( Fig. 16-12 ). A Kidner procedure is a common surgical procedure often performed to remove the os naviculare and reattach the posterior tibial tendon to the navicular bone.

Secondary signs of a posterior tibial tendon tear have been reported and include loss of the longitudinal arch of the foot and a small spur or periosteal reaction along the posterior aspect of the medial malleolus. Tears of this tendon also are associated with the sinus tarsi syndrome and degenerative joint disease of the posterior subtalar joint, which may serve as sources of pain.
A high percentage of patients with a torn posterior tibial tendon have an abnormal spring ligament, which lies just deep to the posterior tibial tendon and contributes to supporting the longitudinal arch of the foot. The spring ligament is discussed in the section on medial ligaments. The posterior tibial tendon rarely can sublux or dislocate in a medial and anterior direction relative to the medial malleolus.
Flexor Digitorum Longus
The flexor digitorum longus tendon is rarely involved with abnormalities. It passes just lateral to the posterior tibial tendon and divides to send insertions to the plantar aspects of the distal phalanges of the second through fifth toes.
Flexor Hallucis Longus ( Box 16-4 )
The flexor hallucis longus tendon is the most lateral of the three medial flexor tendons (see Fig. 16-1 ). It passes in a groove on the medial side of the posterior process of the talus, and then beneath the sustentaculum tali, which it uses as a pulley. It passes along the plantar aspect of the foot, between the hallux sesamoids at the head of the first metatarsal, to attach to the base of the distal phalanx of the great toe. The flexor hallucis longus synovial tendon sheath is in communication with the ankle joint in 20% of individuals; fluid surrounding the tendon is common and may have no significance if an ankle joint effusion also is present ( Fig. 16-13 ). This tendon tends normally to have more fluid in its sheath than do the adjacent two tendons.
- •
Rarely tears
- •
Sheath communicates with ankle (20%)
- •
Asymptomatic tendon sheath fluid common
- •
- •
Proximal tenosynovitis
- •
Repeated plantar flexion (ballet, basketball)
- •
Os trigonum syndrome
- •
- •
Distal tenosynovitis/partial tears
- •
Running, ballet
- •

Focal, asymmetric pooling of fluid within the tendon sheath is indicative of stenosing tenosynovitis, which occurs as the result of focal areas of synovitis or fibrosis within the tendon sheath, interrupting normal synovial fluid flow ( Fig. 16-14 ). Stenosing tenosynovitis of the flexor hallucis longus often is associated with the os trigonum syndrome, which occurs with extreme plantar flexion and causes the os trigonum and the flexor hallucis longus tendon to be trapped between the posterior malleolus of the tibia and the calcaneus. Tears of the flexor hallucis longus tendon at the level of the ankle are rare, and tenosynovitis is far more common. Repeated plantar flexion of the ankle and foot, as occurs in ballet dancers and basketball players, results in inflammatory changes to the sheath of this tendon.

The distal end of the flexor hallucis longus tendon may be partially torn or may develop tenosynovitis where it passes through the confined space between the hallux sesamoid bones ( Fig. 16-15 ). These distal tendon injuries are common in runners and in ballet dancers who dance en pointe.

LATERAL ANKLE TENDONS
Peroneal Tendons ( Boxes 16-5 and 16-6 )
The peroneus brevis and longus tendons are located on the posterolateral aspect of the ankle and serve as the major everters of the foot (see Fig. 16-1 ). These tendons pass posterior and inferior to the lateral malleolus, which they use as a pulley. The tendons share a common tendon sheath proximally, but have separate sheaths distally. The brevis usually is located anterior to the longus (although the brevis sometimes may lie medial to the longus) and runs in a shallow retromalleolar groove on the back of the lateral malleolus ( Fig. 16-16 ). The peroneal tendons are held in place relative to the lateral malleolus by the superior peroneal retinaculum. The tendons often are separated by the small peroneal tubercle on the lateral aspect of the calcaneus, with the brevis passing anterior to the tubercle (see Fig. 16-16 ), or both tendons may pass anterior to the peroneal tubercle. The brevis eventually attaches to the base of the fifth metatarsal. The longus has a broad-based insertion on the plantar surface of the base of the first metatarsal and medial cuneiform, after traversing the plantar aspect of the foot.
- •
Brevis anterior or medial to longus
- •
Brevis: Flat or oval is normal; curved (boomerang shape) is abnormal
- •
Tear or dislocate laterally
- •
Calcaneal fractures cause entrapment, displacement, and tenosynovitis
- •
Vertical tendon tear at level of tip of lateral malleolus
- •
Elderly: Often asymptomatic
- •
Young: Lateral pain, swelling
- •
- •
Caused by increased wear and tear of tendon
- •
Entrapment between peroneus longus and fibula in dorsiflexion
- •
Chronic tendon subluxation from torn retinaculum
- •
Flat or convex posterior aspect of lateral malleolus (predisposes to subluxation)
- •
Low-lying brevis muscle belly or peroneus quartus accessory muscle (causes compression of brevis)
- •
- •
Pitfalls
- •
Bifurcate brevis tendon or peroneus quartus may simulate
- •
Distinguish by: Split tendon has one muscle belly with two tendons coming from it
- •

The peroneus brevis and longus tendons may be difficult to distinguish as separate structures at the level of the lateral malleolus on MRI. The brevis generally is much flatter and broader than the longus, which has a more rounded appearance (see Fig. 16-16 ). Flat is acceptable (for many things), but if the brevis becomes C-shaped, it is considered abnormal.
Calcaneal fractures can be associated with peroneal tendon abnormalities, including entrapment of the peroneal tendons between bone fragments, tendon tears, tendon displacement, or impingement on tendons by fracture fragments. Complete and partial tears also occur in the absence of calcaneal fractures.
Peroneus brevis splits is a term used for longitudinal or vertical tears of the peroneus brevis tendon that can occur in all ages and in athletes ( Fig. 16-17 ). Tears occurring in the elderly may be asymptomatic, whereas younger patients usually have pain and swelling along the lateral malleolus and the course of the peroneal tendons. A history of recurrent inversion injuries and ankle sprains is common. The lateral collateral ligaments have a high association of tears with split tears of the peroneus brevis. The diagnosis is difficult or impossible clinically and overlaps with chronic ankle instability symptoms. Patients who do not respond to conservative management may benefit from surgery with anastomosis of fragments or tenodesis to the peroneus longus tendon.

Peroneus brevis longitudinal tears occur during dorsiflexion, when the brevis tendon is wedged between the lateral malleolus and the peroneus longus tendon. The tear originates at the distal tip of the lateral malleolus, but may propagate variable distances proximally and distally. The peroneus longus tendon also is partially torn in about 30% of individuals with a brevis tear because it becomes directly exposed to the lateral malleolus and subjected to abnormal stresses. A sharp posterolateral fibular spur may be seen with the peroneus brevis splits, representing a reactive periostitis.
Certain conditions are associated with peroneus brevis longitudinal tears. Anything that causes compression or subluxation of the peroneal tendons may predispose to this abnormality by causing increased wear and tear on the tendons. Such conditions include a torn or lax superior peroneal retinaculum, a flat or convex (rather than normal concave) posterior aspect of the lateral malleolus, low-lying peroneus brevis muscle belly (extending to the tip of the lateral malleolus), and the presence of an accessory muscle called the peroneus quartus .
The diagnosis of a longitudinal split of the peroneus brevis tendon may be simulated by the presence of a bifurcated distal peroneus brevis tendon or by the peroneus quartus accessory muscle and tendon ( Fig. 16-18 ). A brevis tendon tear can be distinguished from these two muscle variants, owing to the fact that separate muscle bellies surround each of the tendon slips in the case of a bifurcate brevis tendon, and a muscle belly separate from the peroneus brevis muscle is seen when a peroneus quartus is present. With a peroneus brevis split, there is one muscle belly and two tendons coming from it.

The peroneal tendons are among the few tendons that can sublux or dislocate; this occurs when the superior retinaculum has been disrupted. The retinaculum becomes disrupted from a forced inversion injury with plantar flexion, typically occurring in skiing, basketball, or soccer injuries. The diagnosis is made on MRI if the tendons are located lateral to the distal fibula, instead of posterior to it, or if the torn retinaculum is identified ( Fig. 16-19 ). A shallow or hypoplastic retromalleolar groove of the fibula may predispose to subluxation of the peroneal tendons.

The peroneus longus tendon has a sesamoid bone, the os peroneus, in about 10% of cases. This bone can serve as a stress riser with pain and eventual tendon disruption. This has been called painful os peroneus syndrome . Edema can be seen on MRI in the os peroneus just before the peroneus longus tendon enters the cuboid tunnel ( Fig. 16-20 ). Before the advent of MRI, a torn peroneus longus could be diagnosed with plain films by noting proximal migration of an os peroneus compared with prior films (like we might notice that). With MRI, painful os peroneus syndrome can be diagnosed before the tendon ruptures, which facilitates surgical treatment.

ANTERIOR ANKLE TENDONS
Four tendons can be found anterior to the ankle (see Fig. 16-1 ). From medial to lateral these are the anterior tibial, extensor hallucis longus, extensor digitorum longus, and peroneus tertius tendons. These tendons dorsiflex the ankle and foot. These tendons seldom are affected with pathology compared with the flexor tendons, so little attention is paid to these structures.
Anterior Tibial Tendon ( Box 16-7 )
The anterior tibial tendon is the most likely of all of the anterior tendons to be abnormal. This tendon is the most medial and the largest of the anterior tendons. Tears are uncommon, but may be seen with increasing age and in individuals who run on hills. Occasionally, patients with a partial or complete tear of this tendon present with a mass suspected to be a tumor, rather than with symptoms of a tendon abnormality ( Fig. 16-21 ), but most are diagnosed clinically before imaging. Imaging is done to see how much tendon retraction is present.
- •
Most commonly abnormal anterior tendon
- •
Tears occur from age or running hills
- •
Tears often present as a mass

ANKLE LIGAMENTS
MRI is not routinely used to diagnose ligamentous injuries because they usually can be easily and less expensively diagnosed by clinical examination. In patients who have persistent pain, or who may be imaged for seemingly unrelated reasons, the ligaments need to be evaluated and well understood because abnormalities can be identified and may have clinical significance. Also, it is becoming apparent that many ligament abnormalities are associated with other causes of chronic ankle pain (eg, sinus tarsi syndrome). One must be able to identify ligament pathology on MRI. Generally, the ligaments are thin, taut, low signal intensity structures; however, the thick bands of collagen may predictably create a striated appearance in certain ligaments, including the anterior tibiofibular, the posterior talofibular, and the deep (tibiotalar) and superficial (tibiocalcaneal) layers of the deltoid. The striated appearance in these ligaments must not be confused with partial tears.
Medial Ankle Ligaments
The medial collateral ligamentous complex (deltoid ligament) lies deep to the medial flexor tendons. It has several components—tibiotalar, tibiocalcaneal, talonavicular, and the spring ligament (between the sustentaculum of the calcaneus and navicular bone); the first two of these components routinely are seen well on coronal MR images ( Fig. 16-22 ). The deep tibiotalar portion of the deltoid ligament is seen as a striated structure coursing obliquely between the medial malleolus and the talus on coronal and axial images, usually best on the coronal images. The tibiocalcaneal component of the deltoid runs vertically, just deep to the flexor retinaculum and superficial to the tibiotalar component of the ligament. The deltoid ligament is only infrequently injured compared with the lateral ankle ligaments.

The MRI appearance of a deltoid ligament injury depends on which components were injured and to what extent ( Fig. 16-23 ). The tibiotalar component often loses its striated appearance and shows high signal intensity on T1W and T2W images. This appearance may indicate either a contusion or a tear of the ligament. The tibiocalcaneal portion may be discontinuous and have high signal intensity hemorrhage and edema acutely; a chronic tear may appear as a thickened or discontinuous ligament.

The spring ligament, also called the tibio-spring ligament , arises from the medial malleolus as the medialmost portion of the deltoid. It extends inferiorly just deep to the posterior tibial tendon and then curves medially to support the head of the talus and inserts onto the sustentaculum tali ( Fig. 16-24 ). Although we simplistically think of the spring ligament as having a J shape and supporting the head of the talus like a sling or a hammock, it is more complex than that. Three portions of the spring ligament have been described, but we typically do not identify each portion separately on MRI.

An abnormal spring ligament is often associated with a torn posterior tibial tendon. The posterior tibial tendon and the spring ligament help support the longitudinal arch, and when the posterior tibial tendon fails to hold its share of the load, the spring ligament cannot support the arch by itself, so it too fails. An abnormal spring ligament is identified with MRI if it is unusually thickened or has intermediate signal within it on T1W or T2W sequences ( Fig. 16-25 ). A torn spring ligament is identified by noting a gap in the tendon ( Fig. 16-26 ).


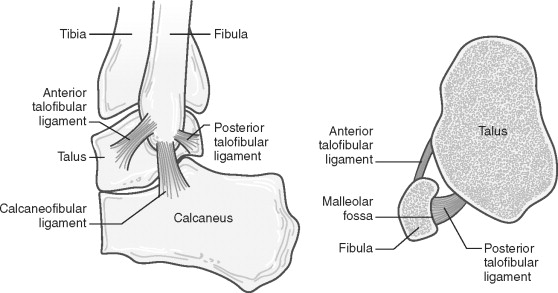
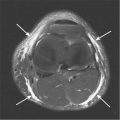
Lateral Ankle Ligaments ( Box 16-8 )
The lateral collateral ligamentous complex is affected in 80% to 90% of all ankle ligament injuries. Generally, these ligaments are best evaluated on axial images. The superiorly located lateral ligaments include the anterior and posterior tibiofibular ligaments, which are located just above the tibiotalar joint ( Fig. 16-27 ). These ligaments course superiorly from the fibula to the tibia (or inferiorly from the tibia to the fibula). The anterior and posterior tibiofibular ligaments, along with the interosseous membrane between the tibia and fibula, compose the syndesmosis. These ligaments are seen well on axial images and often are seen on coronal images also (see Fig. 16-27 ). These ligaments often are best identified on an axial cut that passes through the dome of the talus; this should not cause confusion in thinking that the cut is too distal to be the tibiofibular ligaments. On sagittal images through the ankle, the posterior tibiofibular ligament cut in cross section may resemble an intra-articular loose body in the ankle because it is surrounded by ankle joint fluid (see Fig. 16-27D ). Following the structure on adjacent cuts and its predictable location at the level of the tibiotalar joint makes the differentiation between pathology and normal anatomy possible. The tibiofibular ligaments can be torn, and this is recognized by discontinuity of the low signal structures on axial MR images ( Fig. 16-28 ).
Superior Group
- •
Anterior and posterior tibiofibular ligaments
- •
Seen at top of ankle joint on axial images
- •
Posterior tibiofibular ligament mimics ankle loose body on sagittal images
- •
Inferior Group
- •
Anterior to posterior: Anterior talofibular, calcaneofibular, posterior talofibular
- •
Calcaneofibular: Best seen on coronal images, but seen inconsistently
- •
Anterior and posterior talofibular: Seen on axial images at level of malleolar fossa of fibula
- •
Usually tear in sequence from anterior to posterior
- •
Tears associated with
Osteochondral fractures
Long-term instability
Sinus tarsi syndrome
- •



The second set of lateral ligaments is located just distal to the tibiotalar joint. This inferior set of ligaments is made of the anterior talofibular, calcaneofibular, and posterior talofibular ligaments, from anterior to posterior ( Fig. 16-29 ). The anterior and posterior talofibular ligaments are seen best on axial images just below the tibiotalar joint at the level of the concavity in the medial aspect of the lateral malleolus, called the malleolar fossa ( Fig. 16-30 ). The calcaneofibular ligament is the most difficult ligament to identify routinely and may be best seen on coronal images (see Fig. 16-30 ).