Chapter Outline
Even with the widespread availability of cross-sectional imaging studies, abdominal radiography remains a common imaging test in modern radiology practice. Although CT and ultrasound provide more information about acute abdominal conditions, abdominal radiography has the advantages of relatively low cost and ease of acquisition and can readily be performed on acutely ill or debilitated patients, so it remains a valuable study for the trained and perceptive observer. The abdominal radiograph has also been called a KUB— k idneys, u reters (which are not visible), and b ladder. The term flat plate of the abdomen is dated and refers to a time when glass plates were used to produce images. Other terms include plain film of the abdomen and abdominal plain film, but with the widespread use of digital imaging and picture archiving communication systems (PACS) for interpretation of the images, abdominal radiograph has become the most appropriate term.
A wealth of diagnostic information can be obtained from correct interpretation of abdominal radiographs, and several excellent texts are available on the subject. This chapter focuses on the abnormalities of gas and soft tissues that can be detected on abdominal radiographs.
Normal Bowel Gas Patterns
The intestinal tract in adults usually contains less than 200 mL of gas. Intestinal gas has three sources—swallowed air, bacterial production, and diffusion from the blood. In the supine patient, gas rises and accumulates in anteriorly placed segments of intestine, including the antrum and body of the stomach, transverse colon, and sigmoid colon. Gas may also be present in the remaining colon, particularly the rectum. Radiographic evaluation of intestinal gas should include the following: (1) identification of the bowel segments containing gas; (2) assessment of the caliber of these segments; (3) assessment of the most distal point of passage of gas; and (4) evaluation of the bowel contour outlined by gas.
The normal bowel gas pattern is readily visible on supine abdominal radiographs ( Fig. 12-1 ). The first collection of gas encountered from the top of the radiograph is usually in the antrum and body of the stomach. Gas may also be seen in the transverse colon immediately inferior to the stomach. Gas in the ascending and descending portions of the colon usually occupies the lateral margins of the peritoneal cavity. The sigmoid colon occupies the inferior aspect of the abdomen and is often recognized by its characteristic shape and haustral folds. Rectal gas occupies a midline position in the pelvis and generally extends to the level of the pubic symphysis. The gas-filled small bowel tends to occupy the central portion of the abdomen and has a smaller caliber than the colon.
Although the location of intestinal gas is helpful in differentiating colon from small bowel, recognition of intestinal folds is also important. Haustral folds in the colon are normally 2 to 3 mm in width and occur at intervals of 1 cm, whereas the circular small bowel folds (also known as plicae circulares) are 1 to 2 mm in width and occur at intervals of 1 mm. In general, the small bowel is smaller than 3 cm in diameter and the colon is smaller than 5 cm in diameter.
Intestinal gas is a natural contrast agent for the interpretation of abdominal radiographs. When the patient is in the supine position, the gastric antrum and body tend to distend with air. A long narrowed segment of air-filled stomach may indicate an infiltrating process such as linitis plastica. Gastric ulcers and masses are also occasionally visible ( Fig. 12-2A ). In the colon, gas may outline a narrowed lumen from ulcerative or granulomatous colitis, thickened haustral folds from ischemia ( Fig. 12-2B ), or even a polypoid or annular carcinoma (see Fig. 12-5A ).

Abnormal Bowel Gas Patterns
Gastric Outlet Obstruction
Gastric outlet obstruction may be manifested on abdominal radiographs by a dilated stomach containing air, fluid, and/or debris. The amount of gastric distention depends not only on the degree of obstruction, but also on the duration of obstruction, position of the patient, and frequency of emesis. A dilated, air-filled stomach is usually recognized without difficulty because of its characteristic shape and location associated with inferior displacement of the transverse colon. Occasionally, a massively dilated, fluid-filled stomach can mimic the appearance of ascites or hepatomegaly. A small amount of air is almost always present within the stomach, however, so an upright radiograph of the chest or abdomen should demonstrate an air-fluid level within the gastric lumen.
The distal gastric antrum and pyloric region are the usual sites of gastric outlet obstruction. The most common causes of obstruction include acute edema and spasm from an ulcer in the distal antrum or pyloric channel or chronic antral narrowing secondary to scarring from a previous ulcer. Other causes of gastric outlet obstruction include an infiltrating antral carcinoma and, less commonly, scarring from granulomatous disease, radiation, or previous caustic ingestion.
Not all patients with gastric distention have mechanical obstruction. The stomach may also be dilated because of gastroparesis or gastric atony from diabetes (gastroparesis diabeticorum), which is almost always associated with a peripheral neuropathy. Other causes of gastric dilation include morphine and other narcotic agents, hypokalemia, uremia, porphyria, lead poisoning, and previous truncal vagotomy. Pancreatitis or gastritis may also result in reflex gastric atony, and general anesthesia may occasionally cause marked gastric dilation.
Patients with obstructive lesions in the duodenum may also present with findings of gastric outlet obstruction. The duodenum may be filled with fluid, so it is not readily visible on supine radiographs. Left lateral decubitus views of the abdomen may allow air to enter the dilated duodenum, indicating that the obstruction is distal to the pylorus. When fluoroscopic barium studies are performed in patients with suspected gastric outlet obstruction, the duodenum should be carefully examined if the stomach appears normal.
Adynamic Ileus
The term adynamic ileus refers to dilated bowel in the absence of mechanical obstruction. It is used synonymously with the terms paralytic ileus and nonobstructive ileus. A more specific term, postoperative ileus, is limited to patients in whom recent abdominal surgery is responsible for this condition. All these terms refer to a state of decreased or absent intestinal peristalsis, causing swallowed air to accumulate in dilated bowel. An adynamic ileus is typically manifested on abdominal radiographs by a dilated small bowel and colon, with multiple air-fluid levels on upright or horizontal beam decubitus views, so the presence of a dilated colon allows this condition to be differentiated from mechanical small bowel obstruction, in which only the small bowel is affected (see later, “ Small Bowel Obstruction ”). Sometimes, however, an adynamic ileus is confined to the small bowel, mimicking the findings of small bowel obstruction ( Fig. 12-3 ), so the absence of colonic distention in no way excludes this condition. Apart from recent abdominal surgery, an adynamic ileus may result from a wide variety of causes, including electrolyte imbalances, sepsis, generalized peritonitis, blunt abdominal trauma, and infiltration of the mesentery by tumor.

Other patients may have a localized ileus (also known as a sentinel ileus) related to acute inflammatory conditions in adjacent areas of the abdomen, including the right lower quadrant in patients with appendicitis, left lower quadrant in patients with diverticulitis, right upper quadrant in patients with cholecystitis, and mid upper abdomen or left upper quadrant in patients with pancreatitis.
Small Bowel Obstruction
Small bowel obstruction is often difficult to diagnose on abdominal radiographs. False-positive and false-negative rates of 20% have been reported in the diagnosis of small bowel obstruction based solely on the radiographic findings. The diagnostic sensitivity can be increased by correlating the radiographs with the presence or absence of bowel sounds. Sequential radiographs over 12 to 24 hours may be helpful in demonstrating an evolving obstructive pattern.
When the small intestine becomes completely obstructed, accumulation of swallowed air and intestinal secretions causes proximal dilation of bowel. At the same time, intestinal peristalsis progressively eliminates bowel contents distal to the site of obstruction within 12 to 24 hours. As a result, small bowel obstruction is typically characterized on supine abdominal radiographs by dilated, gas-filled small bowel loops larger than 3 cm in diameter, with little or no gas in the colon or small bowel distal to the site of obstruction ( Fig. 12-4A ). Upright and decubitus abdominal radiographs typically reveal multiple air-fluid levels in the dilated small bowel because of accumulation of gas and fluid proximal to the obstruction ( Fig. 12-4B ).

In his classic work on the acute abdomen, Frimann-Dahl stated that the presence of air-fluid levels at two different heights in the same loop of small bowel indicates a hyperperistaltic small intestine and is therefore a sign of small bowel obstruction. However, subsequent investigators have found that differential air-fluid levels may be present in any tubular viscus containing air and fluid. Thus, air-fluid levels should be recognized as a nonspecific finding that can be seen with a mechanical obstruction or adynamic ileus.
As small bowel obstruction progresses, gas-filled small bowel loops proximal to the site of obstruction become more dilated and tend to have a horizontal orientation in the central portion of the abdomen, producing a classic stepladder appearance. However, the amount of gaseous distention of these loops depends not only on the degree of obstruction, but also on the duration of obstruction, amount of air swallowing or emesis, and use of nasogastric suction for decompression. In some patients with small bowel obstruction who swallow relatively little air, supine abdominal radiographs may be unrevealing, whereas upright or decubitus abdominal radiographs (i.e., horizontal beam views) will show multiple air-fluid levels within small bowel loops proximal to the site of obstruction. In other patients, small amounts of gas trapped between the small bowel folds on upright or decubitus abdominal radiographs may be recognized by tiny bubbles of gas lined up along the nondependent surface of the bowel, also known as the string of pearls or string of beads sign (see Fig. 12-4B ). This sign is seldom seen in patients with an adynamic ileus and should therefore suggest a mechanical small bowel obstruction. Finally, when patients swallow little or no air, abdominal radiographs may reveal multiple tubular, sausage-shaped soft tissue densities representing fluid-filled loops of small bowel without any intraluminal gas in the small bowel or colon, producing a so-called gasless abdomen. In general, the absence of colonic gas should suggest the possibility of a developing small bowel obstruction because gas is normally present in the colon in the absence of obstruction.
Most small bowel obstructions are caused by postoperative adhesions. Such adhesions may occur as early as 1 week after surgery, but more typically there is a remote history of surgery. In the absence of a surgical history, an obstructing hernia should be suspected. Of these hernias, 95% are external (inguinal, femoral, umbilical, or incisional). The presence of air-filled bowel below either pubic ramus should suggest the possibility of an obstructing inguinal hernia. Other less common causes of small bowel obstruction include small bowel tumors, ectopic gallstones, acute appendicitis and, occasionally, intestinal parasites or bezoars.
It may not be possible to distinguish mechanical obstruction from an adynamic ileus on the basis of a single set of abdominal radiographs. If immediate surgery is not contemplated, further radiographic work-up with computed tomography (CT) is usually indicated. This topic is discussed in detail in Chapter 46 . Barium studies may also be helpful when abdominal radiographs reveal findings of low-grade or partial small bowel obstruction.
Colonic Ileus
Acute colonic pseudo-obstruction (also known as Ogilvie’s syndrome) was first described in 1948 by Ogilvie, who postulated that progressive colonic dilation is caused by interruption of sympathetic innervation with unopposed parasympathetic innervation of the colon. The most common clinical presentation is acute abdominal distention, usually occurring within 10 days of the onset of the precipitating pathologic process. Intra-abdominal inflammation, alcoholism, cardiac disease, burns, retroperitoneal disease, trauma, and pregnancy with spontaneous delivery or cesarean section have been described as causes of Ogilvie’s syndrome.
Abdominal radiographs may reveal marked colonic distention, which is typically confined to the cecum, ascending colon, and transverse colon. Occasionally, however, gas may extend to the level of the sigmoid colon. The underlying clinical condition and rapid onset of colonic distention usually suggest the diagnosis of colonic pseudo-obstruction, but a limited contrast enema may be required to rule out obstructing lesions in the colon.
Prediction of impending perforation of the cecum, as judged by cecal diameter, is fraught with difficulty because the risk of cecal perforation depends not only the degree of distention, but also on the duration—that is, the risk is considerably less in patients with long-standing cecal distention than in those with an acute increase in cecal caliber. Although some authors have indicated that a cecal diameter of 9 to 12 cm suggests impending perforation, cecal diameters of 15 to 20 cm are commonly observed in patients who recover spontaneously from Ogilvie’s syndrome. Serial radiographs showing a change in cecal diameter at 12- to 24-hour intervals may be more helpful than a single radiograph showing a dilated cecum. Intravenous (IV) neostigmine is sometimes used for the initial treatment of these patients. Prolonged cecal distention beyond 2 to 3 days should prompt colonoscopic or surgical decompression. The presence of intramural gas in the region of the dilated cecum should strongly suggest infarction and impending perforation.
Colonic Obstruction
More than 50% of colonic obstructions are caused by annular carcinomas of the colon. The obstruction usually occurs in the sigmoid colon, where the bowel tends to have a narrower caliber and the stool is more solid. Conversely, cecal carcinomas and those in the ascending colon are less likely to cause obstruction because of the wider caliber of the bowel and more liquid character of the stool.
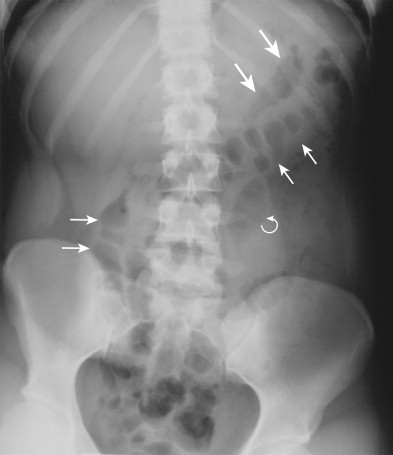
Colonic obstruction is typically manifested on abdominal radiographs by dilated, gas-filled loops of colon proximal to the site of obstruction and a paucity or absence of gas in the distal colon and rectum ( Fig. 12-5A ). Air-fluid levels may be seen on upright or decubitus views ( Fig. 12-5B ). Abdominal CT may be performed to confirm the presence of obstruction and determine its underlying cause ( Fig. 12-5C ). In patients with a competent ileocecal valve, the colon (especially the cecum) may become markedly dilated, and little or no gas may be seen in the small bowel. As the cecal diameter increases, the risk of perforation also increases. In various series, colonic perforation has been reported in as many as 7% of all large bowel obstructions and 2% of obstructing colonic carcinomas. Perforations sometimes occur at the site of obstruction, but usually result from progressive ischemia in the dilated colon or cecum proximal to the obstruction.

An incompetent ileocecal valve allows gas to reflux into the small bowel, decompressing the colon, so the radiographic findings can mimic those of small bowel obstruction. Nevertheless, the distinction between colonic obstruction and small bowel obstruction has important implications because orally administered barium can inspissate above an unsuspected colonic obstruction. Abdominal CT or a single-contrast barium enema should therefore be considered in any patient with apparent obstruction of the distal small bowel on abdominal radiographs (especially an older patient who has no prior history of abdominal surgery) to rule out an underlying colonic or cecal carcinoma as the cause of obstruction.
Closed Loop Obstruction
A closed loop obstruction refers to a segment of bowel that is obstructed at two points. Closed loop obstructions usually involve the small bowel and are caused by adhesions, internal hernias, or volvulus. The findings on abdominal radiographs are often nonspecific. Occasionally, there may be a disproportionately dilated, gas-filled loop of small bowel that has the appearance of a coffee bean. Persistence of the dilated loop on sequential radiographs over several days should increase concern for a closed loop obstruction. Vascular compromise may lead to edema and thickening or effacement of the folds within this loop. If the obstructed segment fills with fluid, a rounded soft tissue density outlined by intra-abdominal fat produces a pseudotumor appearance. A history of intermittent, crampy abdominal pain replaced by steady, unrelenting pain should suggest a closed loop obstruction with vascular compromise. Nevertheless, a definitive diagnosis can be made only at surgery.
Volvulus
Any segment of intestine that has a mesenteric attachment has the potential to undergo a volvulus. Some patients may have intermittent intestinal twists associated with recurrent episodes of abdominal pain or emesis. If the twist is greater than 360 degrees, it is unlikely to resolve spontaneously. In some cases, air and intestinal contents may enter the twisted segment of bowel, producing abdominal distention and pain. The risk of vascular compromise in the twisted segment is more important than the mechanical effects of the volvulus. Severe vascular compromise may result in necrosis and perforation of bowel, causing sepsis and death. Gastric volvulus is discussed in Chapter 34 . Colonic volvulus may involve different segments of the colon, as discussed in the following sections.
Sigmoid Volvulus
Sigmoid volvulus constitutes 60% to 75% of all cases of colonic volvulus. Overall, sigmoid volvulus accounts for 1% to 2% of all intestinal obstructions in the United States. In some areas of South America and Africa, the incidence of sigmoid volvulus is extraordinarily high, reportedly because of a high-fiber diet and the resultant large, bulky stools, producing a chronically dilated, elongated sigmoid colon that predisposes patients to this type of volvulus. The incidence of sigmoid volvulus also appears to be higher in people living at higher altitudes in South America and Africa. In the United States, sigmoid volvulus tends to occur in older men and residents of nursing homes and mental hospitals, in whom chronic constipation and obtundation from medication are predisposing factors for gaseous distention of the sigmoid colon and stretching of the sigmoid mesocolon.
Patients with sigmoid volvulus typically present with abdominal pain and distention resulting from colonic obstruction. Obstipation and vomiting are also common findings. The symptoms are usually acute, but they may have a gradual onset in some patients.
Findings on abdominal radiographs are diagnostic of sigmoid volvulus in about 75% of patients with this condition. The classic radiographic appearance consists of a massively dilated loop of sigmoid colon that has an inverted U configuration and absent haustral folds and extends superiorly above the transverse colon into the left upper quadrant beneath the left hemidiaphragm (even elevating the diaphragm), with air-fluid levels in both the ascending and descending limbs of this loop. However, the dilated bowel can be in the midline or can even extend into the right upper quadrant ( Fig. 12-6 ). Although there often is associated dilation of the more proximal colon, disproportionate dilation of the sigmoid in relation to the remaining colon and extension of the sigmoid colon superiorly above the transverse colon are important diagnostic features for differentiating sigmoid volvulus from simple colonic obstruction. The apposed inner walls of the sigmoid colon may occasionally form a dense white line that points toward the pelvis. The absence of rectal gas is also an important differentiating feature. If prone or decubitus views of the pelvis show free passage of gas into the rectum, sigmoid volvulus therefore is extremely unlikely.

A contrast enema may occasionally be required in patients with suspected sigmoid volvulus. A low-pressure barium enema performed without inflation of a rectal balloon should demonstrate smooth, tapered narrowing, or beaking, at the rectosigmoid junction with associated obstruction.
Patients with sigmoid volvulus sometimes can be successfully treated by placement of a rectal tube for decompression of the dilated sigmoid loop. Patients who have persistent sigmoid dilation despite rectal tube placement and those who develop recurrent sigmoid volvulus may require surgical resection of the sigmoid colon for definitive treatment of this condition.
Cecal Volvulus
The term cecal volvulus refers to a condition caused by a rotational twist of the right colon on its long axis associated with mobility of the ascending colon, so the cecum flips into the midabdomen or left upper quadrant. Cecal volvulus can occur only when the right colon is incompletely fused to the posterior parietal peritoneum, an embryologic variant present in 10% to 37% of adults. These patients have a persistent mesentery on the ascending colon and, because of its greater mobility, the ascending colon can twist on its mesentery, producing a volvulus. Nevertheless, it should be recognized that the vast majority of patients with this embryologic variant never develop cecal volvulus. The term cecal volvulus is actually a misnomer because the twist is distal to the ileocecal valve. Cecal volvulus is less common than sigmoid volvulus, accounting for 2% to 3% of all colonic obstructions and about one third of all cases of colonic volvulus.
The characteristic findings of cecal volvulus, which are present on abdominal radiographs in about 75% of patients, consist of a markedly dilated, gas-filled cecum containing a single air-fluid level in an ectopic location ( Fig. 12-7 ), usually with the cecal apex in the left upper quadrant. The medially placed ileocecal valve may produce a soft tissue indentation, so the gas-filled cecum has the appearance of a coffee bean or kidney. Usually, little gas is seen distally in the colon. If the ileocecal valve is incompetent, refluxed gas in the small bowel may erroneously suggest a small bowel obstruction. The diagnosis may be confirmed by a contrast enema or abdominal CT scan showing the typical beaking at the point of the volvulus in the mid–ascending colon. Cecal volvulus may occur in a variety of settings, including colonoscopy, barium enema, obstructive lesions in the distal colon, and pregnancy.

In 1938, Weinstein described a condition known as cecal bascule, which involved folding of the right colon without twisting, so the cecum occupied a position in the midabdomen. The term bascule is derived from bascula, the Latin word for “scale.” The point at which the ascending colon is folded represents the fulcrum of the scale. This entity also requires a persistent mesentery on the ascending colon. The concept of a cecal bascule was challenged by Johnson and colleagues, who believed that these patients have a focal adynamic ileus of the cecum. Of their patients, 20% had cecal perforation. They emphasized that the duration of cecal distention was more important than cecal diameter in predicting impending perforation. Whether cecal bascule represents an actual anatomic folding of the right colon or an adynamic ileus is not as important as the recognition that a dilated, ectopically located cecum may be a source of abdominal symptoms and potential cecal perforation.
Cecal volvulus should be differentiated from a prolonged colonic ileus in bedridden patients with a persistent mesentery on the ascending colon because the anteriorly located cecum in these patients may become disproportionately dilated, mimicking the appearance of a cecal volvulus. This has been described as cecal pseudovolvulus. Unlike patients with true cecal volvulus, however, cecal pseudovolvulus is associated with diffuse colonic distention, so it is usually possible to differentiate these conditions on the basis of the radiographic findings.
Transverse Colon Volvulus
Volvulus of the transverse colon is an uncommon condition, accounting for only about 4% of all cases of colonic volvulus in the United States. As with sigmoid volvulus, elongation of the transverse mesocolon and close approximation of the hepatic and splenic flexures may allow the transverse colon to twist on its mesenteric attachment. Failure of normal fixation of the mesentery may lead to increased mobility of the ascending colon and hepatic flexure, predisposing these patients to volvulus of the transverse colon. Compression of the duodenojejunal junction at the root of the mesentery may cause severe vomiting. Mortality rates as high as 33% have been reported in these individuals.
Abdominal radiographs are usually not helpful for patients with volvulus of the transverse colon and may erroneously suggest sigmoid volvulus. A barium enema may confirm the diagnosis if it shows typical beaking and obstruction at the level of the transverse colon. Two separate air-fluid levels can sometimes be seen in the dilated transverse colon, a finding that helps differentiate volvulus of the transverse colon from cecal volvulus.
Splenic Flexure Volvulus
Splenic flexure volvulus is the least common type of colonic volvulus. Postoperative adhesions, chronic constipation, and congenital or postsurgical absence of the normal peritoneal attachments of the splenic flexure may predispose patients to this uncommon condition. Abdominal radiographs may reveal a dilated, featureless, air-filled loop of bowel in the left upper quadrant that is separate from the stomach, with air-fluid levels in the transverse colon and cecum. When a splenic flexure volvulus is suspected, a single-contrast barium enema may be performed for a more definitive diagnosis.
Appendicitis
The development of acute appendicitis requires obliteration of the appendiceal lumen, usually by a concretion that may be visible on abdominal radiographs. The concretion has been called a fecalith or coprolith, but the preferred term is appendicolith . This concretion forms around a nidus such as a piece of vegetable matter. Inspissated feces and calcium salts may adhere to the nidus, so it eventually reaches a size that occludes the appendiceal lumen. Accumulation of mucus proximal to the obstruction may distend the appendix, causing inflammation, ischemia, and perforation.
Some investigators believe that abdominal radiographs are of little value in patients with suspected appendicitis. Nevertheless, such radiographs are frequently obtained as the first imaging study in patients presenting to the emergency room with right lower quadrant pain.
Major Signs of Appendicitis
Signs of appendicitis on abdominal radiographs include the following:
Appendicolith.
The presence of an appendicolith is the single most helpful sign of appendicitis on abdominal radiographs. Appendicoliths are found in about 10% of patients with acute appendicitis, typically appearing as round or ovoid calcified densities that are frequently laminated ( Fig. 12-8 ). Most appendicoliths range from 1 to 2 cm in size, but some may be as large as 4 cm. They are usually in the right lower quadrant but can also be located in the pelvis or even in the right or left upper quadrant. The presence of an appendicolith has important implications for patients with appendicitis because it indicates a greater likelihood of superimposed perforation and abscess formation.

Abnormal Bowel Gas Pattern.
About 25% of patients with appendicitis have an abnormal bowel gas pattern, usually an adynamic ileus, but occasionally a partial or even complete small bowel obstruction may be present (see Fig. 12-8 ). An adynamic ileus occurs as a response to focal inflammation and may be localized to the right lower quadrant (also known as a sentinel ileus). Air-fluid levels in the jejunum have also been described in up to 50% of cases. A dilated transverse colon may also be seen as an early sign of appendiceal perforation. Mechanical obstruction may occur if the terminal ileum is compressed by the appendix or narrowed by adhesive bands.
Abnormal Cecum and Ascending Colon.
Localized inflammation and edema may cause thickening of the cecal wall and widening of haustral folds in this region. An air-fluid level may also be present in the cecum on upright or decubitus abdominal radiographs, but this finding is transient and nonspecific.
Extraluminal Soft Tissue Mass.
A soft tissue mass can be found in up to one third of patients with perforation. It may be caused by some combination of edema, fluid, and abscess formation in the right lower quadrant. The presence of mottled or loculated extraluminal gas within this soft tissue mass should strongly suggest an abscess.
Gas in the Appendix.
This sign has been described as one of acute appendicitis, even though the pathophysiology of the disease would more likely result in an absence of appendiceal gas. Usually, an air-filled appendix is a normal finding, simply reflecting the position of the appendix in relation to the cecum, because an ascending retrocecal appendix is more likely to contain gas.
Free Intraperitoneal Air.
A ruptured appendix rarely may lead to the development of a small amount of free intraperitoneal air. The obstructed appendiceal lumen prevents larger collections of gas from escaping into the peritoneal cavity, except in the case of a ruptured gas-containing abscess.
Obliteration of Normal Fat Planes.
Inflammation and edema may alter the water content of surrounding fat and obscure the normal fat planes of the psoas muscle, obturator muscle, or properitoneal flank stripe. This finding is nonspecific and is usually associated with other signs of appendicitis on abdominal radiographs.
Scoliosis of the Lumbar Spine.
Some patients with appendicitis may develop a lumbar scoliosis as a result of splinting. This finding is nonspecific, however, and can be related to patient positioning.
Surgeons have long believed that false-negative laparotomies are acceptable in some patients with right lower quadrant pain because of the serious, potentially life-threatening complications of untreated acute appendicitis. However, cross-sectional imaging studies such as CT and ultrasound have significantly improved the preoperative diagnosis of appendicitis (see Chapter 56 ).
Toxic Megacolon
Toxic megacolon, or toxic dilation of the colon, may be diagnosed on the basis of a dilated colon on abdominal radiographs in patients with fever, tachycardia, and hypotension. Toxic megacolon is traditionally associated with ulcerative colitis, but it can also occur in patients with granulomatous colitis, amebiasis, cholera, pseudomembranous colitis, cytomegalovirus colitis, and ischemic colitis. Toxic megacolon develops in 5% to 10% of patients with ulcerative colitis, but in only 2% to 4% of patients with granulomatous colitis. The duration of the underlying disease has no relationship to the development of toxic megacolon. In fact, 70% of patients with toxic megacolon develop this complication during their first episode of colitis.
When toxic megacolon is suspected on clinical grounds, it is important to assess not only the degree of colonic dilation on abdominal radiographs, but also the appearance of the colonic mucosa outlined by air and the presence or absence of free intraperitoneal air. In general, the transverse and ascending portions of the colon tend to become disproportionately dilated, but this is more a reflection of their anterior position within the abdomen or their underlying capacity to dilate than of a greater predisposition to disease. The upper limit of normal for the diameter of the transverse colon is about 6 cm, whereas the diameter of the transverse colon typically ranges from 6 to 15 cm in patients with toxic megacolon ( Fig. 12-9 ). A nodular mucosa may be visible in the dilated transverse colon as a result of inflammatory pseudopolyps in patients with ulcerative colitis (see Fig. 12-9 ).

Colonic perforation occurs in 30% to 50% of patients with toxic megacolon and is associated with a high mortality rate. Thus, a delayed diagnosis of toxic megacolon on abdominal radiographs may have disastrous consequences for these individuals. An increased amount of gas in the small bowel in patients with severe colitis has also been associated with an increased likelihood of developing this condition.
The diagnosis of toxic megacolon usually is made based on a combination of the clinical and plain film findings, so a contrast enema does not need to be performed in these patients. Although some patients with suspected toxic megacolon have undergone barium enemas, most authors believe that such examinations are contraindicated because of the risk of perforation. When toxic megacolon is suspected, CT may be performed to depict the underlying colitis and detect life-threatening complications such as colonic perforation.
Pneumoperitoneum
The presence of free intraperitoneal air (also known as pneumoperitoneum) is an important radiographic observation that usually indicates bowel perforation in patients with an acute abdomen. A classic experimental study by Miller and Nelson showed that as little as 1 mL of free air can be detected below the right hemidiaphragm on properly exposed upright chest radiographs. They emphasized the importance of placing the patient in the left lateral decubitus position for 15 to 20 minutes before obtaining a radiograph with the patient in an upright position to maximize the possibility of detecting small amounts of free air. Radiographs obtained in midinspiration or midexpiration are even more likely to reveal subtle findings of pneumoperitoneum. Chest radiographs obtained with the patient in an upright position are ideal for demonstrating free air because the x-ray beam strikes the diaphragms tangentially at their highest point. A posteroanterior view is usually obtained, but a lateral view of the chest may be even more sensitive. Although properly performed upright chest radiographs are extremely sensitive for detecting pneumoperitoneum, abdominal CT has been shown to be even more sensitive for detecting tiny amounts of free air in patients with acute trauma.
In contrast, upright abdominal radiographs result in an oblique view of the hemidiaphragms that may obscure free air because the x-ray beam is centered more inferiorly. Left lateral decubitus views of the abdomen are better for detecting small amounts of free air interposed between the free edge of the liver and lateral wall of the peritoneal cavity. Care should be taken to include the upper abdomen, because air rises to the highest point in the abdomen, which frequently is beneath the lower ribs. Radiographs obtained with the patient in the right lateral decubitus position can also be helpful, but gas in the stomach or colon may obscure small amounts of free air. A cross-table lateral view of the abdomen with the patient in a supine position may demonstrate free air in those who are physically unable to roll onto their sides. Not surprisingly, CT also is more sensitive in detecting free air than left lateral decubitus radiographs.
Upright or left lateral decubitus abdominal radiographs are based on the principle that air rises to the highest point in the peritoneal cavity. If, however, horizontal beam views cannot be obtained in patients who are too sick or debilitated to stand or lie on their side, the radiologist must be able to recognize indirect signs of free intraperitoneal air on supine abdominal radiographs. In one study, one or more signs of pneumoperitoneum were present on these radiographs in 59% of patients.
Major Signs of Free Air
Major signs of free air on supine abdominal radiographs include the following:
Rigler’s Sign.
Gas normally outlines only the luminal surface of the bowel. Gas on both sides of the bowel, however, may outline the bowel wall as a thin linear stripe ( Fig. 12-10A ). Since its original description by Rigler in 1941, this sign has been recognized as an important finding of pneumoperitoneum, but a moderate amount of free air must be present in the abdomen. Extraluminal air trapped between adjacent loops of bowel may also have a characteristic triangular appearance in patients with pneumoperitoneum ( Fig. 12-10B ). Overlapping loops of small bowel in the central abdomen can mimic Rigler’s sign, so it is helpful to evaluate the periphery of the radiograph. A pseudo-Rigler’s sign may also result from Mach bands, a phenomenon in which there is the perception of a line at the interface between two areas of differing density (e.g., gas and soft tissue). However, the perceived line has almost no discernable thickness, whereas the bowel wall has a measurable thickness of 1 mm or more in patients with a true Rigler’s sign. Still other patients may have a pseudo-Rigler’s sign caused by faint residual oral contrast material (usually from recent abdominal CT) coating the luminal surface of the bowel, so the increased density of the wall creates the erroneous impression that gas is present on both sides of the wall.

Increased Lucency in the Right Upper Quadrant.
Air accumulating superiorly in the free space between the anterior aspect of the liver and the abdominal wall may cause increased lucency in the right upper quadrant ( Fig. 12-11A ). Depending on the habitus of the patient, the lateral border of the air collection may be linear. Small collections of air may be seen as subtle rounded lucencies overlying the liver. Linear collections of gas may also be seen in the subhepatic space, although the latter finding must be differentiated from subhepatic fat.

Visualization of the Undersurface of the Diaphragm.
Air may be trapped anteriorly in the cupola of the diaphragm, permitting visualization of the undersurface of the central portion of the diaphragm or diaphragmatic muscle slips laterally. These findings depend on the amount of air present and on the orientation of the diaphragm.
Air in Morison’s Pouch (Posterior Hepatorenal Space).
Morison’s pouch is an intraperitoneal recess bounded anteriorly by the liver and posteriorly by the right kidney. In the supine position, fluid may gravitate to this space. Air escaping from a perforated viscus may become loculated in this space because of surrounding inflammation. Air in Morison’s pouch is characterized radiographically by a linear or triangular collection of gas in the medial aspect of the right upper quadrant outside the expected location of the bowel ( Fig. 12-11B ). The gallbladder may also be visualized.
Outline of the Normal Peritoneal Ligaments.
Larger amounts of free air may occasionally outline the falciform ligament ( Fig. 12-11C ) or extrahepatic segment of the ligamentum teres in the right upper quadrant, the lateral umbilical ligaments (inverted V sign) in the lower abdomen, and the urachus.
Football Sign.
Originally described by Miller in infants, this sign is caused by a large amount of free air filling the oval-shaped peritoneal cavity, resembling an American football. Occasionally, this sign may be seen in adults.
Air in the Lesser Sac of the Peritoneal Cavity.
Intraperitoneal air that traverses the foramen of Winslow may become trapped in the lesser sac. Such gas may be manifested by an ill-defined lucency above the lesser curvature of the stomach.
The presence of pneumoperitoneum does not always indicate an acute abdominal condition. Various causes of free air are listed in Table 12-1 .
| BOWEL |
|
| TRAUMA |
|
| FEMALE GENITAL TRACT |
|
Pneumoretroperitoneum
Gas that enters the retroperitoneal spaces (also known as pneumoretroperitoneum) can usually be distinguished from intraperitoneal gas. Because retroperitoneal gas is bound by fascial planes, it tends to collect in a linear fashion along the margins of the kidneys and psoas muscles and along the medial undersurface of the diaphragms ( Fig. 12-12 ). Meyers has described the various pathways in which retroperitoneal gas can travel. Perforation of the retroperitoneal portions of the intestines, such as the duodenum, ascending and descending colon, and rectum, usually accounts for this finding. In patients with sigmoid diverticulitis, gas can extend laterally along the left margin of the psoas muscle or, if the perforation involves the root of the sigmoid mesocolon, along both margins of the psoas muscle.

The location of retroperitoneal gas may provide a clue to its site of origin. Gas escaping from duodenal perforations tends to be confined to the right anterior pararenal space. Gas may also extend medially across the anterior aspect of the psoas muscle, sparing its lateral margin. Less commonly, gas may enter the perirenal space and outline the right kidney. Duodenal ulcers, iatrogenic duodenal injuries, and blunt abdominal trauma are all possible causes of perforation of the extraperitoneal portion of the duodenum.
Gas from a rectal perforation may be confined to the perirectal space or may extend into the anterior and posterior retroperitoneal spaces and even superiorly into the mediastinum. Iatrogenic trauma is a common cause of rectal perforation. Radiologists should always be aware of the potential risk of rectal perforation when insufflating a balloon during barium enemas.
Pneumobilia
Gas in the bile ducts, or pneumobilia , is characterized radiographically by thin, branching, tubular areas of lucency in the central portion of the liver ( Fig. 12-13 ). This central location is explained by the flow of bile from the periphery of the liver toward the porta hepatis.

Pneumobilia almost always results from some type of communication between the bile ducts and intestine. One of the most common causes is a surgically created biliary enteric fistula such as a choledochojejunostomy or cholecystojejunostomy (see Fig. 12-13 ). The most common nonsurgical cause of a choledochoduodenal fistula is a penetrating duodenal ulcer, and the most common nonsurgical cause of a cholecystoduodenal fistula is a gallstone eroding into the duodenum. In some patients with a cholecystoduodenal fistula, a patent cystic duct may allow air to enter the intrahepatic bile ducts. If the ectopic gallstone is 2.5 cm or larger in diameter, it may obstruct the small bowel, usually at or near the ileocecal valve, and produce a so-called gallstone ileus; this is actually a misnomer because these patients have mechanical small bowel obstruction caused by a gallstone impacted in the distal ileum. The classic triad (also known as Rigler’s triad) of air in the biliary tree, small bowel obstruction, and an ectopic calcified gallstone is almost diagnostic of gallstone ileus on abdominal radiographs. An incompetent sphincter of Oddi, recent sphincterotomy or sphincteroplasty, anomalous insertions of the biliary tree, recent passage of a common duct stone, and infestation of the biliary tract by Ascaris are other causes of pneumobilia.
The radiographic appearance of pneumobilia is sufficiently characteristic to allow a confident diagnosis on the basis of the findings on abdominal radiographs. Occasionally, periportal fat or fat around the ligamentum teres hepatis may be manifested by a faint lucency over the liver, but its appearance is different from that of pneumobilia. The most important consideration in the differential diagnosis of pneumobilia is the presence of gas in the portal venous system (see later, “ Portal Venous Gas ”).
Portal Venous Gas
Portal venous gas was originally described in adults by Susman and Senturia in 1960. This ominous radiographic finding is manifested by thin, branching, tubular areas of lucency that occupy the periphery of the liver and extend almost to the liver surface ( Fig. 12-14 ). The peripheral location of the gas reflects the hepatopetal flow of blood in the portal venous system away from the porta hepatis. In advanced cases, air can be seen outlining the more centrally located main portal vein, but this finding is less common. A left lateral decubitus radiograph of the abdomen may facilitate visualization of portal venous gas. Unless the gas has been introduced iatrogenically by vascular catheterization, endoscopic manipulation, or other iatrogenic causes, the source of the gas is almost invariably the intestine. Intraluminal intestinal air can breach a damaged mucosa, enter the bloodstream, and eventually reach the portal venous system of the liver.

The most important cause of portal venous gas is intestinal ischemia or infarction. In adults with ischemic bowel disease, death often occurs shortly after portal venous gas has been observed. The finding of portal venous gas should therefore lead to a careful search for gas in the wall of the bowel caused by intestinal infarction (see later, “ Intramural Gas ”).
Portal venous gas may occasionally have benign causes. Dilation of the stomach and small bowel may allow air to enter the intestinal mucosa, eventually reaching the liver. Nonfatal cases of portal venous gas have also been described in patients with diverticulitis and inflammatory bowel disease and in patients who have undergone a double-contrast barium enema or colonoscopy for inflammatory bowel disease. Traumatic injury to the common bile duct as a complication of endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy has also been reported as a benign cause of portal venous gas. Portal venous gas has even been described as a transient finding on Doppler ultrasound during the early postoperative period after liver transplantation.
Hepatic Arterial Gas
Gas in the hepatic artery has been reported anecdotally in a patient in whom the hepatic artery was ligated for the treatment of an unresectable hepatic adenoma. The smaller caliber of the hepatic artery and relative paucity of intrahepatic branches should differentiate this finding from portal venous gas. Hepatic arterial gas may be reported more frequently as the use of aggressive interventional radiographic techniques increases for the treatment of hepatic neoplasms.
Intramural Gas (Pneumatosis)
Gastric emphysema is a relatively benign form of pneumatosis usually resulting from iatrogenic injury to the mucosa at endoscopy or increased intraluminal pressure in the stomach associated with gastric outlet obstruction. This condition is characterized by linear collections of gas in the wall or stomach. In contrast, emphysematous gastritis is a rare fulminant variant of phlegmonous gastritis; hemolytic Streptococcus is the most commonly implicated organism. Underlying causes of this life-threatening condition include ingestion of caustic substances, severe gastroenteritis, and gastroduodenal surgery that compromises the vascular supply of the stomach. Emphysematous gastritis is characterized by cystic, bubbly collections of gas in the gastric wall that have a very different appearance than that of the linear intramural collections seen in gastric emphysema.
Gas in the wall of the small bowel, which is termed pneumatosis intestinalis, is characterized by two radiographic patterns—a bubbly appearance or thin, linear streaks of gas. The bubbly appearance of intramural gas is easily mimicked by fecal material within the colon. In patients with this form of pneumatosis, close inspection may reveal small bubbles of gas outside the confines of the bowel, leading to the correct diagnosis. In contrast, linear gas collections tend to be more readily apparent and should always be considered an important finding on abdominal radiographs, regardless of their location ( Fig. 12-15 ). In combination with portal venous gas (see earlier, “ Portal Venous Gas ”), linear gas collections in the intestinal wall are almost always a sign of bowel infarction in adult patients. Other findings of bowel ischemia or infarction on abdominal radiographs include dilation of bowel and nodular thickening or thumbprinting of the bowel wall. CT may also reveal characteristic findings in patients with bowel ischemia or infarction. Pneumatosis is particularly well shown by CT, but does not always indicate infarction of the bowel unless the pneumatosis is associated with portomesenteric venous gas. The linear pattern of pneumatosis identified on CT is more likely to be associated with transmural bowel infarction than the bubbly pattern.