Hemangiopericytoma
Deborah R. Shatzkes, MD
Key Facts
Terminology
Hemangiopericytoma (HPC)
Uncommon, slow-growing vascular neoplasm of varying malignancy
Imaging
Most HPCs occur in lower extremities, pelvis
15% occur in head and neck
Intracranial/meningeal: Parasellar & paraclival
Orbit, cervical soft tissues, sinonasal cavity
CT findings
Well circumscribed, lobular, avidly enhancing; more invasive behavior if high grade (CECT)
May see bone erosion or remodeling (bone CT)
MR findings
Intermediate T1, high T2 signal
Vascular flow voids common
Prominent enhancement, typically uniform
Top Differential Diagnoses
Skull base meningioma
Skull base metastasis
Skull base trigeminal schwannoma
Clivus chordoma
Orbital cavernous hemangioma
Sinonasal angiomatous polyp
Pathology
50% malignant, typically low grade
Clinical Issues
Resection is treatment of choice ± XRT
Local recurrence ≤ 50%; 30% metastases < 10 years
HPC mimics many more common tumors
Consider HPC if avidly enhancing, well-circumscribed mass
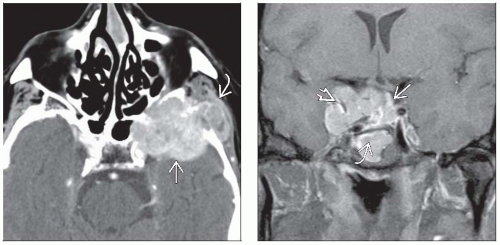 (Left) Axial CECT shows skull base HPC with bone destruction and extension into middle fossa
 and masticator space and masticator space  . Absence of hyperostosis is clue that this is not meningioma, though distinction from other destructive extraaxial masses is difficult. (Right) Coronal T1WI C+ FS MR reveals parasellar HPC with intrasellar . Absence of hyperostosis is clue that this is not meningioma, though distinction from other destructive extraaxial masses is difficult. (Right) Coronal T1WI C+ FS MR reveals parasellar HPC with intrasellar  and infrasellar and infrasellar  components and prominent internal flow voids components and prominent internal flow voids  . Preoperative diagnosis was meningioma; these lesions may be indistinguishable on imaging. . Preoperative diagnosis was meningioma; these lesions may be indistinguishable on imaging.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|