and Robert W. Henderson1
(1)
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Case 16.1: Sarcoidosis
History
50-year-old male, with history of esophageal cancer, status post esophagectomy with gastric pull-through.
Findings
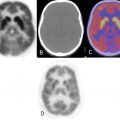
Symmetrically intense FDG activity seen within bihilar and mediastinal lymph nodes, demonstrating hypermetabolism of similar intensity (Figs. 16.1 and 16.2).



Fig. 16.1

Fig. 16.2
Impression
Findings compatible with sarcoidosis by scan pattern (which was proven on surgery, during esophagectomy and gastric pull-up).
Pearls and Pitfalls
The hypermetabolic lymph nodes could have been mistaken for metastatic disease.
Discussion
Etiology for granulomatous disease (noncaseating) is unknown.
Characteristic scan pattern: nodal disease involving mediastinal (lower paratracheal, aortopulmonary window, subcarinal), bilateral hilar, and interlobar lymph nodes.
Parenchymal disease is a late feature; by then nodal disease may have regressed.
18FDG-PET scan pattern is similar to 67Ga scan (lambda pattern) in the region of the chest.
Case 16.2: Pneumoconiosis
History
55-year-old male, sand blaster by occupation, presents with chronic cough.
Findings
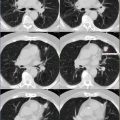
Lambda pattern of lymphadenopathy involving mediastinal and bihilar nodal regions (Fig. 16.3, yellow arrow). Particles predominantly seen in the upper lobes of the lung, as shown here in the right upper lobe image (Fig. 16.4, red arrow).



Fig. 16.3

Fig. 16.4
Impression
Silicosis based on correlation with patient’s occupational exposure history, presence of hypermetabolic mediastinal and bihilar lymph nodes (lambda pattern), and visualization of multiple small pulmonary nodules, predominantly in the upper lobes.
Discussion
Involvement of upper lobes predominantly. This is related to lymphatic drainage, which is better in the lower chest, as it is assisted by more excursion.
Particles that pass the respiratory bronchioles into the alveoli are drained by lymphatics, due to lack of cilia.
Case 16.3: Asbestosis
History
55-year-old male with asbestosis.
Findings
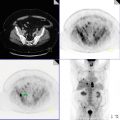
Fibrotic changes in the lower lung fields demonstrating low-grade FDG activity on PET and PET/CT fused images (Fig. 16.5). Pleural plaque in the left lower lobe (red arrow).


Fig. 16.5
Impression
Sequela to prior asbestosis exposure.
Discussion
Differentiating idiopathic pulmonary fibrosis from asbestosis is important because of legal and compensatory issues (Fig. 16.5).
Case 16.4: Prior Tuberculosis /Old Granulomatous Disease
History
Patient with known history of prior tuberculosis (TB).
Findings
Impression
Granulomatous disease by scan pattern.
Pearls and Pitfalls
Granulomatous disease (GD) is by far the commonest false-positive finding for nodal disease in the chest. In majority of the time, the hilar and med iastinal lymph nodes cannot be readily biopsied. Therefore, the classic scan pattern for GD must be identified on PET/CT.
Discussion
Active nodes common.
Does not imply active infection or need for treatment.
May or may not be associated with calcifications.
Nodes usually are normal size.
Usually bilateral (Fig. 16.6).
Case 16.5: Granulomatous Disease in the Midst of Hodgkin’s Lymphoma
History
56-year-old male, with history of Hodgkin’s disease (HD) below the diaphragm and prior history of tuberculosis. PET/CT images during chemotherapy (Fig. 16.7, top images); post chemotherapy PET/CT (Fig. 16.7, bottom images).