• Evaluation of a pelvic mass, uterine enlargement, endometrial abnormalities, ovarian masses or acute pelvic pain • Uterus: a triangular or ovoid soft tissue structure located behind the urinary bladder • Cervix: a rounded structure inferior to the uterine corpus • Vagina: a flat rectangular structure at the level of the fornix • Broad and round ligaments: these are seen coursing laterally and anteriorly (respectively) • Ovaries: these are posterolateral to the uterine corpus The zonal anatomy is demonstrated as follows: • Ovaries: The follicles demonstrate higher SI than the surrounding stroma • Cervical canal: 3–4cm long and ⅓ the length of the uterus (it shortens after childbirth) • Cavity of uterine body: this is triangular in shape • Fallopian tubes: these are 5–6cm long • Embryology: the uterus, upper ⅔ of the vagina and Fallopian tubes are derived from the paired Müllerian ducts • Due to non-development or rudimentary development of one Müllerian duct • T2WI: a ‘banana-like configuration’ of the normal duct: there is a curved, elongated uterus with tapering of the fundal segment off the midline • Due to non-fusion of the two Müllerian ducts • T2WI: there are two widely separate normally sized uterine horns with two cervices • T1WI: haemorrhage may be seen if there is a transverse septa causing obstruction • Due to partial fusion of the Müllerian ducts (with incomplete fusion of the cephalad extent of the uterovaginal horns with resorption of the uterovaginal septum) • The uterine horns are separated by an intervening cleft (> 1cm) within the external fundal myometrium • T2WI (parallel to uterine long axis): there is a convex, flat or concave (< 1cm) external uterine contour (+ fibrous septa) • A transverse vaginal septum prevents loss of menstrual blood and results in haematocolpos • T2WI: a dilated vagina with intraluminal fluid of intermediate or high SI (± fluid and debris levels) • T1WI (+ fat suppression): this confirms the presence of any blood products which appear of high SI • A benign tumour arising from uterine smooth muscle cells (± varying amounts of fibrous tissue) • It is the most common uterine tumour (seen in up to 40% of premenopausal women) • Menorrhagia (if there is a submucosal location) • Depending on the proportion of smooth muscle, fibrosis and degeneration, appearances can range from hypoechoic to echogenic, and homogeneous to heterogeneous • Submucosal leiomyomas may mimic endometrial lesions on US – US HSG may aid in the diagnosis • T1WI: well-circumscribed, rounded lesions with intermediate SI • T1WI (FS): this can demonstrate haemorrhagic degeneration (with high SI) • T1WI + Gad: the enhancement is less than that of the adjacent myometrium • T2WI: there is lower SI relative to the myometrium or endometrium • An enlarged globular uterus, often with antero-posterior asymmetry
Gynaecology
IMAGING TECHNIQUES IN GYNAECOLOGY
ULTRASOUND (US)
Indications
 it allows transabdominal and transvaginal guidance of fluid or tissue sampling
it allows transabdominal and transvaginal guidance of fluid or tissue sampling  it allows transvaginal-guided drain placement and guidance for placement of brachytherapy for cervical and endometrial malignancy
it allows transvaginal-guided drain placement and guidance for placement of brachytherapy for cervical and endometrial malignancy  it allows intraoperative assessment for the completion of evacuation of products of conception
it allows intraoperative assessment for the completion of evacuation of products of conception
Normal US anatomy
 Endometrium: proliferative phase: ≤ 8mm
Endometrium: proliferative phase: ≤ 8mm  midcycle: a trilaminar appearance measuring up to 12–16mm
midcycle: a trilaminar appearance measuring up to 12–16mm  secretory phase: hyperechoic due to the increasing glandular complexity
secretory phase: hyperechoic due to the increasing glandular complexity  ≤ 16mm
≤ 16mm
 Ovaries: these are anterior to the iliac vessels
Ovaries: these are anterior to the iliac vessels  they typically measure 30mm in any two dimensions but may measure ≥ 50mm in one plane
they typically measure 30mm in any two dimensions but may measure ≥ 50mm in one plane  the ovarian volume is usually < 10cm3
the ovarian volume is usually < 10cm3
Computed tomography (CT)
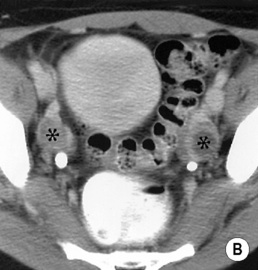
Normal CT anatomy
 the myometrium enhances with contrast (helping to delineate the endometrium, which is of lower attenuation)
the myometrium enhances with contrast (helping to delineate the endometrium, which is of lower attenuation)
 they are of soft tissue density with small cystic regions
they are of soft tissue density with small cystic regions  they are atrophic in postmenopausal women
they are atrophic in postmenopausal women
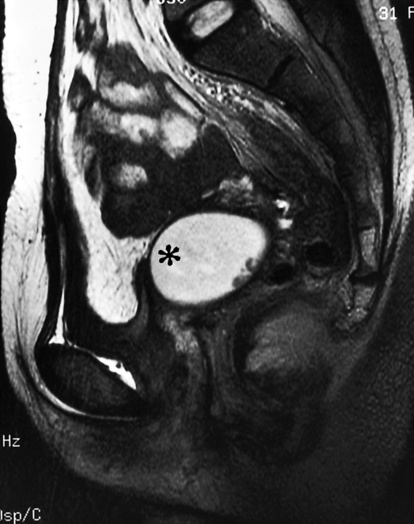
MAGNETIC RESONANCE IMAGING (MRI)
T2WI
 Endometrium: this is of high SI
Endometrium: this is of high SI  ≤ 8mm (proliferative phase)
≤ 8mm (proliferative phase)  ≤ 16mm (secretory phase)
≤ 16mm (secretory phase)  < 5mm (postmenopausal women that are not receiving hormonal therapy)
< 5mm (postmenopausal women that are not receiving hormonal therapy)
 Junctional zone (representing the innermost myometrium): this is of low SI (due to its low water content)
Junctional zone (representing the innermost myometrium): this is of low SI (due to its low water content)
 Peripheral myometrium: this is of intermediate SI (and higher than striated muscle)
Peripheral myometrium: this is of intermediate SI (and higher than striated muscle)
 Endocervical glands and mucus: central high SI
Endocervical glands and mucus: central high SI
 Stroma: low SI (as it is composed of elastic fibrous tissue)
Stroma: low SI (as it is composed of elastic fibrous tissue)
 Periphery of cervix: intermediate SI similar to myometrium (as it is composed of smooth muscle)
Periphery of cervix: intermediate SI similar to myometrium (as it is composed of smooth muscle)
OTHER IMAGING TECHNIQUES
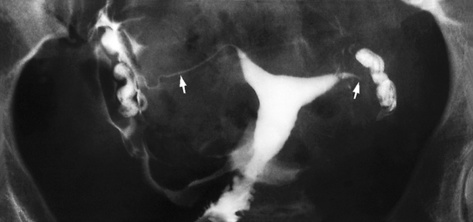
Hysterosalpingography (HSG)
 it is often spindle shaped and there may be glandular filling
it is often spindle shaped and there may be glandular filling
 the average length and intercornual diameter is approximately 35mm
the average length and intercornual diameter is approximately 35mm
 the isthmus is of uniform diameter and opens laterally into a wide ampulla
the isthmus is of uniform diameter and opens laterally into a wide ampulla
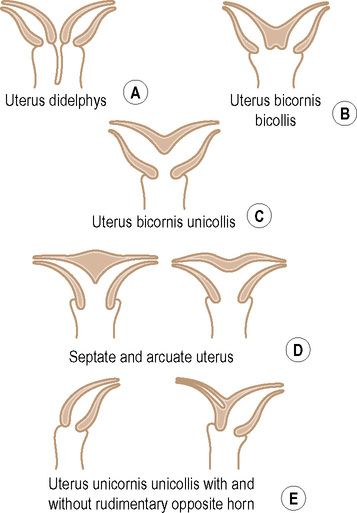
CONGENITAL ANOMALIES OF THE FEMALE GENITAL TRACT
CONGENITAL ANOMALIES OF THE FEMALE GENITAL TRACT
DEFINITION
 at approximately 10 weeks following conception the ducts migrate caudally and undergo fusion and subsequent canalization
at approximately 10 weeks following conception the ducts migrate caudally and undergo fusion and subsequent canalization  congenital anomalies arise when this process is interrupted:
congenital anomalies arise when this process is interrupted:
RADIOLOGICAL FEATURES (MRI)
Uterine anomalies
Class II: unicornuate uterus
 the remaining Müllerian duct is fully developed
the remaining Müllerian duct is fully developed
 the normal uterine zonal anatomy is maintained
the normal uterine zonal anatomy is maintained  the rudimentary horn demonstrates lower SI
the rudimentary horn demonstrates lower SI
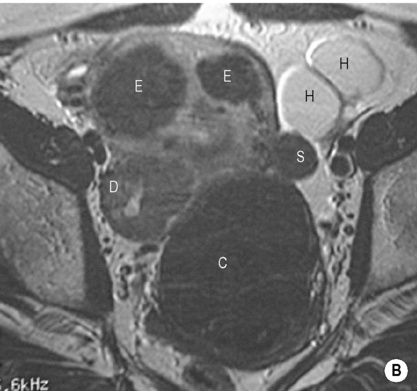
Class III: uterus didelphys
 the endometrial and myometrial widths are preserved
the endometrial and myometrial widths are preserved  a vaginal septum is seen in 75% of cases
a vaginal septum is seen in 75% of cases
Class IV: bicornuate uterus
 a normal zonal anatomy is seen within each horn and there is a dividing septum composed of central myometrium
a normal zonal anatomy is seen within each horn and there is a dividing septum composed of central myometrium
Class V: septate uterus
 Due to incomplete resorption of the final fibrous septum between the two uterine horns
Due to incomplete resorption of the final fibrous septum between the two uterine horns
 The septum may be partial, or it may be complete and extend to the external cervical os
The septum may be partial, or it may be complete and extend to the external cervical os
Vaginal anomalies
Disorder of vertical fusion
 the lower ⅓ of the vagina is replaced by low SI fibrous tissue with loss of the normal zonal anatomy
the lower ⅓ of the vagina is replaced by low SI fibrous tissue with loss of the normal zonal anatomy
BENIGN UTERINE CONDITIONS
LEIOMYOMA (FIBROID)
DEFINITION
 it is oestrogen dependent, and therefore regresses after the menopause
it is oestrogen dependent, and therefore regresses after the menopause
 they are usually multiple
they are usually multiple
CLINICAL PRESENTATION
 dysmenorrhoea
dysmenorrhoea  subfertility (due to narrowed Fallopian tube or interference with implantation)
subfertility (due to narrowed Fallopian tube or interference with implantation)  urinary frequency
urinary frequency
 Red degeneration: this follows acute impairment of the blood supply (often during pregnancy), and presents with acute abdominal pain and tenderness
Red degeneration: this follows acute impairment of the blood supply (often during pregnancy), and presents with acute abdominal pain and tenderness
 Hyaline degeneration: there is gradual impairment of the blood supply, and it is asymptomatic
Hyaline degeneration: there is gradual impairment of the blood supply, and it is asymptomatic
 Obstetric complications: malposition
Obstetric complications: malposition  a retained placenta
a retained placenta  interference with vaginal delivery
interference with vaginal delivery  premature uterine contractions
premature uterine contractions
RADIOLOGICAL FEATURES
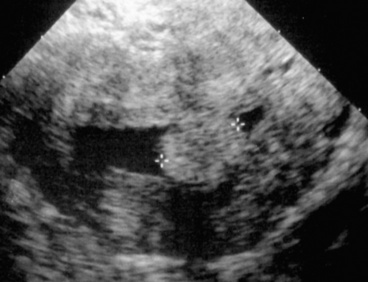
US
 there can be acoustic shadowing or shadowing echogenic foci due to the presence of calcification
there can be acoustic shadowing or shadowing echogenic foci due to the presence of calcification
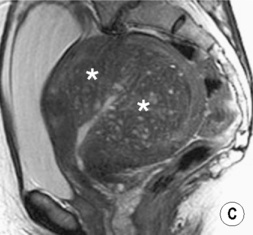
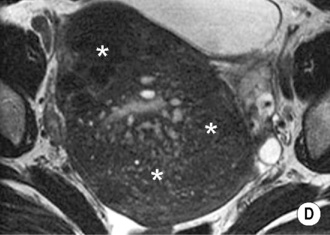
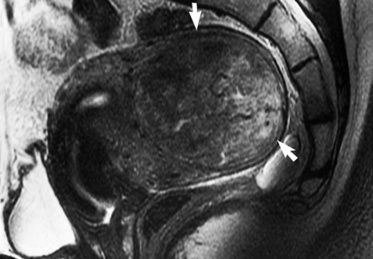
MRI
 any degenerated areas may not enhance
any degenerated areas may not enhance
 signal voids represent calcification or vessels
signal voids represent calcification or vessels
ADENOMYOSIS
Radiological features
 myometrial heterogeneity (due to the endometrial implants and intervening smooth muscle hypertrophy)
myometrial heterogeneity (due to the endometrial implants and intervening smooth muscle hypertrophy)  endometrial implants can present as diffuse echogenic nodules, subendometrial echogenic linear striations, or 2–6mm subendometrial cysts (representing haemorrhage within an implant)
endometrial implants can present as diffuse echogenic nodules, subendometrial echogenic linear striations, or 2–6mm subendometrial cysts (representing haemorrhage within an implant)
MRI
Radiology Key
Fastest Radiology Insight Engine


 a 3.5–5MHz transducer is used
a 3.5–5MHz transducer is used
 a 5–8MHz transducer is used
a 5–8MHz transducer is used  it allows closer apposition to the pelvic organs
it allows closer apposition to the pelvic organs


 the detection of persistent and recurrent pelvic tumour
the detection of persistent and recurrent pelvic tumour  for biopsy guidance
for biopsy guidance for the local staging of uterine and cervical cancer
for the local staging of uterine and cervical cancer  as a problem-solving tool in the evaluation of adnexal masses
as a problem-solving tool in the evaluation of adnexal masses  allowing differentiation between radiation fibrosis and recurrent tumour
allowing differentiation between radiation fibrosis and recurrent tumour  permitting radiologically guided biopsies
permitting radiologically guided biopsies

 it is not widely available but can be used in cervical and ovarian cancer
it is not widely available but can be used in cervical and ovarian cancer it is used for the evaluation of infertility
it is used for the evaluation of infertility distension of the uterine cavity is obtained with sterile saline under direct US visualization
distension of the uterine cavity is obtained with sterile saline under direct US visualization focal pathology can be differentiated from diffuse endometrial conditions with increased accuracy
focal pathology can be differentiated from diffuse endometrial conditions with increased accuracy  it can differentiate between intracavitary, endometrial and subendometrial pathology
it can differentiate between intracavitary, endometrial and subendometrial pathology  it can evaluate tubal patency
it can evaluate tubal patency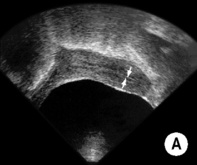
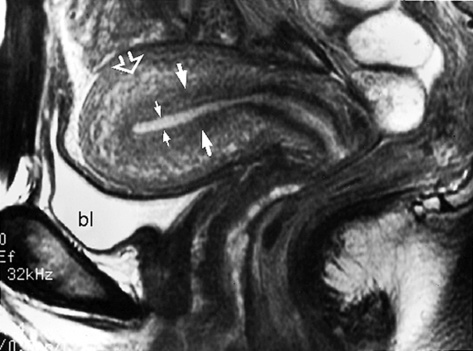
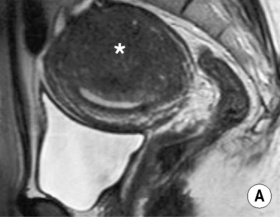
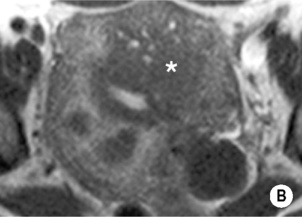
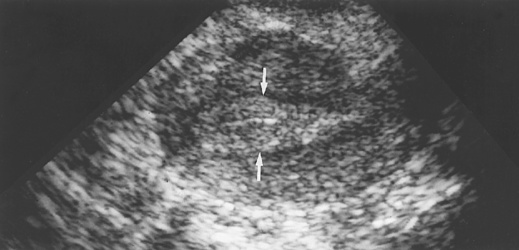
 the band of low SI subjacent to the endometrial stripe represents the inner myometrium or junctional zone (arrows). The outer layer of the myometrium is of intermediate SI (open arrow). bl = bladder.*
the band of low SI subjacent to the endometrial stripe represents the inner myometrium or junctional zone (arrows). The outer layer of the myometrium is of intermediate SI (open arrow). bl = bladder.*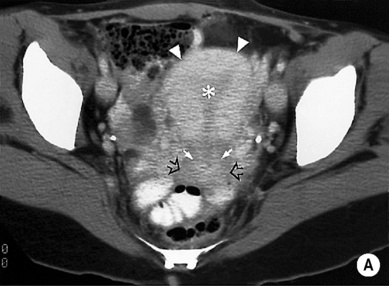





 menstrual disorders
menstrual disorders  infertility
infertility  obstetric complications
obstetric complications
 T2WI: the myometrium is of lower SI than normal
T2WI: the myometrium is of lower SI than normal

 there is some fusion between the two horns (cf. complete separation with didelphys)
there is some fusion between the two horns (cf. complete separation with didelphys) this is often considered a normal variant
this is often considered a normal variant





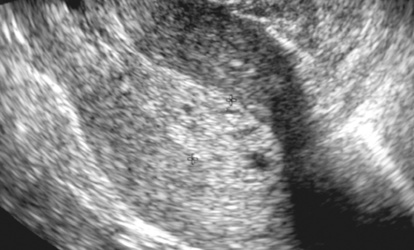
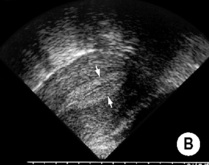
 a well-marginated, hypoechoic, rounded mass within the uterine body
a well-marginated, hypoechoic, rounded mass within the uterine body  distortion of the endometrial complex if there is a submucosal component
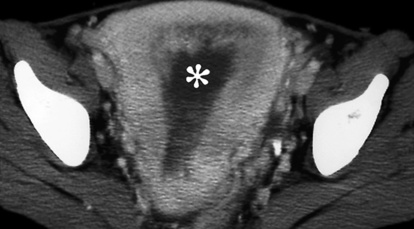
distortion of the endometrial complex if there is a submucosal component necrosis or degeneration may result in low attenuation (± calcification or uterine contour deformity)
necrosis or degeneration may result in low attenuation (± calcification or uterine contour deformity) it can differentiate a pedunculated subserosal leiomyoma from an adnexal mass
it can differentiate a pedunculated subserosal leiomyoma from an adnexal mass MR-guided ultrasound ablation is a recent innovation
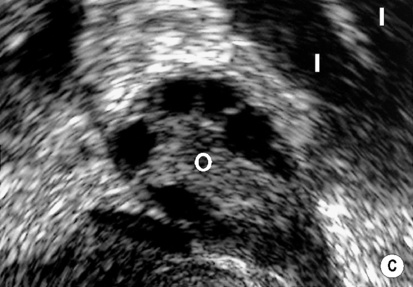
MR-guided ultrasound ablation is a recent innovation there is a preserved endomyometrial interface
there is a preserved endomyometrial interface  there can be central cystic areas and feeding vessels (best seen with colour Doppler)
there can be central cystic areas and feeding vessels (best seen with colour Doppler) T1WI: the polyp is isointense to the endometrium (± hypointense foci)
T1WI: the polyp is isointense to the endometrium (± hypointense foci)  T2WI: the polyp is hypo- to isointense to the endometrium (± cystic changes)
T2WI: the polyp is hypo- to isointense to the endometrium (± cystic changes)  if pedunculated there can be a central hypointense core (± a stalk)
if pedunculated there can be a central hypointense core (± a stalk)  T1WI + Gad: there is homogeneous or heterogeneous enhancement
T1WI + Gad: there is homogeneous or heterogeneous enhancement malignant neoplasm
malignant neoplasm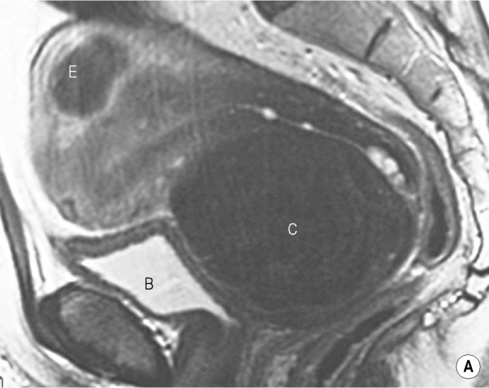








 anovulation
anovulation  obesity
obesity  exogenous hormones
exogenous hormones  functioning oestrogen-secreting ovarian tumours
functioning oestrogen-secreting ovarian tumours


 infertility
infertility  postmenopausal bleeding
postmenopausal bleeding ≥ 16mm (secretory phase)
≥ 16mm (secretory phase) the stripe is isointense or slightly hypointense relative to the normal endometrium (this is a non-specific sign which is also seen with endometrial carcinoma)
the stripe is isointense or slightly hypointense relative to the normal endometrium (this is a non-specific sign which is also seen with endometrial carcinoma)