Gas content within the bowel lumen makes the visibility difficult (Table 41.1).
High-frequency linear probe is used.
For identification
Stomach—Gastric rugae
Jejunum—Valvulae conniventes
Large bowel—Haustra
Normal gut is compressible by probe. Abnormally thickened gut is noncompressible.
Graded compression is used in acute appendicitis. Slow-graded compression moves the bowel loops out of the way without any discomfort to the patient.
1. Free intraperitoneal gas—Difficult to detect on USG
• Echogenic peritoneal stripe
• Air (ring down artifacts) b/w the abdominal wall and the liver
2. Loculated fluid collection—Aperistaltic collection with varying echogenicity
Table 41.1 Illustrating five layers of gut wall (Gut signature)
Mucosa (innermost) | Hyperechoic |
Muscularis mucosa | Hypoechoic |
Submucosa | Hyperechoic |
Muscularis propria | Hypoechoic |
Serosa/adventitia | Hyperechoic |
3. Mesenteric lymphadenopathy—Focal discrete hypoechoic masses of varying size. Loss of echogenic hilum
4. Edematous bowel loops
5. Wall thickening—Normal gut wall—3 millimeters if distended and 5 millimeters if collapsed
6. Loss of normal gut signature
Usually benign lesions involve long segment with concentric thickening and wall layer preservation.
Malignant lesions involve short segment with eccentric disease and wall layer destruction.
Normal appendix is compressible with <3 millimeters wall thickness. Graded compression technique (Puylaert) is required.
Presentation—RLQ pain, high WBC count
USG findings
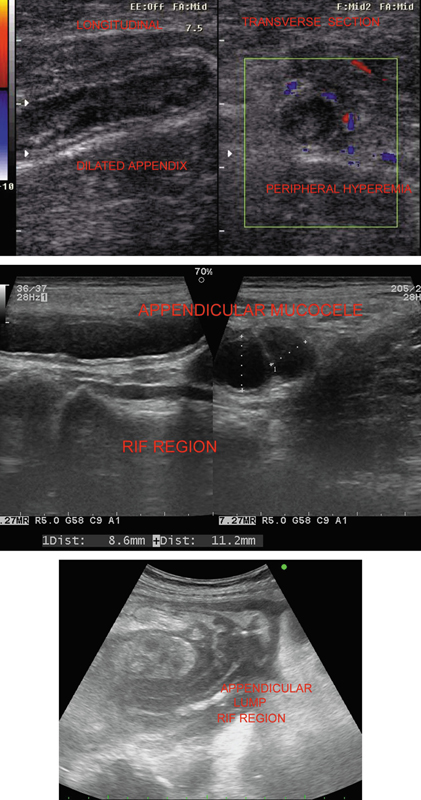
• Blind ended, noncompressible, and aperistaltic tube with diameter >6 millimeters arising from the base of cecum
• Inflamed perienteric fat
• Pericecal collections
• Appendicolith
• Hyperemia of wall
Appendiceal perforation may occur leading to loculated pericecal collection, loss of wall layers (Figure 41.1).
Figure 41.1 Varying presentations of appendicular lesions—appendicitis, mucocele, and appendicular lump.
Mucocele of appendix—Large hypoechoic well-defined RLQ cystic lesion with variable internal echoes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree