Gastrointestinal, Liver–Spleen, and Hepatobiliary Scintigraphy
David K. Shelton
Roshanak Rahnamayi
Gastrointestinal Studies
Nuclear medicine imaging studies can provide considerable information in the functional evaluation of the gastrointestinal (GI) system. Routine studies include hepatobiliary, GI-bleeding studies, and gastric-emptying measurements. Other procedures that are less frequently ordered provide clinically valuable information.
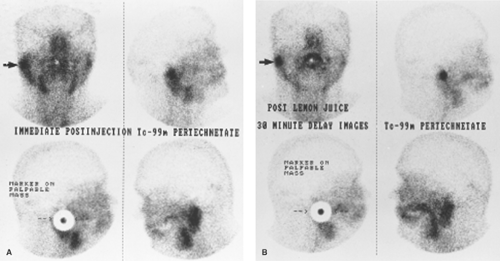
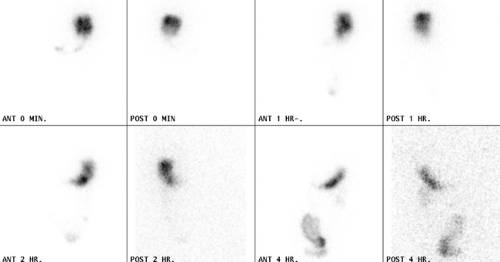
Salivary Scanning
A quick look at the salivary glands of the mouth is frequently had in conjunction with the Tc-99m pertechnetate (Tc-99m-O4) scan of the thyroid gland. The salivary glands can be scanned intentionally with Tc-99m-O4. A 5- to 10-mCi dose is injected intravenously (IV) with planar images performed immediately and after a delay during which lemon juice is washed around the mouth. In the past, this study has been used to grade the severity of Sjogren syndrome as inflammation degrades the secretory function of the glands. The salivary scan can demonstrate salivary obstruction and can be used as an adjunct to or replacement for sialography. Stimulation of the glands with lemon juice is important to document the drainage of saliva through the duct system to the mouth (Fig. 58.1). A salivagram can also be accomplished by swabbing a child’s mouth with radiotracer. Delayed images of the lungs evaluate for aspiration in children suspected of swallowing disorders.
Esophageal Imaging
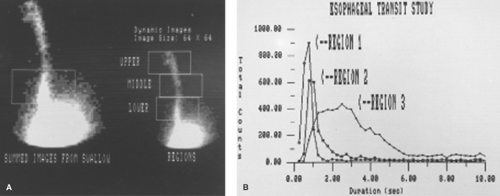
The esophageal transit study, performed with swallowed solutions or with solid boluses labeled with Tc-99m-sulfur colloid, is an examination which can be done in lieu of esophageal manometry. It has been reported to detect esophageal dysmotility in 50% of symptomatic patients with an otherwise normal evaluation for dysphagia.
In the supine or upright position with a gamma-camera imaging in the anterior projection, the patient swallows a radiolabeled bolus while dynamic data are obtained via computer. The esophagus is divided into three regions of interest (ROI): upper, middle, and lower. Transit times are then calculated from time–activity curves representing the ROIs. The normal esophagus demonstrates sequential activity from proximal to distal with no visualized esophageal activity remaining after 10 seconds. Regional analysis may differentiate between achalasia and scleroderma. It is important to remember that esophageal scintigraphy is functional and does not provide detailed anatomic information. Barium or endoscopic study is necessary to exclude the possibility of neoplasm or infection as the cause of impaired esophageal function (Fig. 58.2).
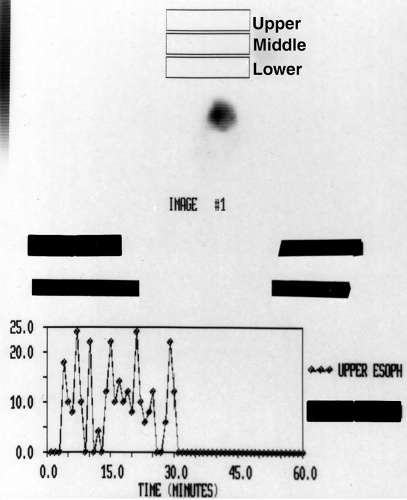
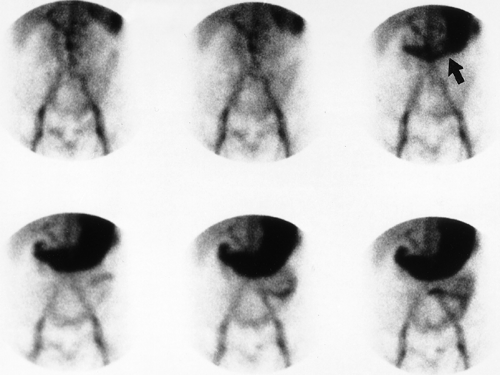
Gastroesophageal Reflux
The evaluation of heartburn and atypical chest pain in the adult commonly raises the clinical question of gastroesophageal reflux (GER) disease. In the pediatric population, failure to thrive and recurrent pneumonia often elicit the same question. A common diagnostic tool currently used in the diagnosis of GER disease is acid reflux monitoring. This examination unfortunately requires nasoesophageal intubation and 24-hour continuous recording. It is invasive and unwieldy, especially in the pediatric age group.
GER scintigraphy is performed with acidified orange juice mixed with Tc-99m-sulfur colloid. The acid decreases the lower esophageal sphincter pressure and also delays gastric emptying. Regions of interest are established via computer to correspond to the stomach and the segments (upper, middle, and lower) of the esophagus. In the pediatric population, ROIs over the lungs detect aspiration by the end of the study or on delayed imaging 1 to 3 hours later. Images may be recorded in adults with an abdominal binder that increases abdominal pressure sequentially in 10-mm Hg increments to a maximum of 100 mm Hg. Normal patients have no detectable GER
activity. This examination is reported to have 90% sensitivity in the detection of GER (Fig. 58.3).
activity. This examination is reported to have 90% sensitivity in the detection of GER (Fig. 58.3).
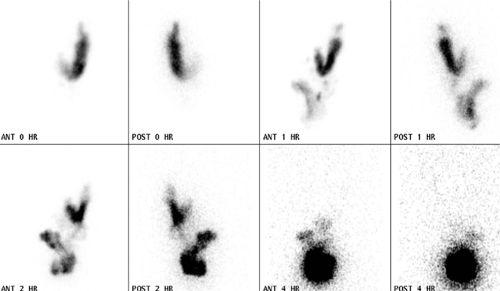
Gastric Emptying
Gastric emptying is a complex physiologic process directed not only by neuroendocrine processes but also by a host of local factors. Food type, pH, and fatty content as well as food osmolality affect the rate of gastric emptying. Impaired gastric emptying can be caused by many diseased states such as diabetes mellitus, electrolyte disturbances, postvagotomy syndromes, and some medications.
Excluding mechanical obstruction is important in diagnosing the cause of the patient’s symptoms. Endoscopy or barium studies are superior in the detection of gastric ulcers, tumors, or bezoars. Gastric-emptying scintigraphy has become the gold standard in the clinical evaluation of gastric motility. It is a simple test to perform, though interpretation is based upon complicated mathematical models. Solid food, liquids, or both
are labeled with a radiotracer and consumed by the patient. Digital images of the stomach are acquired and a time–activity curve is generated for the graphic analysis of the rate of emptying (Fig. 58.4).
are labeled with a radiotracer and consumed by the patient. Digital images of the stomach are acquired and a time–activity curve is generated for the graphic analysis of the rate of emptying (Fig. 58.4).
The normal half-emptying time (T1/2) of radioactive solids and liquids varies with the technique employed. In general, the normal T1/2 is less than 90 minutes for solids and less than 60 minutes for liquids. Each laboratory should establish its own normal T1/2 values. Liquid gastric emptying usually follows an exponential curve, whereas solid emptying is biphasic with an initial lag phase followed by a linear curve. To evaluate gastric emptying, gastric-emptying scintigraphy can be performed with liquid, solid, or both (by using two different radiopharmaceuticals and a dual-energy camera). However, the medical literature states that solid gastric-emptying studies are more sensitive for the detection of gastroparesis than are liquid studies. Visual interpretation of the stomach images is invaluable in understanding the “number” generated for T1/2.
A standard protocol for gastric-emptying scintigraphy is to calculate gastric-emptying rate at 2 and 4 hours after the consumption of a mixture of an egg white meal with 1-mCi Tc-99m-sulfur colloid. A gastric-emptying rate of less than 40% at 2 hours and less than 90% at 4 hours is consistent with gastroparesis (Fig. 58.5).
The gastric-emptying technique can be extended using bowel transit times to evaluate and to time the transit between stomach and colon, colonic transit, and to characterize the disorders of the bowel’s smooth muscle or enteric nervous system.
C-14 Urea Breath Test
The C-14 urea breath test (UBT) is an inexpensive, accurate, noninvasive test for active infection with Helicobacter pylori (H. pylori). H. pylori is a gram-negative, spiral-shaped bacterium that is found in the gastric mucosa or is adherent to the epithelial lining of the stomach. H. pylori is known to cause
more than 90% of duodenal ulcers and up to 80% of gastric ulcers. It has also been associated with an increased incidence of gastric carcinoma and gastric lymphoma. For the UBT, a patient needs to be fasting and off antibiotics, bismuth, and proton-pump inhibitors. A 1-mCi capsule of C-14-labeled urea is administered by mouth and then 10 minutes later a breath sample is collected. H. pylori contains an enzyme, urease, which hydrolyzes the urea into ammonia and C-14-labeled CO2 that is subsequently detected in the breath sample using liquid scintillation techniques. This can be accomplished locally or the sample can be sent into a central laboratory. The UBT has a sensitivity and specificity of 94% to 98%. Alternative tests include endoscopic biopsy to identify the bacterium or serology titers, which will remain positive even after treatment.
more than 90% of duodenal ulcers and up to 80% of gastric ulcers. It has also been associated with an increased incidence of gastric carcinoma and gastric lymphoma. For the UBT, a patient needs to be fasting and off antibiotics, bismuth, and proton-pump inhibitors. A 1-mCi capsule of C-14-labeled urea is administered by mouth and then 10 minutes later a breath sample is collected. H. pylori contains an enzyme, urease, which hydrolyzes the urea into ammonia and C-14-labeled CO2 that is subsequently detected in the breath sample using liquid scintillation techniques. This can be accomplished locally or the sample can be sent into a central laboratory. The UBT has a sensitivity and specificity of 94% to 98%. Alternative tests include endoscopic biopsy to identify the bacterium or serology titers, which will remain positive even after treatment.
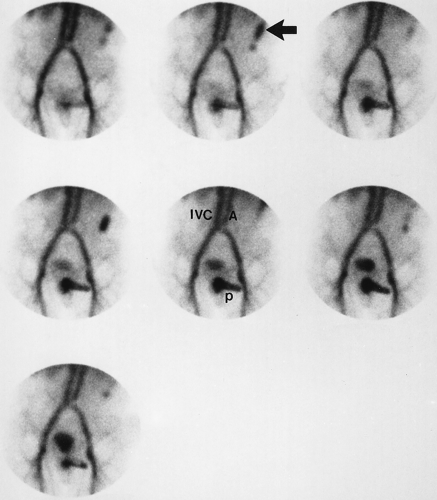
Gastrointestinal Bleeding Scintigraphy
Patients who present with clinically suspected upper GI bleeding are usually evaluated and often treated by endoscopy. Scintigraphy is not usually needed. The patient with suspected lower GI bleeding presents different problems in diagnosis and therapy. Proctosigmoidoscopy can exclude hemorrhoidal bleeding and colonoscopy may identify the cause. An emergent GI bleeding study with in vitro Tc-99m-tagged red blood cells is very sensitive and can locate the bleeding site. Continuous 1-minute dynamic frames are acquired over the abdomen and pelvis in the anterior projection for at least 90 minutes or until the patient has bled enough to locate the source of hemorrhage. This technique can detect bleeding rates as low as 0.1 ml/min versus contrast angiography, which detects 1 ml/min of GI bleeding. The study should be done emergently during the clinical period of suspected active bleeding. Repeated imaging can be done at any time up to 24 hours after red cell labeling but care should be taken because blood may have moved into the colon.
Accurate hemorrhage localization is required for the resection of a bleeding site. If angiographic therapy for a bleeding site is proposed, the more sensitive GI-bleeding study should be done first. The GI-bleeding study will guide the selection of appropriate vessels for embolization or infusion of vasoreactive drugs. Positive GI-bleeding studies demonstrate three cardinal findings: (1) an abnormal hot spot of radiotracer activity appears “out of nowhere” as it enters the bowel lumen; (2) this activity persists and may increase with time; and (3) the activity moves with peristalsis antegrade, retrograde, or in both directions (Figs. 58.6 to 58.8). To interpret the images, one should be aware of false positives such as bladder or genital activity which can be identified by obtaining postvoid and lateral pelvic views.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree