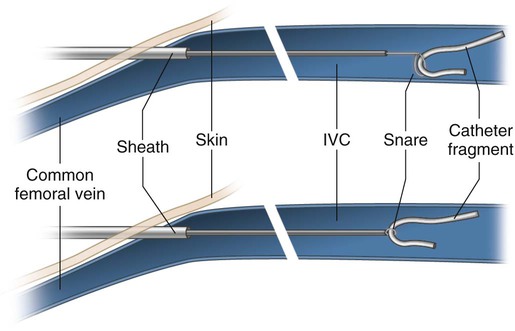
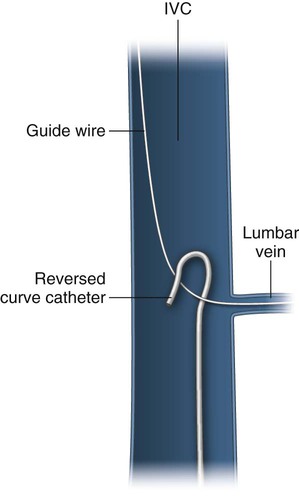
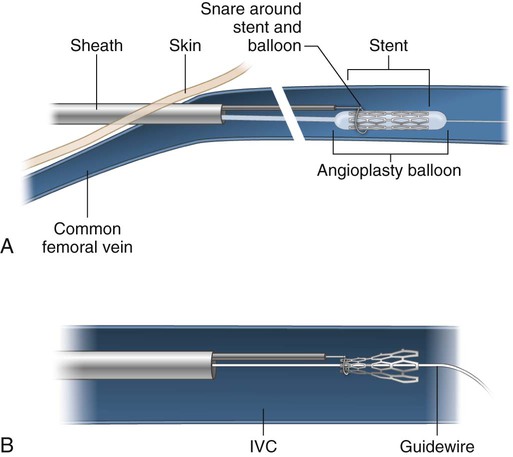
Foreign bodies left unattended in the vascular system have been associated with a 71% major complication rate and 24% to 60% mortality rate. Those located within the cardiopulmonary system pose the greatest risk. Foreign objects find their way into the vascular system through trauma, instrumentation, or transmural penetration from adjacent tissues (e.g., ingested foreign bodies). Upon arriving in the heart, wires, stents, inferior vena cava (IVC) filters and filter fragments can cause cardiac arrhythmias, septal or ventricular wall perforation, myocardial infarction, myocarditis, sepsis, pericardial effusion, and pericardial tamponade.1–6 Continued migration into the pulmonary arteries can result in thromboembolism and sepsis.7,8 Percutaneous techniques have dramatically altered the management of foreign bodies over the last several decades. Earliest reports of retrieving misplaced objects were limited to removal of catheter fragments and wires with a Dormia basket, forceps, or a self-made wire loop.9–13 Unable to be directed over a guidewire, baskets were difficult to manipulate into position. Stiff forceps were prone to traumatizing the vascular media, resulting in spasm, dissection, and perforation. Following reports of the less traumatic self-made wire loop, several improved devices became commercially available. This niche market of retrieval devices has since been driven by the increasing use of stents, filters, coils, and other intravascular devices. Medical literature relating to foreign body retrieval is limited to case reports and short series.14–19 This chapter will describe the rationale for removing foreign bodies and discuss the various techniques that can be used. The most commonly used retrieval devices today are snares. The Amplatz GooseNeck Snare (ev3/Covidien, Plymouth, Minn.) is constructed of a nitinol cable and a gold-plated tungsten loop.20 The snare’s superelastic construction prevents it from deforming during use. The platinum-iridium radiopaque marker band at the tip of the guiding catheter is highly visible under fluoroscopy. When fully deployed, the snare is oriented at a 90-degree angle with respect to the guiding catheter tip. It is cinched around the foreign body by holding it stationary and advancing the catheter forward. Amplatz GooseNeck Snares are available in 5- to 35-mm diameters. The Texan Foreign Body Retrieval Device (IDev Technologies, Houston, Tex.) consists of a dual-lumen catheter shaft, a push rod with a handle, and a nitinol wire loop.21,22 The smaller lumen is used for the loop wire. The larger lumen is used for either a 0.018-inch guidewire or contrast injection. The loop cinches down on the foreign body as the operator pulls back on the push rod. The loop wire opens at a 90-degree angle with respect to the shaft and can be adjusted from 0 to 30 mm in diameter, remaining perpendicular to the shaft throughout deployment. This 90-degree angle being maintained throughout snare deployment accounts for a major difference when compared with the Amplatz GooseNeck Snare, which achieves perpendicular orientation only after it is fully deployed from the catheter tip. Snares are successful in removing foreign bodies 95% of the time. Objects that are too large or noncompressible for removal through a vascular sheath can be relocated to a less noxious location or moved to a position that is easily accessible through a surgical cutdown.23 A guidewire is usually lost in the vascular system by an inexperienced operator who loses sight of the wire during dilator or catheter exchange while placing a central venous catheter.24 Catheter fragmentation usually occurs during catheter removal. Catheter shearing may also occur when the catheter is “pinched off” between the clavicle and the anterior portion of the first rib. Peripherally inserted central catheter (PICC) lines usually become torn when the peripheral arm vein goes into spasm during catheter removal. When a catheter of any type has become torn or is found incidentally on imaging or a wire has been lost, use of an endovascular snare becomes necessary.18 A vascular sheath is placed in either the internal jugular or common femoral vein. A long sheath provides greater support and stability for the snare. The snare is passed through the sheath and advanced or retracted over the fragment tip. The snare is then cinched and drawn out with the fragment through the sheath (Fig. 107-1). A fragment tip that is caught in a small branch vessel or chronically embedded in the vessel wall must first be freed from the vessel wall in order to be snared. A reverse curve catheter passed through the same sheath or a separate sheath can be used to pull down on the shaft of the foreign body, freeing the tip (Fig. 107-2). A braiding technique can also be used for this purpose.25 With this method, a pigtail catheter tip is wrapped around the fragment and rotated, braiding itself with the fragment and freeing the tip to allow successful snaring. The end of a fragment may sometimes extend into the subcutaneous tissues while remaining invisible at the skin surface. This occurs when the catheter is torn during attempted removal. With the help of fluoroscopy or ultrasound, one can incise the skin and dissect down onto the fragment. The fragment is then secured and extracted along with its intravascular component. An 18- to 20-gauge needle can be formed into a hook on the table for this purpose.26 If the tip of the foreign body is too deep for a safe or successful cutdown, the intravascular end of the fragment can be snared and removed through a vascular sheath, bringing the soft-tissue component along with it. Rarely, a catheter will become sutured to the wall of a vein during an operation. Snaring the catheter would risk tearing the vessel wall. In this setting, two vascular sheaths are placed via femoral and internal jugular access.27 One snare is passed through each sheath. The catheter is snared on each side of the suture, immediately adjacent to the suture. Steady, equal traction is applied to the catheter fragment from each direction until the fragment is torn into two pieces. Each fragment is subsequently removed through the sheaths. Because of the risks associated with this procedure, anesthesiology and surgery services should first be consulted. A self-expanding stent can migrate during deployment when the constrained stent is not centered on a stenosis and it “trumpets” or “melon seeds” in either direction during release. A stent can also migrate following a technically successful deployment in a vein as the vessel diameter increases with respirations or Valsalva maneuvers. Using a T-fastener to anchor an IVC stent to the wall of the intrahepatic IVC has been described in this setting.28 A stent may become irretrievable if left to migrate into the heart chambers, requiring open-heart surgery for its removal. Maintaining a guidewire through the lumen of a lost stent is key to its successful capture and removal. Keeping the wire in both the superior and inferior vena cavae will prevent the stent from passing into the heart chambers. The vascular sheath is exchanged for one that is wide enough to pull the captured stent through. The snare is cinched around the wire outside of the sheath. The snare and its guiding catheter are passed through the sheath along the guidewire. The snare is opened around the proximal-most end of the lost stent. The snare is then cinched down on the proximal end of the stent, drawing the constrained end of the stent out through the sheath.29 Having successfully passed a wire through the stent, the operator may still find it difficult to avoid hang-up of the snare on the struts at the end of the stent. Use of an angioplasty balloon will provide a transition zone for the snare to approach and slip over the end of the stent. The vascular sheath is first exchanged for an appropriately sized one. An angioplasty balloon 1 to 2 mm greater in diameter than the stent and longer than the stent is selected. A snare is cinched around the balloon catheter shaft outside of the sheath. The balloon/snare combination is passed over the wire just proximal to the stent. The snare is opened. The balloon is advanced into the stent and inflated. The open snare is advanced over the tapered end of the balloon and onto the proximal end of the stent (Fig. 107-3, A). The balloon is deflated and pulled out of the stent as the end of the stent is constrained by the snare (Fig. 107-3, B). The deflated balloon and captured stent are then drawn out sequentially through the sheath.
Foreign Body Retrieval
Introduction
Snares
Lost Guidewire and Catheter Fragments
Lost Endovascular Stents
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine