Fig. 17.1
Pathological changes of the brain in the cases of HFMD. (a, b) Gross specimen observation during autopsy demonstrates swelling of brain tissue and congestion at the surface of the brain. (c) Electron microscopy demonstrates lesions of cerebral infarction. (d) Infiltration of lymphocytes is demonstrated
Cerebellum
Lymphocytic leptomeningitis can be found. The cortex and white matter are subject to focal inflammation, with perivascular infiltration of lymphocytes and plasmocytes.
17.3.3 Lung
The weight of the lung is observed to be increased, with pulmonary blood stasis and edema accompanied by multifocal pulmonary hemorrhage. A small quantity of transparent membranous structures can be locally observed, generally with no obvious infiltration of inflammatory cells and diffuse alveolar lesions. Otherwise, only mild or moderate infiltration of inflammatory cells is observed, with local pulmonary atelectasis as well as shedding and proliferation of a small quantity of alveolar epithelial cells but no virus inclusion body (Fig. 17.2).
Fig. 17.2
Pathological changes of the lung in the cases of HFMD. (a, b) Gross specimen observation during autopsy indicates congestion at the surface and section of the lung and consolidation of some lung lobes. (c–e) Electron microscopy demonstrates peribronchiolar infiltration of cells, pulmonary hemorrhage and consolidation, diffuse pulmonary edema, and hemorrhage
17.3.3.1 Myocardium
The heart is basically normal or shows myocardial hypertrophy, with infiltration of a small quantity of lymphocytes and plasmocytes in the ventricular myocardium, local myocardial necrosis in rare cases, and no virus inclusion body.
In other organs such as the liver, fatty degeneration, blood stasis, and other nonspecific changes can be observed. The lymphatic system is subject to enlarged lymph nodes, proliferation of various lymphocytes, more immunoblasts, and closure of lymph sinus. There is also proliferation of small vessels as well as swelling of endothelial cells (Figs. 17.3 and 17.4).
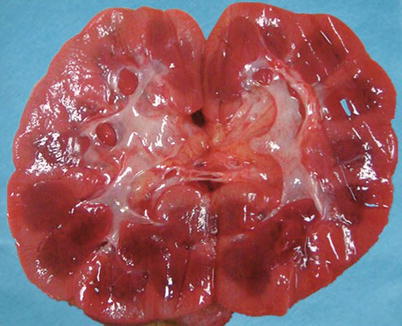
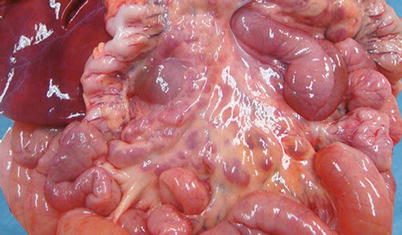
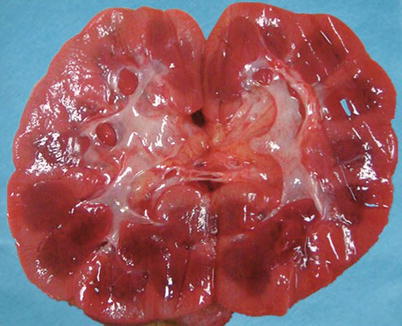
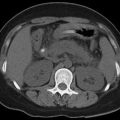
Fig. 17.3
Pathological changes of the kidney in the cases of HFMD. Gross specimen observation during autopsy indicates congestion at the section of the kidney
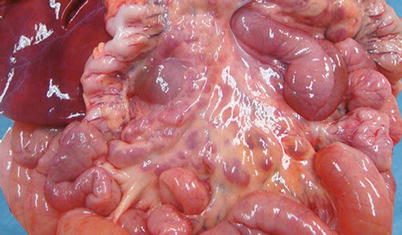
Fig. 17.4
Pathological changes of the mesentery in the cases of HFMD. Autopsy indicates swelling of mesenteric lymph nodes
17.4 Clinical Symptoms and Signs
The incubation period generally lasts for 2–7 days. And the patients might not experience obvious prodromal symptoms but a sudden and acute onset. About 50 % of the patients experience moderate- or low-grade fever (about 38 °C) 1–2 days prior to the onset or along with the onset and accompanying cold-like symptoms such as fatigue, sneezing, cough, and runny nose. The patients may also experience gastrointestinal symptoms such as poor appetite, nausea, vomiting, and abdominal pain.
17.4.1 Manifestations of Common Type
The patients experience an acute onset, with fever, scattering herpes at the oral mucosa, as well as macula, papules, and herpes at the hand, foot, and buttock. Inflammatory red halo can be observed around the herpes, with a small quantity of fluid in the herpes. The accompanying symptoms include cough, runny nose, and poor appetite. In some cases, the patients only experience skin rash or herpetic angina, which can be mostly cured within 1 week with favorable prognosis. In some cases, the skin rashes are atypical, such as skin rashes only within one area or only manifestation of maculopapules.
17.4.2 Manifestations of Severe Type
In rare cases, especially toddlers under the age of 3 years, the conditions develop rapidly, with occurrence of meningitis, encephalitis (with brain stem encephalitis as the most dangerous), encephalomyelitis, pulmonary edema, and circulatory disturbance 1–5 days after the onset. In extremely rare cases, the patients experience severe or critical conditions, with possible occurrence of death. The surviving patients commonly sustain sequela.
17.4.2.1 The Nervous System
The patients experience poor spirits, drowsiness, susceptibility to fears, headache, vomiting, delirium, and even coma. The patients may also experience trembling limbs, myoclonia, nystagmus, ataxia, eyeball movement disorder, weak or acute flaccid paralysis (AFP), and convulsions. By physical examinations, signs meningeal irritation can be found, with weakened or absent tendon reflex and Babinski sign positive.
17.4.2.2 The Respiratory System
The patients experience shortness of breath, dyspnea or change of respiratory rhythm, cyanosis of lips, and coughing with white, pinkish, or bloody foamy sputum. By auscultation, moist rales or phlegm wheezing can be heard.
17.4.2.3 The Circulatory System
The patients experience grayish pale face, skin disturbance, cold limbs, cyanosis of fingers (toes), cold sweating, and prolonged refilling period of the capillaries. The patients may also experience increased or decreased heart rate, superficial and rapid pulses, as well as increased or decreased blood pressure. In other cases, the pulse may be weakened or absent.
Some scholars believed that HFMD caused by EV71 can be hardly distinguished from HFMD caused by CoxA16 based on the clinical symptoms. However, EV71 infection is commonly accompanied by acute aseptic meningitis, brain stem encephalitis, acute flaccid paralysis, and neurogenic pulmonary edema, which is more dangerous than CoxA16 infection. However, CoxA16 infection is simply manifested as HFMD, with no other accompanying diseases. Studies also indicated that the size of herpes as well as the style of rash erupting are different between EV71-induced and CoxA16-induced HFMD.
17.5 HFMD-Related Complications
17.5.1 The Central Nervous System
17.5.1.1 Brain Stem Encephalitis
The infant patients commonly experience myoclonia, trembling, ataxia, nystagmus, and cranial nerve paralysis, such as swallowing nerve, abduct nerve, and facial nerve paralysis. The clinical manifestations are categorized into three levels: Level I, only manifestations of myoclonus, trembling, and ataxia; Level II, concurrence of myoclonus and autonomic nerve dysfunction (including nausea, vomiting, systemic coldness, palpitation, shortness of breath, unstable blood pressure, and elevated blood sugar); and Level III, autonomic nerve dysfunction and pulmonary edema or pulmonary hemorrhage. Pulmonary edema or hemorrhage is manifested by sudden tachypnea, tachycardia, cyanosis, shock, rales at lung and foamy sputum, circulatory failure, coma, absent pupil reflex to light, and apnea. Studies have demonstrated that vomiting, tachycardia, high blood pressure, and dysphagia are the important signs indicating brain stem dysfunction.
17.5.1.2 Aseptic Meningitis
The patients experience severe headache and accompanying fever, vomiting, and neck rigidity. In some cases, the patients experience simultaneous involvement of the meninges and brain parenchyma, which is known as the meningoencephalitis type. Accompanying various degrees of consciousness disturbance may be found.
17.5.1.3 Acute Flaccid Paralysis
The patients experience acute unilateral or bilateral limb weakness, decreased muscle strength, movement difficulty, and weakened or absent tendon reflex. Most patients can be completely cured, rarely with permanent neurological sequela such as limb paralysis.
17.5.1.4 Cerebellar Ataxia
EV71 infection might cause acute cerebellar ataxia, and the patients experience trunk ataxia, with/without accompanying nystagmus, most of which can be completely healed. Although brain function can be completely recovered, accompanying various degrees of cerebral cortex atrophy might occur.
17.5.2 Neurogenic Pulmonary Edema
Neurogenic pulmonary edema refers to pulmonary edema caused by cranial or brain injury or other diseases of the central nervous system, with no primary cardiopulmonary disease, which is also known as central pulmonary edema. At its early stage, the patients only experience increased heart rate, elevated blood pressure, and tachypnea with irregular breathing rhythm (with tachypnea indicating early interstitial pulmonary edema and irregular breathing rhythm indicating brain stem encephalitis). In scientific literature, it has been reported that child patients experience increased heart rate as well as elevated or declined blood pressure.
17.6 Diagnostic Examination
17.6.1 Laboratory Test
17.6.1.1 Routine Test
Increased peripheral blood WBC count, blood sugar, and early hypersensitivity C-reactive protein (hs-CRP) have clinical significance. The peripheral blood WBC count and blood sugar can be used to assess the condition and predict the prognosis, while Hs-CRP is a sensitive indicator for the early diagnosis and clinical medication.
17.6.1.2 Blood Biochemical Examination
In some cases, the patients experience mild elevation of ALT, AST, blood sugar, and other myocardial enzymes. The degree of elevation is positively related to the severity of the condition. In addition, it is closely related to the prognosis. At the convalescence stage, these indicators gradually return to normal. Their high levels at the convalescence stage are possibly related to immune lesions.
17.6.1.3 Cerebrospinal Fluid Examination
The titer of the virus and antibody at the acute stage being at least four times above the convalescence stage or the titer ≥1:256 has diagnostic value.
17.6.1.4 Etiological Examination
The etiological examinations include viral isolation and culture, RT-PCR, fluorescent quantitative PCR, and serological test. Enterovirus isolation after tissue culture is the golden standard for the diagnosis. Specific nucleic acid test of the enterovirus, such as EV71 and CoxA16, is the main examination to define the pathogen of HFMD, which is efficient, convenient, highly sensitive, and specific. In addition, such a test is more sensitive than cell culture. As one of the diagnostic examinations for enterovirus infection, it can be applied to determine the neutralizing antibody titer of serum enterovirus. The serum collected at the acute stage is commonly compared to that collected at the convalescence stage, and an increase of at least four times of the antibody titer is defined as positive of viral infection.
17.6.2 Diagnostic Imaging
17.6.2.1 X-Ray and CT Scanning
X-ray and CT scanning are commonly applied to diagnose the respiratory complications of HFMD, whose demonstrations are related to the changes of the condition. The demonstrations show severity, changes, and prognosis of the condition, which are of clinical significance in assessing the condition, changing therapeutic plans, and predicting prognosis.
17.6.2.2 MR Imaging
MR imaging is the most sensitive radiological examination for the diagnosis of HFMD complicated by encephalitis, especially brain stem encephalitis. It can be applied to detect the location, range, and severity of the lesions.
17.7 Imaging Demonstrations
17.7.1 Neurological Complications
17.7.1.1 Aseptic Meningitis
Plain MR imaging commonly demonstrates no abnormalities, and contrast imaging demonstrates no meningeal enhancement, which is different from bacterial meningitis. In cases complicated by viral encephalitis, MR imaging demonstrates necrosis and edema at bilateral temporal lobes and bilateral frontal lobes, with long T1 long T2 signals at the affected cerebral lobes.
17.7.1.2 Brain Stem Encephalitis
EV71 can cause brain stem encephalitis, with lesions commonly found at the medulla oblongata, pons, midbrain, and commonly dorsal brain stem. At the acute stage, the lesions are demonstrated with high T2WI signal and no obvious space-occupying effect but no T1WI signal, suggesting acute inflammation of the brain tissue. Most of these lesions are reversible. Along with further development of the condition, the lesions are demonstrated with low T1WI signal, high T2WI signal, high FLAIR signal, and high DWI signal, with poorly defined boundaries and inapparent space-occupying signs. In some cases, the brain stem is subject to atrophy and shrinkage in the advanced stage, with central cavity at the brain stem (Figs. 17.5, 17.6, and 17.7).
Fig. 17.5
EV71-induced HFMD complicated by brain stem encephalitis. (a, b) (indicated by white arrow) Sagittal T1WI demonstrates long patches of relatively low signals at the dorsal medulla oblongata. (c, d) (indicated by black arrow) Sagittal T2WI demonstrates long patches of relatively high signals at the dorsal medulla oblongata with poorly defined boundaries and no obvious space-occupying effect. (e) Transverse T2WI demonstrates small patches of relatively high signals at the left dorsal medulla oblongata. (f) (indicated by white arrow) Transverse T1WI demonstrates small patches of relatively low signals at the left dorsal medulla oblongata with poorly defined boundaries and no obvious space-occupying effect
Fig. 17.6
EV71-induced HFMD complicated by brain stem encephalitis. (a, b) MR imaging demonstrates irregular patches of slightly long T1 long T2 signals at the brain stem (including medulla oblongata and pons). FLAIR demonstrates moderate high signal with poorly defined boundary. T2WI more clearly demonstrates the lesions. Transverse T1WI demonstrates small patches of relatively low-signal shadows at the medulla oblongata (indicated by long arrow) and the pons (indicated by short arrow), with poorly defined boundaries. (c, d) Transverse T2WI demonstrates small patches of relatively high-signal shadows at the medulla oblongata (indicated by long arrow) and the pons (indicated by short arrow) with poorly defined boundaries. The signal is more obvious at the right medulla oblongata than at the left medulla oblongata. (e, f) FLAIR demonstrates moderate high signal, with poorly defined boundary (indicated by arrow); (g, h) Sagittal T1WI demonstrates small patches of relatively low-signal shadows (indicated by arrow) at the medulla oblongata and the pons. (i, j) Sagittal T2WI demonstrates small patches of relatively high-signal shadows (indicated by arrow) at the medulla oblongata and the pons, with no obvious space-occupying effect
Fig. 17.7
HFMD complicated by pons encephalitis and central spinal canal cavity. (a) Transverse T2WI demonstrates patches of high signals at the pons. (b) Transverse T1WI demonstrates patches of low signals at the pons. (c) Sagittal T1WI demonstrates C3-C6 spinal central canal with stripes of relatively low signals. (d) Sagittal T2WI demonstrates C3–C6 spinal central canal with stripes of relatively high signals (Note: The case and the figures were provided by Lao Q. from Hangzhou Children Hospital, Hangzhou, Zhejiang, China)
Case Study 1
A boy infant aged 23 months experienced repeated high fever for 3 months and non-injective vomiting for 1 day. By physical examination, poor consciousness, lethargy, shortness of breath, cyanosis, and paroxysmal limb trembling are evident. By laboratory test, nucleic acid of the pathogenic EV71 was detected in his feces by RT-PCR.
Case Study 2
A boy aged 4 months experienced skin rashes for 5 days as well as fever and limb trembling for 2 days. He also experienced convulsion for once. His clinical diagnosis was EV71-induced HFMD and viral meningoencephalitis.
Case Study 3
An infant girl aged 18 months experienced fever, oral herpes, and skin rashes on both hands for 3 days and startling for 2 days. By physical examination, her body temperature rose up to 39.1 °C with frequent startling, drowsiness, vomiting, muscular strength level V, slight neck resistance, and positive knee tendon reflex (++). By blood biochemistry, WBC was 13.5 × 109/L; N, 64.7 %; L, 27.8 %; PLT, 143 × 109/L; and CR, 10.6 mg/L. By cerebrospinal fluid examination, the cerebrospinal fluid was colorless, transparent, and Pandy test positive, with karyocytes 140 × 106/L, RBC 20 × 106/L, L 92 %, protein 484 mg/L, glucose 3.42 mmol/L, and chloride 133 mmol/L. Laboratory test results indicated encephalitis. Cranial CT scanning demonstrated no abnormality. MR imaging demonstrations indicated brain stem encephalitis and spinal central canal cavities. The clinical diagnosis was severe HFMD complicated by brain stem encephalitis and central spinal canal cavities.
17.7.1.3 Encephalitis
The radiological demonstrations of encephalitis are nonspecific, with large range of lesions involving the cerebral lobes, basal ganglia, thalamus, brain stem, cerebellum, corona radiata, and corpus callosum. The lesions mainly involve the gray matter, possibly with concurrent involvement of the white matter. However, their space-occupying effect is relatively slight, only with local broadening of the gyrus, shallow sulcus, and no shift of the midline structures. The lesions are demonstrated as small patches with low density. MR imaging demonstrates long T1 long T2 signals, high T2WI FLAIR signal, and high DWI signal, with poorly defined boundaries. CT scanning at the late stage (2 months after onset) demonstrates obvious shrinkage of the lesions and small spots of low-density lesions. MR imaging demonstrates small spots of long T1 long T2 signal, high T2WI FLAIR signal, and low DWI signal. In cases with brain arterial endarteritis, which leads to cerebral infarction or hemorrhagic cerebral infarction, MR imaging demonstrates signs of cerebral infarction. During the hyperacute stage, T1WI and T2WI fail to demonstrate any significant signal change, but high DWI signal. During the acute stage, the lesions are demonstrated as low T1WI signal, high T2WI signal, and high FLAIR signal. The lesions eventually develop into encephalomalacia (Figs. 17.8, 17.9, and 17.10). In cases complicated by hemorrhagic cerebral infarction, the signal changes are complex. In the advanced stage, brain atrophy can be demonstrated.
Fig. 17.8
EV71-induced HFMD complicated by encephalitis. (a–d) MR imaging demonstrates long T1 long T2 signal shadows at the midbrain and the left dorsal thalamus, slight rightward shift of the mesencephalic aqueduct due to compression, dilated 3rd brain ventricle, and bilaterally symmetric dilation of the lateral ventricles. (e, f) FLAIR demonstrates high signal of the above lesions. (g, h) Contrast imaging demonstrates no enhancement of the lesions
Fig. 17.9
EV71-induced HFMD complicated by encephalitis. (a, h) Transverse imaging demonstrates long stripes of low signal at bilateral basal ganglia, with mainly high FLAIR and DWI signals and observable small patches of abnormal signals. T1WI demonstrates low signal, while T2WI and FLAIR demonstrate high signals, with no significant space-occupying effect. Basal ganglia is demonstrated with cerebral infarction and accompanying hemorrhage. The left temporal lobe is demonstrated with flakes of long T1 long T2 signals and high FLAIR and DWI signals. The diagnosis is suspected to be left temporal encephalitis. (a, b) T1WI demonstrations. (c, d) T2WI demonstrations. (e, f) FLAIR demonstrations. (g, h) DWI demonstrations
Fig. 17.10




EV71-induced HFMD complicated by encephalitis. (a, b) Sagittal MR imaging demonstrates small long stripes of slightly long T1 slightly long T2 signals (indicated by arrow) at the posterior dorsal superior medulla oblongata; (c, z) The brain stem is demonstrated with multiple small patches of abnormal signal shadows with long T1 long T2 signal (indicated by arrow), flakes of long T1 long T2 signal (indicated by arrow) at the bilateral centrum semiovale and basal ganglia, and high FLAIR and WDI signal (indicated by arrow). The small patches are demonstrated by T1WI as high signal while by T2WI and FLAIR as low signal, with no significant space-occupying effect. The lesions are actually cerebral infarction at the basal ganglia with accompanying hemorrhage. (w, bb) The interface of the left frontal and parietal lobes is demonstrated with flakes of long T1 long T2 signals and high FLAIR and DWI signals, which is suspected to be left frontoparietal encephalitis. (c–h) FLAIR demonstrations; (i–n) T2WI demonstrations; (o–v) T1WI demonstrations; (w–bb) DWI demonstrations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree