Grade
Symptoms
I
LUTS without gross hematuria
II
LUTS + gross hematuria
III
LUTS + gross hematuria + clots
IV
LUTS + gross hematuria + clots causing urinary retention
Infectious Etiology
Infectious HC is most commonly seen in immunocompromised patients, especially those that are undergoing bone marrow or hematopoietic stem cell transplant. In fact, between 10 and 25 % of bone marrow transplant (BMT) patients suffer from HC [3]. The majority is seen with viral-mediated HC; however, one can see other forms of infectious HC as discussed below.
Viral-Mediated HC
The immunosuppression in transplant patients increases the risk of opportunistic infection, and polyoma viruses (BK and JC virus) along with adenoviruses are the most common causative agent of HC in this population. Infection with polyoma virus is opportunistic, as up to 80 % of all adults are colonized. The virus infects many different cell types including urothelial cells of the renal pelvis, ureters, and bladder [4–6]. In immunocompetent hosts, they lie dormant following infection – viral reactivation requires a combination of predisposition to reactivation, target organ damage, and host immune dysfunction.
Adenovirus represents another common infectious agent associated with HC in immunocompromised patients. The incidence of adenovirus infection ranges from 10 to 20 %, with renal transplant patients being at increased risk of HC associated with infection [7, 8]. Children have been shown to have onset of symptoms sooner than adults (30 vs. 90 days) [9].
While polyoma virus and adenovirus infection cause HC in immunocompromised hosts, infection with cytomegalovirus (CMV) has recently been shown to cause HC despite seemingly normal immune function. In one report, an otherwise healthy 3-year-old boy with gross hematuria had cystoscopic evidence of HC – bladder biopsy was consistent with CMV infection and viral DNA was present in both serum and urine samples. In this patient, symptoms resolved spontaneously with conservative management 1 month after onset [10].
Diagnosis
Onset is usually within the first 30–90 days following initiation of immunosuppression, though symptoms can arise as far as 1 year later. Symptom severity correlates with increased rates of complication including bladder perforation, hydronephrosis, and kidney injury [11]. Viral shedding in the urine is seen both in active and dormant infection, though studies have shown that patients with viruria prior to immunosuppression are at almost twice the risk of developing HC (9 % vs. 16 %) [12]. Diagnosis can be made with urine cytology or PCR testing for viral DNA. These patients should be monitored closely so that intervention can be timely. Adenovirus viruria is present during active disease and can be detected with PCR testing of the urine [13].
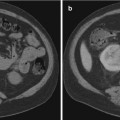
Infectious causes of HC share similar imaging findings. Bladder ultrasound as well as computed tomography (CT) can show a thickened bladder wall along with increased attenuation of urine and intraluminal clots. Magnetic resonance imaging will show inflammation and edema within the bladder wall [14, 15].
Management
Management of HC caused by polyoma virus includes reduction of immunosuppression, treatment with antibiotic and/or antiviral agents along with supportive treatment targeted at preventing urinary clot retention and hemorrhagic anemia, as well as symptom control (discussed below). In patients with additional risk factors for renal failure or concern for renal transplant graft dysfunction, reduction of immunosuppression alone can be quite effective and avoids the use of nephrotoxic agents. One study demonstrated that a 50 % reduction in immunosuppressive agents resulted in clearance of BK viremia in 58 % of patients [16]. Cidofovir is viral DNA synthesis inhibitor and has demonstrated utility in treating patients with polyoma virus-associated HC, with the limiting factor of nephrotoxicity [17–19]. Most studies have investigated intravenous cidofovir, though there are also reports of effectiveness in intravesical instillation. This is useful in patients where the nephrotoxicity of intravenous cidofovir is prohibitive. In a retrospective study, treatment with IV cidofovir resulted in 67 % of patients with complete resolution of HC and another 12 % with partial resolution [20]. In the same study, 60 % treated with intravesical cidofovir had complete resolution of symptoms and another 20 % had partial resolution. Another agent shown to be effective in polyoma virus infection is leflunomide, a pyrimidine synthesis inhibitor with both immunosuppressive and antiviral properties. One study demonstrated an 88 % reduction in viremia following treatment with leflunomide combined with reduction in immunosuppression [21]. Finally, fluoroquinolones are effective both in prophylaxis and treatment of polyoma virus-associated HC [22, 23]. A retrospective study of 92 consecutive patients demonstrated that prophylaxis with ciprofloxacin prior to and during immunosuppression led to a significant reduction in the incidence of BK virus-associated HC (2.6 % vs. 20.9 %) [24].
The principles of therapy are similar to that for polyoma virus such as reduction of immunosuppression, the use of antivirals, and symptomatic control are the same as that for adenovirus in general. There are no specific antiviral treatments for adenovirus, though agents such as ganciclovir, vidarabine, ribavirin, and cidofovir have all been used with some success [25–28]. The best studied of these agents include ribavirin and cidofovir, though to date, there are no randomized controlled trials (RCT) investigating their effect.
Nonviral Infectious HC
While viral HC is most common, bacterial, fungal, and parasitic infection can also cause HC. Bacterial cystitis, though usually a benign disease, has been reported in rare but severe cases to progress to HC with potentially fatal outcomes including spontaneous bladder perforation [29]. The most common bacterial causes are E. coli, Proteus spp., Klebsiella spp., and S. saprophyticus [30]. There is a recent report of a patient with acalculous cholecystitis and acute HC caused by S. typhi [31]. Regardless of the causative agent, management of bacterial HC relies on culture-driven antimicrobial therapy along with symptom control.
HC is also a known sequelae of tuberculosis of the bladder. This is seen in the immigrant population and affected individuals usually have concurrent renal tuberculosis [32].
Fungal causes of HC are rare and usually associated with treatment of bacterial cystitis [33]. Organisms reported to cause hemorrhagic complications include Candida albicans, Cryptococcus neoformans, Aspergillus fumigatus, and Torulopsis glabrata. Characteristic findings include white plaques overlying the urothelium. As with bacterial cystitis, symptoms resolve following treatment of the underlying infection [34]. In the United States, parasitic HC is rare. However, bladder schistosomiasis is a serious health concern in developing nations, primarily in Africa [35]. Infection starts with exposure to contaminated water, where larvae penetrate the skin. Following maturation in the lungs and liver, adult worms travel to the pelvic veins and deposit eggs in the bladder wall. The eggs incite an inflammatory reaction with subsequent fibrosis. During the inflammatory phase, nodular bladder wall thickening is seen on CT urography. In the chronic fibrotic phase, bladder volume is decreased and imaging shows a thickened calcified bladder [36].
Treatment with praziquantel will treat the infection but the chronic fibrotic changes cannot be reversed [37]. In rare cases, hemorrhagic cystitis has been noted in association with hydatid cyst disease caused by Echinococcus granulosus [38]. Treatment with albendazole leads to resolution of symptom.
Noninfectious Etiology
Radiation-Induced HC
Radiation-induced cystitis is seen in adult patients with pelvic malignancy and pediatric patients following whole-body radiation in preparation for bone marrow transplantation. Its presentation can be divided into acute and late radiation cystitis.
The overall incidence of radiation cystitis ranges from 5 to 10 %. This number varies greatly depending on the series and the patient population studied. Patients receiving larger doses of radiation or radiation directed at the bladder have an increased risk of developing radiation cystitis of worsening severity [39]. It is therefore not surprising that patients who have undergone radiation treatment for bladder cancer have the highest rates of radiation cystitis, with almost 10 % of patients having small shrunken bladders [40]. Patients treated with radiation for either prostate or cervical cancer have a 6–8 % risk of grade III/IV HC [41, 42]. Acute radiation cystitis occurs either during or shortly after radiation therapy (usually within 3 months) and is caused by injury to the fast dividing cells of the bladder mucosa. The symptoms are typically self-limiting and include dysuria, urgency, and frequency. These can usually be managed conservatively. In the acute phase, imaging findings are similar to those seen in infectious HC. Late radiation cystitis develops anywhere between 6 months and 20 years after therapy. It is caused by damage to vascular and connective tissues, which have a much slower cell turnover rate than the bladder mucosa. Endothelial cell damage and perivascular fibrosis are seen months to years after radiation and can result in vascular occlusion/bladder ischemia [43]. The vascular ischemia causes late bladder fibrosis and contraction which can be seen on CT imaging. Radiation also damages smooth muscle cells, causing them to be replaced by fibroblasts, which will lead to decreased bladder compliance. Histologically, these late changes present as a progressive obliterative endarteritis that leads to mucosal ischemia, cellular depletion, and fibrosis. The hypoxia results in tissue breakdown and sloughing of the necrotic bladder mucosa, which leads to hematuria. Telangiectasia also develops which can further contribute to the hematuria. The impaired tissue healing and fibrosis lead to a reduction in bladder capacity and can cause LUTS [44].
Chemically Induced HC
Oxazophorine-Induced HC
There are a wide variety of drugs that have been implicated in the development of hemorrhagic cystitis. The best studied of these agents include the oxazophorine compounds such as cyclophosphamide and ifosfamide. These are alkylating agents that are used in the treatment regimens of several cancers including Hodgkin’s disease, small cell lung carcinoma, and breast cancer. Cyclophosphamide is also used in nonneoplastic disorders such as Wegener’s granulomatosis, systemic lupus erythematosus, and rheumatoid arthritis [45]. The dose-limiting step of the oxazophorine compounds is typically urotoxicity. Hemorrhagic cystitis can develop in up to 40 % of patients after treatment with cyclophosphamide or ifosfamide with the toxicity typically being dose related and occurring within 48 h [46, 47]. In around 4 % of patients, the bleeding can become uncontrollable and even life threatening [48].
The pathophysiological mechanism of oxazophorine urotoxicity involves the breakdown of the drugs into acrolein. Cyclophosphamide and ifosfamide are both metabolized by hepatic microsomal enzymes into a mustard derivative (the antineoplastic metabolite) and acrolein. Acrolein is an unsaturated aldehyde with no significant antitumor activity that is excreted through the urine and can interact with the urothelium to produce toxic effects [49]. Acrolein enters the cells both directly and indirectly (through nuclear factor kappa B and activator protein-1) and causes an increase in reactive oxygen species and nitric oxide, which leads to peroxynitrite production. The increase in peroxynitrite levels causes lipid peroxidation, protein oxidation, DNA strand breaks, and eventual necrotic cell death [50]. Clinically, this causes bladder mucosal edema, vascular dilation, increased capillary fragility, and hemorrhage. This can result in chronic fibrosis of the bladder wall, which may lead to a small, fibrotic, noncompliant bladder [51].
The three main approaches for prophylaxis of oxazophorine-induced hemorrhagic cystitis are sodium 2mercaptoethane sulfonate (mesna), hyperhydration with forced diuresis, and continuous bladder irrigation (CBI). The common mechanism of these 3 methods is to reduce the contact of acrolein with the bladder epithelium. CBI and forced diuresis accomplish this through dilution and forced excretion of the toxic compound. Mesna is a thiol-containing compound that can be coadminstered with cyclophosphamide and ifosfamide. It is excreted into the urinary tract where the sulfhydryl group of mesna can combine with the terminal methyl group of acrolein to form a nontoxic thioether [52]. Mesna works only as a prophylactic method and has no role in treating HC after it has developed. The results of prophylaxis with mesna versus CBI have been examined in a prospective randomized controlled trial. A study of 200 patients receiving either mesna or CBI found that the incidence of hematuria was diminished in the group receiving mesna (76 % vs. 53 %; p = 0.007); however, the incidences of grade 3 and 4 hematuria were the same in each group (18 %). The group receiving CBI also had significantly increased incidence of moderate to severe bladder discomfort/spasms and UTIs compared to group receiving mesna [53]. More recently, a nonrandomized clinical study showed hemorrhagic cystitis occurred in 50 % of patients after prophylaxis with mesna, hydration, and an alkalizing regimen versus 32 % of patients when CBI was added to the prophylaxis regimen (p = 0.11). Moreover, they found that in the CBI group, there was a significant reduction in the mean duration of hemorrhagic cystitis (10 vs. 18 days; p = 0.02), in duration of hospitalization (30.2 vs. 39.6; p < 0.001), and in lateonset hemorrhagic cystitis (p = 0.001) [54]. Future prospects for prophylactic agents include compounds such as amifostine and glutathione as well as a wide variety of plant derivatives such as flavonoids and polyphenols [55].
Other Chemotherapeutics
There are several other chemotherapeutic drugs that are less commonly associated with hemorrhagic cystitis. In all cases, management includes stopping the offending agent and supportive management. Busulfan is an alkylating agent that is used in the treatment of CML and in conjunction with cyclophosphamide as a conditioning agent prior to bone marrow transplantation. It has been reported to cause hemorrhagic cystitis in up to 16 % of patients [56, 57]. Bleomycin, a glycopeptide antibiotic used in the treatment of Hodgkin’s lymphoma, squamous cell carcinoma, and testicular cancer, has been shown to cause HC as well [58, 59]. Temozolomide is an alkylating agent used in the treatment of brain masses and was first reported to be associated with HC in 2002 in a patient being treated for breast cancer with brain metastasis [60]. Docetaxel is a microtubule inhibitor used in treating hormone-independent prostate cancer and, in rare cases, has been shown to cause HC [61]. Cabazitaxel is a microtubule inhibitor used in prostate cancer patients who have developed resistance to docetaxel. There are reports of patients starting this drug and developing HC soon after. Of note, all patients who developed HC after starting cabazitaxel had previously undergone radiation therapy for prostate cancer and cystoscopic findings were very similar to that seen in radiation-induced HC. In all patients, however, symptoms resolved after cabazitaxel was discontinued [62]. Given the timeline of development and resolution of symptoms, it seems that cabazitaxel precipitated radiation HC. Gefitinib, an EGFR inhibitor used in treating non-small cell lung cancer, has been shown to precipitate HC – discontinuation of the agent led to resolution of symptoms [63].
Miscellaneous Drug Agents
Along with chemotherapeutic agents, other medications have been shown to cause HC. In rare cases, penicillins have precipitated hemorrhagic cystitis, though this has only been reported in severely ill patients. This reaction is thought to be caused by an immune-mediated process – all patients were reported to have eosinophilic infiltration on the bladder wall along with peripheral eosinophilia. Immunofluorescent staining of the submucosal tissue shows the presence of immunoglobulin G and M along with C3 [46]. Piperacillin, methicillin, carbenicillin, ticarcillin, and penicillin G have all been associated with HC [64, 65]. Symptoms typically begin 2–4 weeks of starting the antibiotic and resolution of symptoms occurring with discontinuation of the drug [66–69]. Of note, all patients reported to have penicillin-associated HC were being treated for severe systemic infection, suggesting that the systemic inflammatory response played some role in precipitating the hemorrhagic event. However, with the limited amount of data on the topic, further research is needed to determine the exact mechanism involved. Danazol, a synthetic steroid, was shown to cause hemorrhagic cystitis in 19 % of a series of patients with hereditary angioedema. Neither the dose nor the duration of danazol treatment affected the severity, and in all the patients but one, the symptoms resolved after discontinuation of the drug [70]. Tiaprofenic acid is a nonsteroidal anti-inflammatory drug used in the treatment of osteoarthritis and rheumatoid arthritis. It can cause hemorrhagic cystitis with reports of onset ranging from 2 days to 3 years after starting the drug. As with most medications, stopping the drug will most often reverse the symptoms [71]. Cystoscopic and biopsy findings are similar to interstitial cystitis.
Topical agents that are introduced into the bladder can also cause hemorrhagic cystitis through direct irritation of the bladder mucosa. Nonoxynol-9 is a spermicide used as a vaginal contraceptive suppository. Accidental insertion into the bladder causes hemorrhagic cystitis due to the acidic nature of the suppository [72, 73]. All patients presented with acute onset of LUTS and gross hematuria. Cystoscopic findings reveal diffuse inflammation of the bladder mucosa with decreased bladder volumes and associated ulceration and hemorrhage. Ether has been used to declog Foley balloon ports. Rupture of the balloon can result in an ether cystitis that can be resistant to treatment [74, 75]. The effects on bladder function can be so severe that bladder augmentation can be needed to restore normal micturition.
Occupational Agents
Occupational exposure to toxic compounds is known to cause HC. o- and p-toluidine, organic compounds used in the synthesis of chemical dyes, have a well-known association with hemorrhagic exposure. As the geopolitical industrial climate has shifted and manufacturing is moved overseas, the incidence of HC is becoming rarer and rarer in the United States while there are increasing reports coming from nations with large manufacturing industries [76, 77]. Chlordimeform, a pesticide used against ticks and moths, has also been reported to cause HC after occupational exposure. Cystoscopic findings are consistent with acute inflammatory changes and hemorrhage, and symptoms usually resolve with conservative management [78]. Organophosphate toxicity, which is well known for its anticholinergic symptoms, has recently been shown to cause grade IV HC. CT imaging reveals inflammatory changes of the bladder and ureters. Given the acute nature of the insult, symptoms resolve with conservative management [79].
Abuse of the anesthetic agent ketamine, an NMDA receptor antagonist that has become increasingly popular in the past decade, is showing a growing association with HC. Multiple case series describe patients who were daily ketamine users presenting with grade III and IV HC. CT imaging revealed classic inflammatory changes including diffuse bladder wall thickening and perivesicular stranding. Cystoscopic examination revealed bladder ulceration, diffuse hemorrhage, and reduced bladder capacities. Biopsy showed acute and chronic inflammation with an eosinophilic infiltrate suggesting a possible allergic mechanism. Cessation of use along with oral hyaluronic acid led to improvement of symptoms [80].
Management
Overall Management
The initial management of HC begins with careful history, physical examination, and labs as needed to determine not only the underlying etiology but also the degree of the blood loss, as patients should be resuscitated appropriately with fluids and/or blood product based on standard critical care guidelines. Urinalysis and urine culture should be performed, and all patients should be presumed to have urinary tract infection until culture data shows otherwise. Diagnosis should rule out other conditions including medical renal disease, UTI, urolithiasis, coagulopathy, and neoplasm of the bladder or upper urinary tract. In cases of bleeding caused by these mechanisms, treatment of the underlying disorder leads to resolution of symptoms. Even in such cases, hemorrhage itself must be managed and can be done so using the same algorithm used in all other forms of HC.
In determining appropriate management strategies, it is important to understand the severity as well as chronicity of the symptoms. In grade I and II hematuria, management involves treating the underlying cause combined with increased fluid intake. Increased fluids dilute the urokinase found in urine allowing bleeding to resolve with normal coagulation. In patients with grade III and IV HC (Table 24.1), treatment by a urologist is often necessary. These patients are characterized by hemorrhage severe enough to cause urinary retention secondary to clot obstruction of the bladder neck and urethra.
Prevention
Of course, the ideal strategy would be that of prevention. For patients undergoing radiation treatment, this involves tailoring the treatment as much as possible to the region of interest and limiting the dose delivered to the bladder. For chemical-induced cystitis, such as that caused by acrolein, minimizing exposure through treatments that are very effective (i.e., mesna) is the best treatment as it prevents HC. In many patients, once chronic changes are present, they are irreversible and the effect of urokinase in the urine on the underlying bladder muscle and vasculature propagates a cycle of irritation, causing hemorrhage that is very difficult to control.
Initial Bedside Management
Irrigation and Clot Evacuation
When bleeding is severe enough to warrant urologic consultation, care should follow as such. Residual hematoma and urinary stasis provide an excellent culture medium for bacteria to grow, and patients can quickly progress to urosepsis, and again, the treatment of any possible infection is of utmost importance. In the setting of ongoing hemorrhage or urinary clot obstruction, bladder irrigation at the bedside is warranted using a large, stiff-walled catheter as one must evacuate and remove all clots from the bladder [54]. Given that the bladder wall is friable and delicate in HC, the urologist should always be weary of bladder perforation, especially in the case of a chronically fibrotic, shrunken bladder that may be seen in late-stage radiation cystitis. Irrigation is usually performed with a large, catheter-tipped syringe and should continue until there is no clot remaining, and this can often require multiple liters of irrigation.
Continuous Bladder Irrigation
Once all clots have been removed, patients who continue to have low-volume bleeding should be placed on continuous bladder irrigation. It is often the practice of these authors to place patients on continuous bladder irrigation (CBI) for at least several hours if we are consulted for severe HC that requires catheter placement and irrigation. The rate of irrigation can be titrated by nursing staff as long as the urine remains free of clot. Once bleeding has resolved and the urine has remained free of blood for 24 h, the catheter can be removed. If bleeding is persistent for greater than 24 h and requires multiple hand irrigations, then cystoscopy and fulguration under anesthesia or intravesical installation should be considered. If the clinician is concerned that all of the clot is not able to be removed, then cystoscopy under anesthesia with clot evacuation and fulguration is most likely the best next step. This is because intravesical treatments are not likely to work with residual clot in the bladder. However, if the clinician feels that the clot is removed but it is continuously bleeding that is necessitating the CBI, then intravesical therapies may be a good next option as there are some that do not require anesthesia. It is most likely that a patient with grade IV HC will need cystoscopic clot evacuation before proceeding to possible bedside intravesical instillations to ensure clots are removed.
Bedside Intravesical Instillations
Aluminum (Alum)
Aluminum salts can control bladder hemorrhage by causing protein precipitation at the cell surface and within the interstitial space. The resulting vascular protection reduces edema, inflammation, and exudate, all of which contribute to the promotion of further bleeding. As opposed to HA or chondroitin sulfate, alum instillation can be used for severe HC. The first use of intravesical aluminum salt (alum) irrigation is described in a 1982 report of six patients with severe HC following radiation for bladder cancer [81]. Patients were irrigated with a 1 % alum solution in sterile water via a large rigid three-way catheter at the bedside. Subsequent reports have confirmed the utility of intravesical alum irrigation with minimal adverse events [82]. The precipitates formed after alum instillation can cause catheter obstruction, and in rare cases, alum irrigation has been reported to cause systemic side effects including anemia, osteomalacia, and renal failure with associated encephalopathy [83, 84]. Alum should be instilled utilizing a 1 % solution intravesically with a rate of 250–300 ml/h to prevent clotting of the tubing. Clinicians should be checking serum alum levels as well as neuro checks for signs of aluminum toxicity. These signs include lethargy, confusion, seizures, and metabolic acidosis. Clinicians should be cautious of using alum in patients with renal failure as well as patients with significant allergic history.
Amicar
Another agent that can be used at the bedside for intravesical irrigation is ε-aminocaproic acid (Amicar), which is a lysine derivative that acts as an inhibitor of tissue plasminogen and related enzymes. Amicar is particularly useful in HC as it also inhibits urokinase, which, as discussed above, is an integral component of propagating bladder hemorrhage. A study of 37 patients with refractory HC treated with intravesical Amicar showed resolution of bleeding in 89 % of subjects. Patients were treated with 200 mg/L solution of Amicar in normal saline irrigated continuously until 24 h after bleeding resolved [85]. An important consideration in planning treatment with Amicar is ensuring that the bladder is clot-free prior to therapy, as Amicar causes hardening of clots making them difficult to remove. Thus, patients being considered for Amicar should undergo clot evacuation either by hand irrigation or cystoscopically and then be placed on CBI in preparation for treatment.
Procedural Interventions
Cystoscopy and Fulguration
Electrocautery
In those patients whose bleeding does not resolve, or clot removal is not possible with hand irrigation, cystoscopic intervention with electrocautery fulguration of bleeding sites and clot evacuation is indicated [86, 87]. Care should be taken as the underlying tissue can be very friable and bladder perforation can occur. Though the data is sparse, approximately 60 % of patients will see resolution of bleeding after a single treatment with cystoscopic clot evacuation. However, patients requiring further clot evacuations have a significantly reduced chance of responding and often require more aggressive means of treatment [88].
Nd:YAG
Nd:YAG is utilized and has been reported as effective option. However, the mechanism for its effect is thermal coagulation and thus, the tissue will eventually slough just as it will with electrocautery and then must heal. This is a concern in patients with radiation-induced cystitis where healing may be affected [89].
Argon Beam
Greenlight KTP Laser
A recent report has described 10 patients with refractory radiation-induced HC treated with Greenlight KTP laser coagulation, which is traditionally used in transurethral resection of the prostate for benign prostatic hyperplasia. In this series, 9 out of 10 patients had no recurrence of bleeding at 6-month follow-up [92]. Another retrospective review of 20 patients showed that the KTP laser was able to selectively ablate the vasculature while persevering the overlying mucosa. Ninety-two percent of the patients had successful treatment with average hematuria-free periods of 11.8 months [89].
Intravesical Therapy Refractory
Intravesical formalin has been extensively studied and has demonstrated excellent results in treating HC that is refractory to conservative measures [93]. Formalin is an aqueous solution of formaldehyde and acts similarly to alum when instilled in the bladder. It causes precipitation of cellular proteins [94] and its fixative properties stabilize the telangiectatic changes seen in HC. Its use was first described in 1969 [95] – a 10 % formalin solution was used in patients with severe HC and improvement in symptoms was seen in 90 % of those treated. Since the initial study, variations to treatment protocols, including formalin concentration as well as contact time and subsequent irrigation, have been studied. It has been shown in these studies that intravesical formalin is highly effective in controlling severe HC with success rates of 80–93 % [96]. Of note, formalin instillation is extremely painful, and either general or spinal anesthesia is required during instillation. General principles of formalin instillation include the following:
Make sure all clots removed from the bladder and fulgurate any obvious bleeding vessels.
Protect external skin areas such as vaginal packing to prevent leakage around catheter and Vaseline to skin around penis.
Perform cystography to make sure vesicoureteral reflux (VUR) is not present.
Start with a low concentration (1–2 %) and repeat with incrementally increased concentrations as necessary.
Minimize the volume of formalin used.
Minimize formalin dwell time in the bladder (15 min).
In our experience, obstruction of the ureters with ureteral dilators prior to instillation is another effective approach to minimizing VUJ/ureteric complications.
The major limiting factors to the use of formalin include local and systemic complications, which include a small and contracted bladder, incontinence, vesicoureteral reflux (VUR), ureteral strictures, acute tubular necrosis, urinary fistulas, bladder perforation, and toxic effects on the myocardium [97–104]. Using a lower concentration of formalin and minimizing exposure to the ureters and vesicoureteral junction can minimize many of these side effects [105]. Patients with radiation-induced HC have been shown to require higher concentrations of formalin and/or repeat instillations compared with bleeding secondary to cyclophosphamide or bladder cancer.
In patients with focal areas of bleeding, formalin-soaked pledgets were applied cystoscopically. Similar to instillation, lower concentrations appear to be equally effective – use of 4 % formalin was equally effective as 10 % [105].
Other Intravesical Options
Silver nitrate, which is commonly used to treat bleeding wounds at the bedside, can also be used intravesically. The data is sparse, but one study showed improvement in eight out of nine subjects [106]. There are reports of patients suffering subsequent renal failure secondary to precipitation of silver salts in the ureters [107]. Renal function improved after ureteroscopic removal of precipitates, but this complication emphasizes the importance of ruling out VUR prior to intravesical therapy. Irrigation with phenol has also been described in a case report [108], though the deleterious effects of phenol persisting in the bladder require neutralization and large-volume irrigation following instillation [109]. Given the paucity of data and significant risks, this is not a recommended treatment modality.
Intravesical prostaglandin has been described both in the United States and abroad to be effective in treating refractory HC. Though the exact mechanism is not known, it is thought that prostaglandins cause vasoconstriction and promote platelet aggregation. These agents are especially useful as they can be administered at the bedside, have very few associated adverse effects, and are generally well tolerated by patients [110]. A 1984 report describes a BMT patient with refractory HC who had previously required multiple transfusions and failed conservative management. The patient’s bladder was filled with a 3.75 mg/L solution of PGE2 in normal saline, which remained in place for 4 h before being drained. This was repeated for 5 days, at the end of which hematuria resolved [111]. PGE1 and PGF2-alpha have also been reported to be effective [110, 112, 113




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree