Hip and Thigh Anatomy
The hip joint is a synovial articulation between the acetabulum of the pelvis and the proximal femur. The joint recess extends from the acetabulum over the femur to the level of the intertrochanteric line, just beyond the femoral neck. The joint capsule becomes thickened from the iliofemoral, ischiofemoral, and pubofemoral ligaments ( Fig. 6.1 ), and a reflection of the joint capsule extends proximally along the femoral neck. The femoral head is covered by hyaline cartilage, whereas the acetabulum is lined by hyaline cartilage in an inverted U shape with a fibrocartilage labrum attached to the acetabular rim.

Several muscles originate from the pelvis and extend across the hip joint, and others originate from the femur itself. Muscles that originate from the posterior surface of the ilium are the gluteus minimus (which inserts on the anterior facet of the greater trochanter), the gluteus medius (which inserts on the lateral and superoposterior facets of the greater trochanter), and the gluteus maximus (which inserts on the posterior femur gluteal tuberosity below the trochanters and iliotibial tract) ( Figs. 6.2 and 6.3 ). Posteriorly, the piriformis originates from the sacrum and extends inferior and lateral to insert onto the greater trochanter. Other muscles inferior to the piriformis that extend from the pelvis to the proximal femur include the superior gemellus, obturator internus, inferior gemellus, obturator externus, and quadratus femoris.


At the anterior aspect of the hip joint, the iliopsoas can be seen as a continuation of the iliacus and psoas major, which inserts on the lesser trochanter, although the anatomy is complex with independent muscle bundles. Other anterior muscles include the sartorius (which originates from the anterior superior iliac spine of the pelvis and inserts on the medial aspect of the proximal tibia) and the tensor fasciae latae (which originates from the posterolateral aspect of the ilium and inserts on the iliotibial tract, which, in turn, inserts on the proximal tibia) ( Fig. 6.4 ). The rectus femoris has two origins: a direct or straight head, which originates from the anterior inferior iliac spine; and an indirect or reflected head, which originates inferior and posterior to the anterior inferior iliac spine from the superior acetabular ridge. Distally in the thigh, the direct tendon forms an anterior superficial tendon with unipennate architecture, whereas the indirect tendon forms the central tendon with bipennate architecture. The rectus femoris distally combines with the vastus medialis, vastus lateralis, and vastus intermedius musculature (which all originate from the femur) to form the quadriceps tendon, which inserts on the patella with superficial fibers continuing distally over the patella (termed the prepatellar quadriceps continuation ) to the tibial tuberosity by way of the patellar tendon.
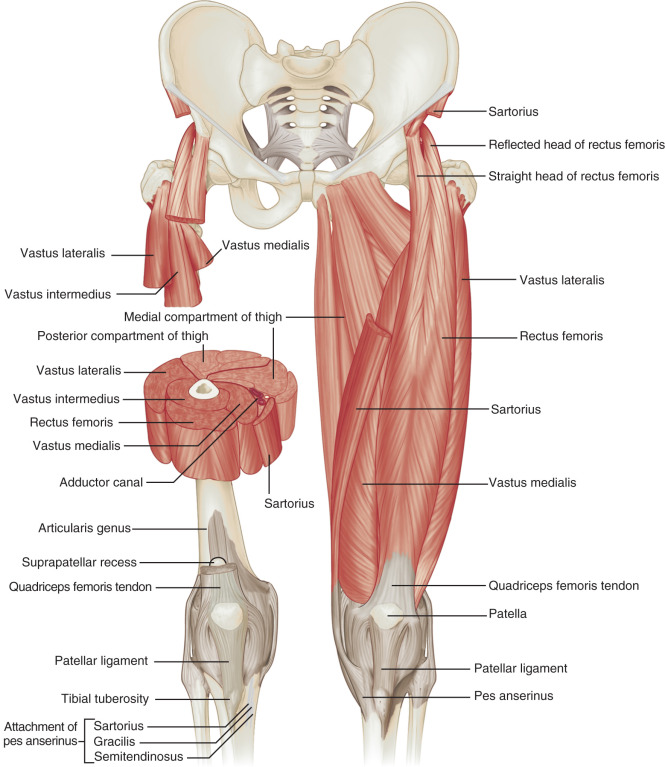
Medially, the adductor musculature includes the adductor longus, the adductor brevis, and the adductor magnus, which originate from the ischium and pubis of the pelvis and insert on the femur at the linea aspera and, in the case of the adductor magnus, the adductor tubercle as well. Superficial and medial to the adductors, the gracilis muscle extends from the inferior pubic ramus to the proximal tibia as part of the pes anserinus.
The posterior thigh musculature, from medially to laterally, consists of the semimembranosus, the semitendinosus (both of which originate from the ischial tuberosity and insert on the proximal tibia, with the semitendinosus being part of the pes anserinus), and the biceps femoris (with long head origin from the ischial tuberosity and short head origin from the femur; the biceps femoris inserts on the fibula and lateral tibial condyle) ( Fig. 6.5 ). Proximally, the semimembranosus tendon is located anterior to the conjoined biceps femoris–semitendinosus tendon and the semitendinosus muscle belly; the semimembranosus origin on the ischium is anterolateral to the conjoint tendon origin.

Other important structures of the anterior hip and thigh include (lateral to medial) the femoral nerve, artery, and vein (use the mnemonic NAVEL for n erve, a rtery, v ein, e mpty space, l ymphatics). A branch of the femoral nerve, the saphenous nerve, courses deep to the sartorius muscle and becomes subcutaneous inferior to the knee. The sciatic nerve is seen in the posterior thigh adjacent to the biceps femoris muscle, where it bifurcates as the tibial nerve and the common peroneal nerve laterally.
Several bursae are located about the hip. The iliopsoas bursa is located anteriorly along the medial aspect of the psoas major tendon of the iliopsoas complex and normally communicates with the hip joint in up to 15% of the population. The trochanteric (or subgluteus maximus) bursa is located posterolateral over the posterior and lateral facets of the greater trochanter deep to the gluteus maximus and iliotibial tract, whereas smaller subgluteus medius and subgluteus minimus bursae are located between the lateral facet and gluteus medius, and the anterior facet and gluteus minimus, respectively (see Fig. 6.16 ). Other more variable bursae exist about the proximal femur as well. Other possible bursae include the obturator externus bursa, located medially and inferior to the femoral neck, which may communicate with the posteroinferior hip joint. An ischial (or ischiogluteal bursa) is found superficial to the ischial tuberosity.
In the inguinal region, the inguinal canal represents a triangular, elongated passage in the lower abdominal wall located just superior to the inguinal ligament ( Fig. 6.6 ). The inguinal canal’s posterior opening, the deep inguinal ring , is located laterally, whereas the anterior opening, called the superficial inguinal ring , is located medially near the pubis. The contents of the inguinal canal include the ilioinguinal nerve, as well as the spermatic cord in males and the round ligament in females. The deep inguinal ring is located just lateral to the origin of the inferior epigastric artery from the external iliac artery. The inguinal (or Hesselbach) triangle is demarcated by the lateral margin of the rectus abdominis medially, the inguinal ligament inferiorly, and the superior epigastric artery laterally. Another structure near the inguinal ligament is the lateral femoral cutaneous nerve, which exits the pelvis to extend over the lateral thigh in a somewhat variable manner. Although most common medial, it may also course superficial or lateral to the anterior superior iliac spine with variable branching.

Ultrasound Examination Technique
Table 6.1 is a checklist for hip and thigh ultrasound examination. Examples of diagnostic hip ultrasound reports are shown in Boxes 6.1 and 6.2 .
Examination: Ultrasound of the Right Hip
Date of Study: March 11, 2016
Patient Name: Jack White
Registration Number: 8675309
History: Hip pain, evaluate for bursitis
Findings: The hip joint is normal without effusion or synovial hypertrophy. Limited evaluation of the anterior labrum is unremarkable. No evidence of iliopsoas bursal distention or snapping iliopsoas tendon with dynamic imaging. The remaining anterior tendons, including the rectus femoris and sartorius, as well as the adductors, are normal.
Evaluation of the lateral hip is normal. No evidence of abnormal bursal distention around the greater trochanter. The gluteus minimus and medius tendons are normal. No abnormal snapping with dynamic evaluation.
Impression: Unremarkable ultrasound examination of the hip.
Examination: Ultrasound of the Right Hip
Date of Study: March 11, 2016
Patient Name: Brennan Huff
Registration Number: 8675309
History: Hip pain, evaluate for tendon tear
Findings: There is a partial tear of the adductor longus origin at the pubis. No evidence of full-thickness tear or tendon retraction. The common aponeurosis and rectus abdominis tendon are normal, as is the pubic symphysis.
The hip joint is normal without effusion or synovial hypertrophy. There is a possible tear of the anterior labrum. No paralabral cyst. No evidence of iliopsoas bursal distention or snapping iliopsoas tendon with dynamic imaging.
Evaluation of the lateral hip is normal. No evidence of abnormal bursal distention around the greater trochanter. The gluteus minimus and medius tendons are normal. No abnormal snapping with dynamic evaluation.
Impression:
- 1.
Partial-thickness tear of the proximal adductor longus.
- 2.
Possible anterior labral tear. Consider MR arthrography if indicated.
General Comments
Ultrasound examination of the hip and anterior thigh is completed with the patient supine; the patient is prone for evaluation of the posterior thigh. For evaluation of the greater trochanteric region, the patient rolls on the contralateral side. Evaluation of the hip and thigh may be considered as two separate examinations in most circumstances. Hip or groin pain in an athlete may be caused from hip joint pathology, tendon or muscle pathology, osseous injury, or adjacent hernia, and therefore all etiologies should be considered. The choice of transducer frequency depends on the patient’s body habitus. A high-frequency linear probe is preferred to optimize resolution, although with a large body habitus a transducer of less than 10 MHz may be needed to penetrate the soft tissues adequately; a curvilinear transducer in this latter setting provides a larger field of view and is also helpful when guiding percutaneous needle procedures. A lower frequency transducer should be considered regardless of body habitus because one should examine the entire depth of the soft tissues before focusing on the more superficial structures. This approach ensures a complete and global evaluation and also serves to orient the examiner to the various muscles, an important consideration because the bone landmarks are few and deep. Evaluation of the hip and thigh may be focused over the area that is clinically symptomatic or relevant to the patient’s history, keeping in mind symptoms may be multifactorial or referred. Regardless, a complete examination of all areas should always be considered for one to become familiar with normal anatomy and normal variants, and to develop a quick and efficient sonographic technique.
Hip Evaluation: Anterior
The primary structures evaluated include the hip joint and recess, iliopsoas complex and bursa, proximal thigh musculature origin in the hip region (rectus femoris and sartorius), and pubic symphysis region. Depending on patient history and symptoms, all of these structures should be considered in the evaluation because symptoms may be referred and etiology multifactorial. Evaluation begins with the anterior hip with the transducer long axis to the femoral neck, which is in the oblique-sagittal plane ( Fig. 6.7A ). To find the femoral neck, one may initially image transversely over the femoral shaft to locate the curved and echogenic surface of the femur and then move the transducer proximally; once the bony protuberances of the greater and lesser trochanter are identified, the transducer is turned to the sagittal-oblique plane parallel to the femoral neck. The hip joint may also be located lateral to the femoral vasculature. The hip joint is identified long axis to the femoral neck by the characteristic bone contours of the femoral head, acetabulum, and femoral neck ( Fig. 6.7B–D ). It is at this location superficial to the femoral neck where the anterior joint recess is evaluated for fluid or synovial abnormalities.



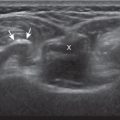
The anterior recess of the hip joint over the femoral neck is normally about 4–6 mm thick, and this can be explained anatomically. The anterior joint capsule extends inferiorly from the acetabulum and labrum and inserts at the intertrochanteric line of the femur; however, some capsule fibers are reflected superiorly along the femoral neck to attach at the femoral head-neck junction ( Fig. 6.8 ). Both the anterior and posterior layers of the joint capsule measure 2–3 mm each in thickness; physiologic fluid between these layers should measure less than 2 mm, and typically no fluid is identified in the normal situation. The anterior layer may be slightly thicker than the posterior layer as a result of capsular thickening from ligaments and the zona orbicularis, which encircles the capsule at the femoral head-neck junction. The posterior layer may also demonstrate focal thickening at its attachment at the femoral head-neck junction. The normal anterior joint recess is usually concave or flat anteriorly but may be convex with internal hip rotation (see Fig. 6.35 ). The true hyperechoic and fibrillar appearance of the joint capsule and its reflection is best appreciated when the femoral neck is perpendicular to the sound beam (see Fig. 6.7C ); if imaged obliquely, the joint capsule may artifactually appear hypoechoic and may simulate fluid in echogenicity, especially in a patient with a large body habitus (see Fig. 6.7B ). The femoral head and neck should be smooth, and the visualized portion of the hypoechoic hyaline cartilage that covers the femoral head should be uniform. The fibrocartilage labrum is hyperechoic and triangular and extends from the margins of the acetabulum (see Fig. 6.7D ). The femoral head and neck are also evaluated in short axis to the femoral neck ( Fig. 6.9 ).




To evaluate the iliopsoas region, the transducer is first placed in the transverse plane over the femoral head because this bone landmark is easy to identify (see Fig. 6.9B ). The transducer is then moved superiorly and angled parallel to the inguinal ligament ( Fig. 6.10 ). The characteristic bone contours are seen, as well as the iliopsoas complex, the rectus femoris origin at the anterior inferior iliac spine laterally, and the femoral vessels medially. The iliopsoas complex is comprised of multiple muscular and tendon components. The muscle identified laterally represents the lateral and medial fibers of the iliacus separated by an intramuscular fascia, while the prominent tendon medially represents the psoas major tendon with its respective muscle tissue seen more medially. The true iliopsoas tendon does not form until more distal. As with imaging any tendon in short axis, toggling the transducer is often helpful to visualize the tendon as hyperechoic, especially because the iliopsoas normally courses deep toward the lesser trochanter and is oblique to the sound beam. The iliopsoas should be evaluated dynamically for tendon snapping (see Snapping Hip Syndrome later in the chapter). The anterior hip is also evaluated for iliopsoas bursa, which originates at the level of the femoral head and typically extends medial and possibly deep to the psoas major tendon and iliopsoas tendon. The transducer is also rotated 90 degrees to evaluate the iliopsoas tendon in long axis; visualization of the distal iliopsoas tendon is improved with the hip in flexion abduction and external rotation (FABER) ( Fig. 6.11 ).




To evaluate the rectus femoris origin, the transducer is returned to the transverse plane over the iliopsoas complex parallel to and at the level of the inguinal ligament (see Fig. 6.10A ) and then moved laterally over the anterior inferior iliac spine. The direct head is seen directly superficial to the anterior inferior iliac spine and is imaged in short and long axis ( Fig. 6.12A and B ) ( ). When moving the transducer laterally from the direct head in long axis, the indirect head will be seen coursing proximal and deep, appearing hypoechoic from anisotropy and producing a characteristic refraction shadow ( Fig. 6.12C ) ( ). One method of evaluating the indirect head of the rectus femoris is to begin anteriorly over the anterior iliac spine short axis to the direct head. The transducer is then moved over the lateral acetabulum in the transverse plane to identify the indirect head and then rotated 30 degrees to visualize the tendon in long axis ( Fig. 6.12D and E ). To evaluate the sartorius, the transducer is returned to short axis relative to the rectus femoris direct head and moved proximally and laterally to visualize the sartorius and its origin on the anterior superior iliac spine ( Fig. 6.13 ).




To evaluate the lateral femoral cutaneous nerve, position the transducer in the transverse plane over the proximal sartorius near the anterior superior iliac spine. As the transducer is moved distally, the lateral femoral cutaneous nerve can be seen as several nerve fascicles coursing over the sartorius from medial to lateral ( Fig. 6.14A ). More distally, a branch of the lateral femoral cutaneous nerve is identified in a triangular hypoechoic fatty space at the lateral aspect of the sartorius adjacent to the tensor fascia latae ( Fig. 6.14B ) ( ). The transducer is then moved proximally to evaluate for potential nerve entrapment at the inguinal ligament ( Fig. 6.14C and D ). The lateral femoral cutaneous nerve may branch proximal to the inguinal ligament and has a variable course. Although most common medial, it may also course superficial or lateral to the anterior superior iliac spine with a variable branching pattern.


Although thigh evaluation is considered separately, patients with hip pain (especially sports-related pain or athletic pubalgia) may have abnormalities at the adductor tendon origin and the rectus abdominis insertion, with possible abnormalities directly associated with the pubic symphysis. To evaluate the pubic symphyseal region, the transducer can be placed transverse the rectus abdominis inferior to the umbilicus. The transducer is centered over one of the rectus abdominis muscles and then rotated 90 degrees in the sagittal plane. The rectus abdominis is followed distally until the echogenic surface of the pubis and overlying common aponeurosis is seen. Angling the transducer laterally at this point toward the adductor tendons can visualize the rectus abdominis, the adductor longus, and the intervening common aponeurosis ( Fig. 6.15A ). The symphysis pubis is then evaluated by rotating the transducer back to the transverse plane and centered over the symphysis pubis ( Fig. 6.15B ). Further assessment of the more distal adductor musculature is discussed with the medial thigh evaluation.

Hip Evaluation: Lateral
To evaluate the soft tissues over the greater trochanter, bone landmarks are essential ( Fig. 6.16 ). The patient lies on the opposite side and the transducer is placed laterally over the hip of interest in the transverse plane ( Fig. 6.17A ). If the greater trochanter is not directly visualized, the transducer can be placed short axis to the femoral shaft more inferiorly. With movement of the transducer cephalad, the characteristic bone contours of the greater trochanter are identified laterally. The key landmark is the apex of the greater trochanter between the anterior and lateral facets, which typically is identified slightly anterior to the lateral hip ( Fig. 6.17B ). Posterior to the lateral facet is the rounded posterior facet of the greater trochanter. The gluteus minimus tendon is identified inserting on the anterior facet, the distal gluteus medius inserting on the lateral facet, and the gluteus maximus superficial but not attaching to the posterior facet. Superficial to the gluteus minimus tendon over the anterior facet is seen the hypoechoic muscle of the gluteus medius and more superficially the iliotibial tract, with the latter appearing as a hyperechoic band of tissue as a continuation of the fascial layers that envelop the gluteus maximus posteriorly and the tensor fascia latae anteriorly ( Fig. 6.16 ). Superficial to the gluteus medius tendon over the lateral facet is seen the iliotibial tract; if the hip is externally rotated, the gluteus maximus will also be visualized over the gluteus medius. Each greater trochanter facet should be evaluated separately in short axis and the transducer should be positioned so that the cortex of each individual facet is perpendicular to the sound beam to eliminate anisotropy of the overlying tendon and to evaluate for distended bursae ( Fig. 6.17C ).


The subgluteus minimus bursa, subgluteus medius bursa, and trochanteric (subgluteus maximus) bursa are located between each respective tendon and their greater trochanter facet (see Fig. 6.16 ). Because the trochanteric bursa is located between the gluteus maximus and posterior facet, it is essential to position the transducer posteriorly so as not to overlook bursal distention at this site. When distended, the trochanteric bursa may also extend laterally between the gluteus medius tendon beneath the iliotibial tract.
The gluteus minimus tendon is then evaluated in long axis by moving the transducer in short axis over and perpendicular to the anterior facet, visualizing the gluteus minimus tendon, and then rotating the transducer 90 degrees but slightly anterior ( Fig. 6.18A ). The same technique is used over the lateral facet to evaluate the gluteus medius tendon in long axis with the transducer angled slightly posteriorly ( Fig. 6.18B ). Because the gluteus medius tendon is attached to two facets (lateral and superoposterior), the transducer should be moved cephalad and posterior to visualize the full extent of the gluteus medius tendon attachment ( Fig. 6.18C ). In long axis, the gluteus minimus and medius tendons form a “V” moving cephalad (see Fig. 6.2 ).

Hip Evaluation: Posterior
Evaluation of the posterior hip and pelvis is not typically considered part of a routine hip evaluation but rather is guided by patient history and symptoms. Structures of interest include the sacroiliac joints, piriformis, superior gemellus, obturator internus, inferior gemellus, obturator externus, and quadriceps femoris (see Fig. 6.3 ). Evaluation can begin with the sacroiliac joint by first positioning the transducer in midline over the sacrum and then moving the transducer laterally to visualize the posterior sacral foramina and more laterally to view the sacroiliac joint and adjacent posterior ilium ( Fig. 6.19 ) ( ). The posterior sacral foramina are differentiated from the sacroiliac joint by their more medial location as well as the characteristic focal disruptions in the cortex when scanning superior to inferior, which is in contrast to the more lateral and linear cortical disruption of the sacroiliac joint. The superior aspect of the sacroiliac joint is widened at the fibrocartilage or ligamentous articulation ( Fig. 6.19A ), whereas the more inferior true synovial articulation is narrow ( Fig. 6.19B ).

To identify the piriformis, a curvilinear transducer with a frequency of less than 10 MHz is essential given the required depth of penetration. The transducer is first positioned in the transverse plane over the sacroiliac joint, as described, then moved inferior into the greater sciatic notch and angled inferiorly and laterally toward the greater trochanter (see Fig. 6.19C ) to identify the piriformis in long axis (see Fig. 6.19D ). The muscle belly will be located medial to the ilium, while the tendon will be seen directly over the ilium extending to the greater trochanter. Passive hip rotation will assist in its identification because of movement of the tendon and muscle ( and ).
To identify the quadratus femoris, obturators, and gemelli, examination can begin in the transverse plane at the level of the ischial tuberosity and hamstring origin ( Fig. 6.20A ). Lateral to the ischial tuberosity and deep to the sciatic nerve is located the quadratus femoris muscle between the ischium and proximal femur. The obturator externus is located deeper and courses anteriorly. Moving cephalad, the inferior gemellus is seen ( Fig. 6.20B ), followed by the obturator internus ( Fig. 6.20C ), and then superior gemellus. The obturator internus is identified by its unique anatomy coursing medial over the ischial tuberosity and into the pelvis. The relationship between the gemelli and the obturator internus, often considered a single functional unit, is appreciated in their short axis with the transducer in the sagittal plane ( Fig. 6.20D ). If the transducer is moved cephalad again and angled medial and superior toward the sacrum, the piriformis muscle will be seen (see Fig. 6.19C ). In their short axis, from cephalad to caudal, the piriformis, superior gemellus, obturator internus, inferior gemellus, obturator externus, and quadratus femoris are identified deep to the sciatic nerve ( Fig. 6.20D ). The sciatic nerve lies deep to the piriformis but superficial to the other external hip rotators described.

Inguinal Region Evaluation
Sonography of the hip and groin region may also include evaluation for inguinal hernias as patient symptoms are often multifactorial. For example, inguinal hernia and adductor tendon abnormalities often coexist in patients with femoroacetabular impingement. At ultrasound an important landmark for determining the type of inguinal hernia is to identify the Hesselbach triangle, which has its base medially bordered by the lateral margin of the rectus abdominis and its apex laterally formed by the inferior epigastric artery superiorly and the inguinal ligament inferiorly (see Fig. 6.6 ).
To begin, one sonographic technique is to scan in the transverse plane over the mid-abdomen below the umbilicus with the patient supine. At this location, the linea alba is seen as a hyperechoic fascial layer between the rectus abdominis muscles and the transducer is centered over one of the ipsilateral rectus abdominis muscles. The transducer is then moved inferior in the transverse plane, and the inferior epigastric artery will be identified beneath the rectus abdominis coursing from medial to lateral ( Fig. 6.21A ). The inferior epigastric artery is then followed inferiorly and laterally until it joins the external iliac artery, which is the apex of the Hesselbach triangle. This site is a very important landmark; just lateral and superior to this location is the deep inguinal ring ( Fig. 6.21B ). Hernias that originate lateral to the inferior epigastric artery at the deep inguinal ring and extend superficially and medially within the inguinal canal are indirect inguinal hernias. In contrast, hernias that originate in the Hesselbach triangle and move in an anterior direction are direct inguinal hernias.





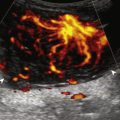
At the deep inguinal ring, the transducer is then angled toward the pubis, parallel and just superior to the inguinal ligament, long axis to the inguinal canal to visualize indirect inguinal hernias if present (see Fig. 6.21C ). In male patients, the serpiginous and mixed-echogenicity spermatic cord can be identified (see Fig. 6.21D and E ). At this location, the patient is asked to tighten the stomach or perform the Valsalva maneuver (forced expiration against a closed airway) to evaluate for transient herniation of intra-abdominal structures or tissue; the patient can be asked to blow against the back of the hand and puff the cheeks outward. This maneuver is also repeated with the transducer directly over the Hesselbach triangle to evaluate for direct hernias. Identification of inguinal hernias must also be confirmed in the sagittal plane to avoid several diagnostic pitfalls. When imaging the inguinal canal and spermatic cord (in males) in short axis, an indirect inguinal hernia will be seen moving in and out of the ultrasound plane displacing the spermatic cord. Similar to the transverse plane, a direct hernia will appear as focal abnormal anterior movement, which must be differentiated from non-focal movement of intra-abdominal fat.
For evaluation of femoral hernias, the transducer is again positioned long axis to the inguinal ligament (see Fig. 6.21F ) and moved distally over the common femoral artery just beyond the inguinal ligament during Valsalva maneuver. An adequate Valsalva maneuver is confirmed if the femoral vein distends. Ultrasound evaluation of other types of ventral abdominal hernias, such as Spigelian (located between the rectus abdominis and lateral abdominal musculature), umbilical, and incisional are usually directed by patient symptoms. Although the causes of “sports hernia” are debated, abnormality of the common aponeurosis is the predominant finding in athletic pubalgia , which is described earlier in evaluation of the symphysis pubis.
Thigh Evaluation: Anterior
Structures of interest anteriorly in the thigh include the four muscles that make up the quadriceps femoris (see Fig. 6.4 ). Examination can begin in the transverse plane over the mid-anterior thigh, where the four individual muscles can be identified ( Fig. 6.22A ) ( and ). Directly below the transducer and most superficial is the rectus femoris muscle ( Fig. 6.22B ). Deep to this and immediately adjacent to the femur is the vastus intermedius. Lateral to these two structures is the vastus lateralis ( Fig. 6.22C and D ), and medial is the vastus medialis ( Fig. 6.22E and F ). Muscle at ultrasound is predominantly hypoechoic, although interspersed hyperechoic fibroadipose septa are identified.






The quadriceps femoris is then evaluated in long axis ( Fig. 6.23 ). As one moves the transducer distally, the rectus femoris tapers to a tendon, followed by the vastus musculature, which forms the trilaminar quadriceps tendon that inserts on the superior pole of the patella. The superficial layer of the distal quadriceps tendon is made up of the rectus femoris, the middle layer is composed of both the vastus medialis and lateralis tendons, and the deep layer is made up of the vastus intermedius tendon. Some quadriceps tendon fibers continue over the patella (termed the prepatellar quadriceps continuation ) to attach to the tibial tuberosity by means of the patellar tendon. The distal tapering appearance of the rectus femoris is best appreciated in long axis in the sagittal plane. The individual muscles of the quadriceps can then be evaluated more proximally.


As described earlier, the rectus femoris tendon proximally originates at the ilium (see Fig. 6.12 ), where its direct head originates from the anterior inferior iliac spine and the indirect head originates laterally at the superior acetabular ridge. In the thigh, the direct head flattens superficially, the indirect head continues as the central aponeurosis of the rectus femoris, and more distally a posterior aponeurosis forms (see Fig. 6.22B ). The adjacent tensor fasciae latae is seen lateral to the rectus femoris muscle ( Fig. 6.24 ); the fascia of the tensor fascia latae continues laterally as the iliotibial tract (see Fig. 6.16 ).

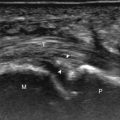
Thigh Evaluation: Medial
Structures of interest in the medial thigh include the femoral nerve, artery, and vein and the sartorius, gracilis, and adductor musculature. Ultrasound examination can begin with the anterior thigh as mentioned for orientation and initial identification of the rectus femoris muscle. The transducer is then moved cephalad into the medial upper thigh (see Fig. 6.22E ). The femoral artery is identified at the medial aspect of the rectus femoris and vastus medialis muscles and is a very helpful landmark ( Fig. 6.25A ). Directly superficial to the femoral artery is the sartorius muscle. Medial and posterior to these structures are the adductor muscles ( Fig. 6.25B ). The most anterior is the adductor longus, next posterior is the adductor brevis, and most posterior and largest is the adductor magnus. One mnemonic to describe the order of adductor muscles from anterior to posterior is “ALABAMa” ( a dductor l ongus, a dductor b revis, a dductor m agnus). Between these respective muscles are located the anterior and posterior branches of the obturator nerve. Superficial and medial to the adductor muscles is the gracilis muscle, just below the subcutaneous tissues ( Fig. 6.25C ). The saphenous nerve can be identified in the distal medial thigh as it crosses from anterior to posterior deep to the sartorius and superficial to the gracilis ( Fig. 6.25D ), becoming subcutaneous adjacent to the great saphenous vein below the knee ( Fig. 6.25E ) ( ). For each of these medial thigh muscles, the proximal to distal extents can be visualized in short axis. The transducer can also be turned in long axis over each muscle to visualize the proximal origins and distal attachments ( Fig. 6.25F ).



Thigh Evaluation: Posterior
Structures of interest in the posterior thigh include the semimembranosus, the semitendinosus, the biceps femoris, and the sciatic nerve. Ultrasound evaluation can begin in the transverse plane at three different levels: the gluteal fold, the ischial tuberosity, or the mid-posterior thigh.
Gluteal Fold and Ischial Tuberosity
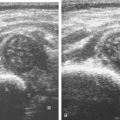
If the transducer is placed in the transverse plane at the gluteal fold ( Fig. 6.26A ), the characteristic appearance of the semimembranosus tendon and aponeurosis is identified deep to the semitendinosus muscle, which is a helpful landmark for orientation. In addition, the conjoined biceps femoris long head–semitendinosus tendon, the semimembranosus tendon, and the sciatic nerve are in the arrangement of a triangle. The semimembranosus is medial and the sciatic nerve lateral forming the base of the triangle, and the conjoined biceps femoris–semitendinosus tendon is the more superficial apex ( Fig. 6.26B ). Toggling the transducer to eliminate anisotropy is helpful to visualize the tendons as hyperechoic ( Fig. 6.26C ). The adductor magnus tendon can be identified medial to the semimembranosus ( Fig. 6.26B ). As the transducer is moved cephalad toward the ischial tuberosity, the semimembranosus tendon will cross under the conjoined biceps femoris–semitendinosus tendon from medial to lateral ( Fig. 6.26D ).

At the ischial tuberosity in the transverse plane, the conjoined biceps femoris–semitendinosus tendon is seen in short axis and is superficial, whereas the adjacent semimembranosus tendon is lateral and deep on the ischial tuberosity ( Fig. 6.26E ). Lateral to the hamstring tendons is the sciatic nerve and posterior femoral cutaneous nerve, located superficial to the quadratus femoris muscle. Ultrasound evaluation of the proximal hamstring tendons in short axis may be completed from the gluteal fold to ischial tuberosity as described, or one may start at the ischial tuberosity and move caudal, using palpation to assist in initially locating the ischial tuberosity. As another characteristic anatomic finding, if one moves the transducer distal from the gluteal fold, a curvilinear hyperechoic intramuscular raphe is identified within the semitendinosus ( Fig. 6.26F ).
To evaluate the proximal hamstring tendons in long axis, the transducer can be placed in the sagittal plane over the ischial tuberosity ( Fig. 6.27A ). At this site, the conjoined biceps femoris–semitendinosus tendon can be identified at the superficial aspect of the ischial tuberosity ( Fig. 6.27B ). To visualize the semimembranosus tendon, the transducer is moved slightly lateral to the conjoint tendon and angled toward midline ( Fig. 6.27C and D ). The conjoined biceps femoris–semimembranosus tendon and semimembranosus tendon can only be visualized together in long axis over a short segment where they cross just distal to the ischial tuberosity ( Fig. 6.27E ). The sciatic nerve is also identified in long axis laterally and should not be mistaken for tendon ( Fig. 6.27F ). Positioning the transducer superior to the ischial tuberosity and angling slightly medial can identify the sacrotuberous ligament ( Fig. 6.27G ), which has fibers continuous with the conjoined biceps femoris–semitendinosus tendon.


Mid-Posterior Thigh
In the transverse plane centered over the mid-posterior thigh ( Fig. 6.28A ), three distinct muscles can be identified medial to lateral, which are the semimembranosus, semitendinosus, and biceps femoris muscles ( Fig. 6.28B ). The short head of the biceps femoris can be identified deep to the long head at the femoral cortex at the level of the mid-femur, and the honeycomb appearance of the sciatic nerve can be identified between the biceps femoris muscle and the semitendinosus muscle. When the transducer is moved in the transverse plane distally toward the knee, the semitendinosus becomes a round tendon and moves directly superficial to the semimembranosus muscle ( Fig. 6.28C–E ). As the transducer is moved cephalad from the mid-thigh, the biceps femoris short head disappears from view proximal to its femoral origin, and the semimembranosus muscle forms an aponeurosis and tendon that course beneath the semitendinosus muscle as described earlier at the gluteal fold. The individual hamstring muscle can also be imaged in long axis.





Hip Evaluation for Dysplasia in a Child
There are several opinions with regard to the ultrasound technique for hip dysplasia. Whereas one method favors the position of the femoral head and measurements, another emphasizes dynamic evaluation of position and stability using the Ortolani and Barlow maneuvers. Regardless, a minimal examination should include coronal neutral or coronal flexion positions (with optional stress and measurements) and a transverse flexion position with and without stress. An ultrasound protocol for hip dysplasia may be divided into several steps. The first is a coronal view with the hip in neutral position ( Fig. 6.29A ). The resulting image is likened to an egg on a spoon, in which a line drawn from the flat ilium covers at least 50% of the head and an acetabular α angle is greater than 60 degrees ( Fig. 6.29B and C ). The α angle measures the angle between the lateral ilium (baseline) and the acetabular roof line, whereas the β angle measures the angle between the lateral ilium baseline and a line drawn through the hyperechoic labral tip from the lateral acetabulum (inclination line). The ossified acetabulum and proximal femur are hyperechoic with shadowing, and the unossified femoral head and triradiate cartilage of the acetabulum appear speckled and hypoechoic. The second position is in the coronal plane with the hip flexed ( Fig. 6.30A ). In this position, in addition to assessment of the femoral head position, the transducer is moved posteriorly over the triradiate cartilage, and posteriorly directed stress is applied to evaluate for posterior subluxation of the femoral head ( Fig. 6.30B ). In the third position, the hip remains flexed, and the transducer is turned to the transverse plane ( Fig. 6.31A ). In this position, dynamic hip adduction with posteriorly directed stress (the Barlow test) ( Fig. 6.31B ) evaluates for hip subluxation, and hip abduction with anteriorly directed stress (the Ortolani test) evaluates for relocation if there is subluxation or dislocation of the hip.