Head and Neck Procedures
Srikar Adhikari
INTRODUCTION
Head and neck procedures are frequently performed in the emergency department (ED). Traditionally, surface anatomical landmarks have been used by physicians to determine the accurate approach to performing these procedures. As a result, there was considerable variation in both success and complication rates. In recent years, ultrasound is increasingly being used at the bedside by clinicians. Ultrasound can be extremely useful in facilitating various head and neck procedures in the ED. The use of ultrasound guidance can potentially decrease complications and improve patient safety. A thorough understanding of the basic principles of ultrasound, sonographic anatomy, and hand-eye-coordination skills is crucial to use ultrasound for procedural guidance.
ASPIRATION OF PERITONSILLAR ABSCESSES
Clinical Indications
Successful drainage of a suspected peritonsillar abscess can present a significant challenge. Unlike cutaneous abscesses, the anatomic location of a peritonsillar abscess is not as accessible as the skin for aspiration. Additionally, the proximity of vascular structures makes needle aspiration potentially more complicated. Complications with blind needle aspiration include injury to the carotid arteries, jugular veins, or parotid gland. Additionally, blind needle aspiration of the peritonsillar region has a reported false-negative rate of 10% to 12% (1). Bedside intraoral ultrasound has been shown to be useful to differentiate peritonsillar abscess from cellulitis, localize the abscess, and perform an aspiration. Ultrasound thus avoids discomfort from a dry tap. The superiority of ultrasound-guided aspiration over the landmark approach has been well documented in the literature (2, 3, 4). The ability of ultrasound to define the margins of the tonsils, their relationship to adjacent vascular structures, and provide real-time guidance to insert the needle makes the procedure very safe.
Procedure
The technique used to perform the aspiration is similar to ultrasound-guided vascular procedures. The only difference is that a high-frequency (5-10 MHz) curved array endocavity probe is used to guide the aspiration of peritonsillar abscess because its shape allows placement in the posterior pharyngeal space. The procedure is typically performed freehand, but a needle guide can be attached to the endocavity transducer to perform the aspiration. However, it adds significant costs to the procedure and also limits the distance the needle can be inserted into the oropharynx. The manual dexterity needed to manipulate the endocavity probe while performing aspiration requires some practice. Generally, the procedure is performed by one operator, holding the probe with one hand and performing the aspiration with the other hand, while making appropriate adjustments of the probe to visualize the needle. Prior studies have clearly demonstrated the ability of the emergency physicians to effectively use bedside ultrasound for both the diagnosis of peritonsillar abscess and real-time guidance for needle aspiration (3, 4, 5).
Adequate systemic analgesia should be given to the patient prior to performing the procedure. Topical anesthetic should be sprayed into the posterior pharyngeal area to avoid gagging and overcome trismus. After placing gel over the tip of the endocavity probe, it should be covered with a sheath or condom. The endocavity probe is then inserted into the oral cavity and advanced into the pharyngeal region. The peritonsillar area is scanned systematically in both long and short axes. The presence of the peritonsillar abscess should be confirmed, which can have variable appearances on ultrasound. Often, a peritonsillar abscess is visualized as a hypoechoic or complex cystic mass, typical of most abscesses (Fig. 25.1). The depth of the abscess cavity from the mucosal surface
should be noted, and the length of the needle required to enter the abscess cavity should be determined prior to aspiration. The carotid artery and its relationship to the abscess cavity should be assessed. It is visualized as an anechoic tubular structure along the posterolateral aspect of the tonsil, generally within 5 to 25 mm of an abscess cavity (Fig. 25.1). Color Doppler can help identify the carotid artery. The relationship of the tonsillar tissue, abscess cavity, and carotid artery is best assessed in transverse axis. The transducer should be held horizontally, and the fluid collection should be localized. Once the abscess is localized, an 18-gauge 2-inch needle attached to a 5- to 10-mL syringe is inserted lateral to the tip of the transducer (Fig. 25.2). Alternatively, a 14-gauge needle can be used if purulent material appears too thick. The needle should be placed in the middle of the tip of the transducer, exactly in the same plane as the ultrasound signal. As with vascular access procedures, real-time guidance should be used. The same principles should be employed to track the entire course of the needle. The needle should be advanced slowly under direct visualization with ultrasound. If the needle tip is not seen at any point, no further advancement should be made. Once the needle penetrates the abscess cavity, aspiration should be performed under real-time guidance (Fig. 25.3). Reduction in the size of the abscess cavity should be seen on ultrasound (Fig. 25.4). Occasionally, saline injection into the abscess cavity might be necessary to break up the loculations and facilitate aspiration (Fig. 25.5).
should be noted, and the length of the needle required to enter the abscess cavity should be determined prior to aspiration. The carotid artery and its relationship to the abscess cavity should be assessed. It is visualized as an anechoic tubular structure along the posterolateral aspect of the tonsil, generally within 5 to 25 mm of an abscess cavity (Fig. 25.1). Color Doppler can help identify the carotid artery. The relationship of the tonsillar tissue, abscess cavity, and carotid artery is best assessed in transverse axis. The transducer should be held horizontally, and the fluid collection should be localized. Once the abscess is localized, an 18-gauge 2-inch needle attached to a 5- to 10-mL syringe is inserted lateral to the tip of the transducer (Fig. 25.2). Alternatively, a 14-gauge needle can be used if purulent material appears too thick. The needle should be placed in the middle of the tip of the transducer, exactly in the same plane as the ultrasound signal. As with vascular access procedures, real-time guidance should be used. The same principles should be employed to track the entire course of the needle. The needle should be advanced slowly under direct visualization with ultrasound. If the needle tip is not seen at any point, no further advancement should be made. Once the needle penetrates the abscess cavity, aspiration should be performed under real-time guidance (Fig. 25.3). Reduction in the size of the abscess cavity should be seen on ultrasound (Fig. 25.4). Occasionally, saline injection into the abscess cavity might be necessary to break up the loculations and facilitate aspiration (Fig. 25.5).
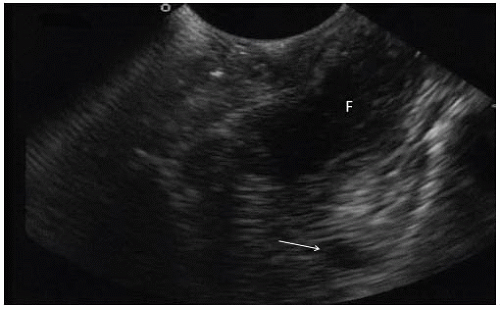 FIGURE 25.1. B-Mode Image of a Peritonsillar Abscess Obtained with an Endocavity Probe. Note the abscess cavity with hypoechoic fluid collection (F) in the near field and anechoic carotid artery (arrow) posterolateral to the abscess cavity in the far field. (Courtesy of Michael Blaivas, MD.)
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




