Chapter 8 Foot, toes, ankle, tibia and fibula
Foot and toes
Indications
Examination of the foot for trauma should only be performed if there is true bony tenderness; the demonstration of a fracture rarely influences management.1 Examination of the foot for hallux valgus is not indicated unless it is for preoperative assessment.
Lisfranc injuries
These are traumatic subluxations or dislocations at the base of the metatarsals at the tarsometatarsal joints, with or without fracture. This injury may involve some or all of the joints. The mechanism of injury can be from several incidents, such as the foot hitting the floor of a car in a road traffic accident, or missing a step or a kerb.2
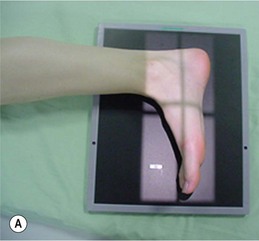
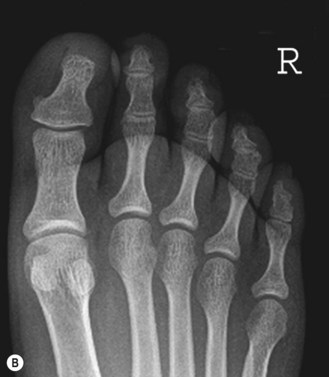
Dorsiplantar (DP) foot (Fig. 8.1A,B)
In both the DP and DP oblique positions, in order to enable the joint spaces between the tarsal bones to be demonstrated more clearly, a 15° cranial angle may be used.3 When using this projection the tarsometatarsal articulations are demonstrated without as much bony overlap as when a perpendicular central ray is used. However, careful consideration must be given when directing the tube towards the gonads, and adequate radiation protection must be used. The same image can be produced by using a 15° foam wedge directly under the foot, the thickest end being placed at the toe end; this removes the necessity for angulation of the central ray directly towards the gonads, but the image of the metatarsals and phalanges will be magnified if used in this way, as the object to receptor distance will vary along the length of the foot. An alternative is to position the pad under the image receptor (IR), which does remove the problem of magnification.
Positioning
• The patient is seated on the table with their legs extended and their hands are used to support themselves
• The patient’s knee on the side under examination is flexed and the plantar aspect of the foot is placed in contact with the IR
• The opposite leg is abducted and a lead rubber sheet is placed over the abdomen and pelvis for radiation protection
Criteria for assessing image quality
• Demonstration of the phalanges, metatarsals, navicular, cuboid and cuneiform bones and soft tissue shadowing of the outline of the foot
• Adjacent phalanges should be demonstrated separately with exception of the bases of metatarsals 2–5, which will be slightly overlapped. Toes of patients with toe deformities are unlikely to all be separated
• Shafts of the metatarsals separated
• Tarsal bones should appear overlapped
• Talus and calcaneum should be superimposed over the tibia and fibula
• Sharp image demonstrating the soft tissue margins, bony cortex and trabeculae of the phalanges, metatarsals and tarsus. The proximal calcaneum and talus will not be penetrated sufficiently to be demonstrated
| Common error | Possible reason |
|---|---|
| Superimposition of the lower leg over the tarsal bones | Knee may be too flexed, encouraging too much ankle flexion |
Dorsiplantar oblique (DPO) foot (Fig. 8.2A,B)
Positioning
• The plantar aspect of the foot is placed in contact with the IR
• From the DP position the patient’s foot is internally rotated to bring the plane of the dorsum of the foot parallel to the IR
• A radiolucent pad is placed under the lateral plantar aspect of the foot for immobilisation
• The opposite leg is abducted and a lead rubber sheet is placed over the abdomen and pelvis for radiation protection
Criteria for assessing image quality
• Demonstration of the phalanges, metatarsals, navicular, cuboid and cuneiform bones and soft tissue shadowing of the outline of the foot
• Adjacent phalanges are not likely to all be separated, due to obliquity, especially in the case of patients with toe deformities (i.e. ‘hammer toe’)
• Shafts of metatarsals 2–4 separated
• Overlap of the bases of the first and second metatarsals
• Separation of the tarsal bones, although the medial and middle cuneiforms will appear superimposed, with some overlap of middle and lateral cuneiforms
• Talus and calcaneum are clear of the tibia and fibula
• Sharp image demonstrating the soft tissue margins of the foot, bony cortex and trabeculae of the phalanges, metatarsals and tarsus
| Common errors | Possible reasons |
|---|---|
| Superimposition of the lower leg over the tarsal bones | Knee may be too flexed, or the foot may be under-rotated |
| Overlapping of metatarsals | Over-rotation of foot |
Lateral foot (Fig. 8.3A,B)
Positioning
• With the leg extended, it is externally rotated until the lateral aspect of the foot is in contact with the IR. This may be more comfortable if the knee is slightly relaxed and not fully extended. The plantar aspect of the foot is 90° to the IR
• Radiolucent foam pads may be placed under the lower leg and foot for support in this position
• A lead rubber apron is placed over the abdomen for radiation protection
Criteria for assessing image quality
• Demonstration of the phalanges, metatarsals, navicular, cuboid and cuneiform bones and soft tissue shadowing of the outline of the foot
• Phalanges should be superimposed; the distal phalanges of the longest toe (hallux or second toe) will lie clear
• Metatarsals should be overlapped, with the first metatarsal lying most superiorly and the fifth inferiorly
• Sharp image demonstrating the superimposition of the phalanges and metatarsals and the bony trabeculae of the tarsal bones, navicular, talus and calcaneum
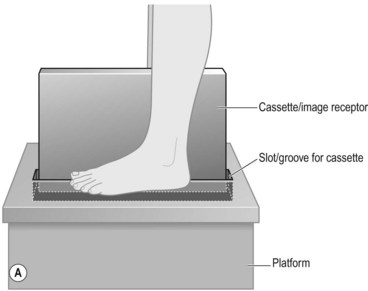
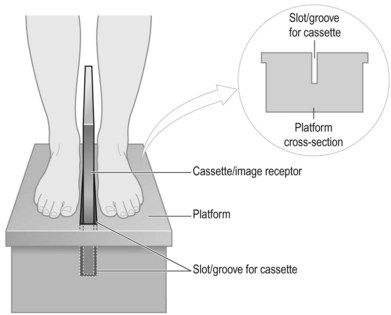
Weightbearing lateral foot (Fig. 8.4A,B)
This projection is usually performed as part of an orthopaedic assessment. It is important to include the whole length of foot on the image as the relationship between the joints of the tarsal bones and the metatarsals is an important indication of the degree of surgical intervention required following trauma. This is particularly important in Lisfranc injuries, where fracture dislocations are involved and a complete radiographic evaluation of the foot is required.2
A suitably designed platform is required for good radiography of this area. The platform should be made of radiolucent material, with a groove in the centre for positioning the IR vertically and to allow the IR to be placed at a level below the soft tissues of the plantar aspect of the foot to enable the soft tissues to be included on the image. The platform should be of a dimension to allow both feet to be placed comfortably on either side of the groove (Fig. 8.5). Most frequently these platforms are made as a bespoke design in hospital workshops, rather than obtained from commercial sources.
Positioning
• Stand the patient on the specially designed platform
• Ensure the patient is stable and suitable support is provided to allow even distribution of the weight of both feet
• Support the IR in the erect, transverse position in the groove of the platform on the medial aspect of the foot
• Use a sheet of lead or lead rubber between the back of the IR and the foot that is not under examination, for radiation protection
• The long axis of the foot should be parallel to the long axis of the IR
• A lead rubber apron is placed over the abdomen for radiation protection
Criteria for assessing image quality
• Distal phalanges, calcaneum, ankle joint and soft tissue outlines of the foot should all be demonstrated
• Phalanges should be superimposed, with the longest toe cleared as for non-weightbearing lateral
• Metatarsals should be overlapped as for the lateral foot
• Medial and lateral articular surfaces of the talus should be superimposed
• Sharp image demonstrating superimposition of the phalanges and metatarsals, bony trabeculae of the tarsal bones, navicular, talus and calcaneum. The soft tissue of the heel pad should not be over-blackened. kVp should be sufficient to reduce the subject contrast along the length of the foot
Toes
DP and DPO toes
It is often a requirement to examine all the toes, but most often toes 2–5, in one projection. Therefore, the description that follows gives the option to do this or to examine the toes individually. The practice of including other toes on an image is often used to establish which phalanx is being examined (see also the section on fingers in Ch. 5), but this involves irradiating areas that are not required for examination and it could be argued that this contravenes IR(ME)R 2006.4 Collimation to include just part of the adjacent toe either side may be sufficient for identification purposes.5
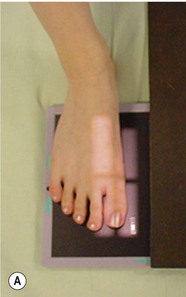
DP toe/toes (Figs 8.6A,B, 8.7A,B)
Positioning
• The patient is seated on the table with their legs extended and their hands are used to support themselves
• The patient’s knee on the side under examination is flexed and the plantar aspect of the toes is placed in contact with the IR
• The opposite leg is abducted and a lead rubber sheet is placed over the abdomen and pelvis for radiation protection
Centring point
To the individual toe under examination at the metatarsophalangeal joint (Fig. 8.6A) or between the second and third metatarsophalangeal joints if all the toes are to be included (Fig. 8.7A)
Criteria for assessing image quality
• All the phalanges and the distal half of the metatarsals should be included
• Symmetry of the phalangeal condyles
• Joint spaces of the interphalangeal joint spaces are demonstrated clearly. Separation of the toe or toes from the adjacent toes. Neither of these may be possible with patients with toe deformity
• Separation of adjacent metatarsal heads
• Sharp image demonstrating the soft tissue margins of the toe/toes, bony cortex and trabeculae of the phalange/s
DPO toes (Fig. 8.8A,B)
Positioning
• The patient is seated on the table with their legs extended and their hands are used to support themselves
• The plantar aspect of the toes is placed on the IR
• From the DP position the patient’s foot is internally rotated until approximately 30° to the IR
• A radiolucent pad is placed under the plantar aspect of the foot for immobilisation
• The opposite leg is abducted and a lead rubber sheet is placed over the abdomen and pelvis for radiation protection