The head module contains three groups of regions:
Cranial
Facial
Airways
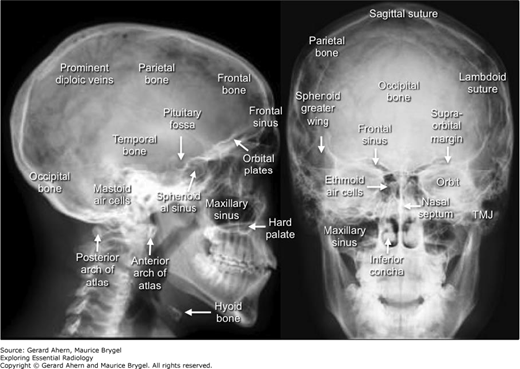
The cranial regions include the scalp, temporal region, cranial cavity, orbit, and ear. The importance of the cranial cavity contents makes it the dominant group of images represented here. They are divided into congenital, hemorrhage, tumors, trauma, and infection.
The facial regions include superficial regions (face, parotid) and deep regions (infratemporal region, pterygopalatine fossa, deep styloid region).
The airway regions include nasal regions (nasal cavity, paranasal sinuses, nasopharynx), oral regions (oral cavity, oropharynx), and laryngeal regions (larynx, laryngopharynx).
Some miscellaneous images are grouped together for convenience (e.g., Paget’s disease).
High prominent forehead, flat posterior skull, flat face, shallow orbits, broadly spaced eyes, low set ears, mental deficiency, and deformities of the hands and feet.
Brachycephaly due to coronal suture closure (Apert syndrome).
Surgery to prevent closure of the coronal suture plus facial corrections. Correct syndactyly.
Skull deformity at birth. Mental deficiency if later.
Craniosynostosis (metopic and coronal).
Surgical correction.
Skull deformity at birth. Mental deficiency if later.
Craniosynostosis (sagittal).
Surgical correction.
Skull deformity at birth. Mental deficiency if later.
Multiple suture craniosynostosis (coronal, sagittal, and lambdoid).
Surgical correction.
Learning difficulties, developmental delays, and possible symptoms and signs of involvement of other viscera.
Multiple small lesions consistent with cerebral tubers (tuberous sclerosis).
Medical treatment often improves the effects.
Headaches, dizziness, facial pain, impaired gag, dysphagia, dysautonomia.
Herniation of cerebellar tonsils through large foramen magnum, hydrocephalus (not seen), and syringomyelia (Chiari malformation).
May require surgical decompression.
History of major or minor head injury, often in a young man who has been drinking alcohol. Headache, lucid interval (4–6 hours), then worsening neurological signs.
Right extradural collection with midline shift and a compressed lateral ventricle.
Right lateral craniotomy, decompression and hematoma evacuation.
History of major or minor head injury, often in an elderly person. Frequently a minor headache with subtle personality changes. Neurological symptoms and signs depend on whether acute or chronic type.
Left frontal and temporoparietal subdural hemorrhage. Some midline shift.
Craniotomy, decompression, and hematoma evacuation if patient well enough and clinical signs are significant.
Sudden collapse in a young adult or worsening of stroke in an elderly patient. Symptoms and signs of a massive intracranial bleed. May be due to a berry aneurysm (younger patient) or an intracerebral bleed rupturing into the cerebrospinal fluid system (elderly patient).
Subarachnoid bleed into frontal regions and the basal cisterns. Fissures filled with blood.
If sudden, often dies before treatment. If not, a berry aneurysm may be clipped or coiled. In the elderly, usually symptomatic treatment only.
History of sudden collapse and severe headache with subarachnoid bleed. May be found incidentally on computed tomography scan, ordered for some other reason.
Large berry aneurysm on division of basilar artery into posterior cerebral arteries.
Coiling (above) or clipping if patient well enough.
History of hypertension with onset of stroke symptoms and signs.
Left temporal bleed with involvement of subarachnoid space plus secondary hydrocephalus.
Dependent on patient’s clinical situation.
History of significant head trauma.
Corpus callosum and left temporal bleed, sphenoid sinus fluid plus air in the orbits.
Conservative treatment likely; surgery if possible but is a very sick patient.
History of vascular problems; symptoms and signs of a stroke.
Hypertensive bleed left cerebrum and lateral ventricle; age related atrophy.
Probably just conservative treatment; may embolize the causative vessel.
History of progressive cerebellar symptoms and signs in a patient with known breast carcinoma.
Enhancing mass lesion in left cerebellar hemisphere consistent with metastasis.
Primary will require treatment, but the secondaries are beyond definitive treatment.
This patient had a history of human immunodeficiency virus with worsening neurological symptoms and signs.
Large ovoid mass in left basal ganglia and corona radiata with edema and lateral ventricle compression (lymphoma).
Likely to undergo non-surgical treatment with high dose drugs via multiple routes.
History of progressive temporal and parietal neurological symptoms and signs.
Large left temporal and parietal lobe lesion of a cystic nature (astrocytoma).
Surgical removal if possible but likely to be too invasive.
Headache with endocrine symptoms specific to the hormone secreted (if any). Worsening tunnel vision.
Large lobulated pituitary mass eroding the pituitary fossa and compressing the suprasellar structures. A large pituitary adenoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree