Humeral Shaft Fractures
Humeral shaft fractures account for 3% to 5% of all skeletal fractures. This chapter will focus on fractures of the shaft. Proximal humeral fractures were discussed in Chapter 9. Distal fractures including intra-articular fractures will be included in Chapter 11.
Mechanism of Injury
There are several unique features of the humerus that present problems with fracture management. First, the humerus is the most freely movable osseous structure in the body. Scapulohumeral motion can exaggerate the already flexible range of motion in the humerus. Second, the humerus functions as a lever; therefore, nearly all stress to the bone is in tension from or is at an angle to the long axis of the bone. Weight-bearing and compression forces are not an issue with regard to fracture treatment. Finally, when the humerus hangs vertically it is influenced by gravity alone allowing realignment of the fracture fragments.
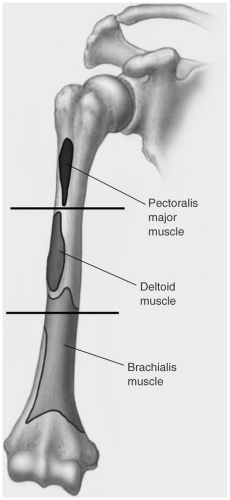
The location of the fracture in relation to the muscle attachments affects the displacement of fragments (see Fig. 10-1). Fractures of the proximal third (between the pectoralis and deltoid muscle insertions) result in medial displacement of the proximal fragment due to pectoralis major muscle forces (see Fig. 10-2). When fractures occur distal to the deltoid muscle attachment, the deltoid muscle forces cause abduction of the proximal fragment. The brachialis and biceps muscles cause proximal displacement of the distal fragment (see Fig. 10-3).
Direct trauma from blunt or penetrating injuries is the most common cause of humeral fractures. Transverse fractures are usually the result of bending forces. Spiral fractures occur due to a combination of bending and rotational forces. Compression forces acting on the humerus tend to affect the proximal or distal portions, but spare the diaphysis. Indirect forces, such as falling directly on the elbow or outstretched hand, vigorous
throwing motions, and violent muscle contractions can also cause humeral shaft fractures. Fractures should be described by location as proximal, middle, distal, or at the junction of the proximal and middle thirds or middle and distal thirds (Holstein-Lewis fracture, see Chapter 2). Forty-three percent to 69% of fractures involve the mid shaft. Of these, 61% are transverse, 18% oblique, 17% spiral, and 4% comminuted or segmental. Thirty percent to 40% percent involve the proximal shaft and 10% to 16% the distal shaft. Fracture incidence has a bimodal distribution with peaks in the third and seventh decades.
throwing motions, and violent muscle contractions can also cause humeral shaft fractures. Fractures should be described by location as proximal, middle, distal, or at the junction of the proximal and middle thirds or middle and distal thirds (Holstein-Lewis fracture, see Chapter 2). Forty-three percent to 69% of fractures involve the mid shaft. Of these, 61% are transverse, 18% oblique, 17% spiral, and 4% comminuted or segmental. Thirty percent to 40% percent involve the proximal shaft and 10% to 16% the distal shaft. Fracture incidence has a bimodal distribution with peaks in the third and seventh decades.
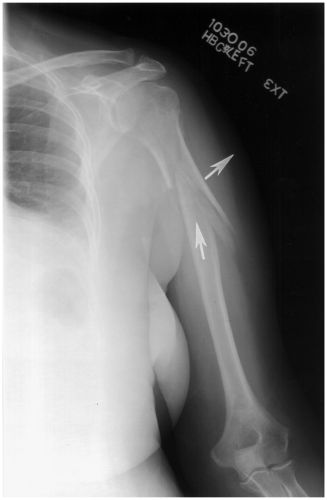
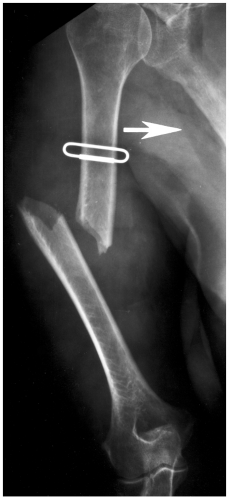 Fig. 10-2 Fracture at the deltoid insertion with adduction of the proximal fragment due to pectoralis muscle forces (arrow). |
Fractures at the junction of the mid and distal thirds are particularly difficult to manage. Injury to the nutrient artery at this level may contribute to delayed union or nonunion. The radial nerve is also at risk for injury at this level. Therefore, open reduction and fixation is more often required compared to more proximal fractures.
Open fractures occurred in 2% to 5% of cases. The severity of injury is classified based on the extent of soft tissue injury using the Gustilo and Anderson lassification listed in the subsequent text. Most are minor open wounds (72%), but 14% are more extensive type II and 14% type III open wounds.
Classification
Most humeral shaft fractures are described by location and fracture line orientation or the degree of comminution. The AO (Arbeitsgemeinshaft fur Osteosynthesefragen)/Orthopaedic Trauma Association (OTA) classifications divide fractures into three large simple categories with multiple subcategories in each type.
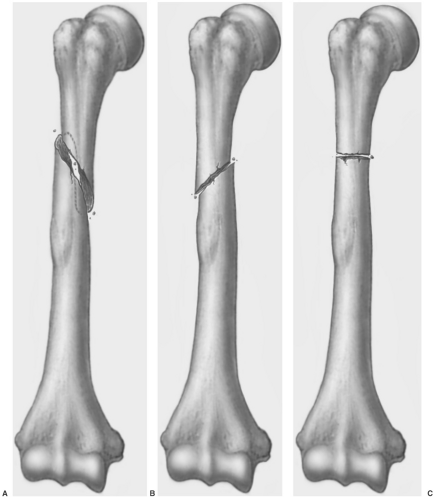
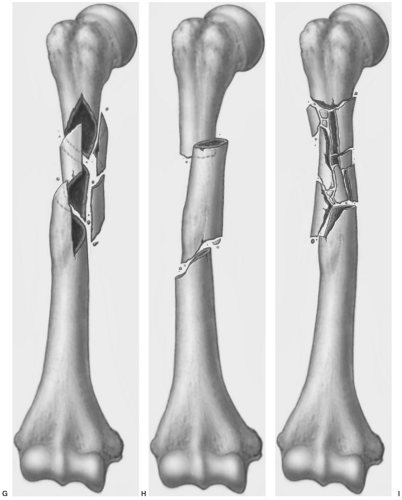
AO/OTA classification (see Fig. 10-4)
Type A: Simple, no comminution (63.3%) (Fig. 10-4A–C)
A1—simple spiral
A2—simple oblique
A3—simple transverse
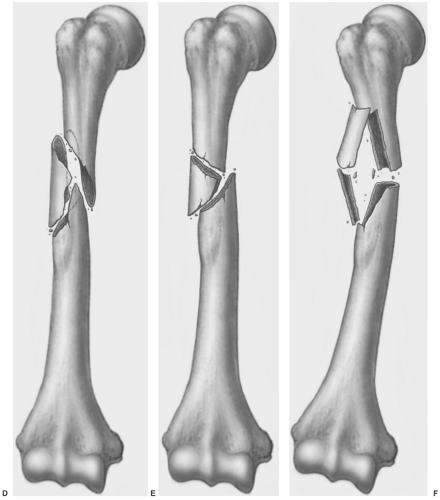
Type B: Wedge (butterfly) fragment (26.2%) (Fig. 10-4D–F)
B1—spiral wedge
B2—bending wedge
B3—fragmented wedge
Type C: Comminuted (10.5%) (Fig. 10-4G–I)
C1—spiral comminuted mid shaft
C2—segmental
C3—irregular shaft comminution
Gustilo and Anderson classification for open fractures
Type I: Open fracture due to fragment penetration and minimal soft tissue damage, wound clean <1 cm (72%)
Type II: Wound >1 cm without extensive soft tissue damage (14%)
Type IIIA: Extensive soft tissue damage with wound >10 cm, periosteum intact (7%)
Type IIIB: Periosteal stripping requiring wound coverage (7%)
Type IIIC: Same as IIIB, but with vascular injury requiring vessel repair (rare)
Suggested Reading
Ekholm R, Adami J, Tidermark J, et al. Fractures of the shaft of the humerus: An epidemiological study of 401 fractures. J Bone Joint Surg. 2006;88B:1469–1473.
Ekholm R, Tidermark J, Tornkvist H, et al. Outcome after closed functional treatment of humeral shaft fractures. J Orthop Trauma. 2006;20:591–596.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five fractures of the long bones. J Bone Joint Surg. 1976;58A:453–458.
Muller ME, Nazarian S, Koch P, et al. The comprehensive classification fractures of long bones. Berlin: Springer-Verlag New York; 1990.
Tytherleigh-Strong G, Walls N, McQueen MM, et al. The epidemiology of humeral shaft fractures. J Bone Joint Surg. 1998;80B:249–253.
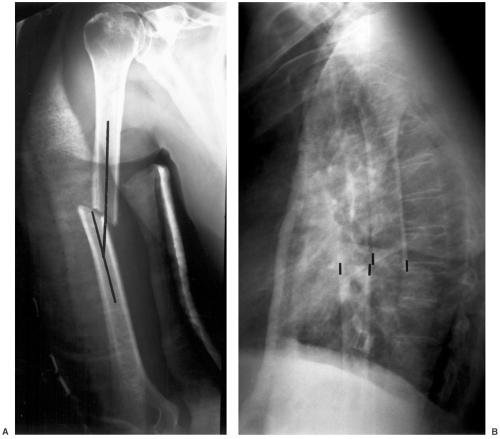
Imaging
Detection and classification of humeral shaft fractures can usually be accomplished with anteroposterior (AP) and lateral radiographs of the humerus. A transthoracic view is an excellent method of obtaining a lateral view at 90 degrees to the AP view. This is especially useful for fractures of the upper
humerus (see Fig. 10-5). The shoulder and elbow need to be included on the images. Depending on the presence of other injuries, it is better to rotate the patient instead of turning the arm to obtain the two different views. Complex fractures (OTA type C) may require computed tomography (CT) or magnetic resonance imaging (MRI) for further evaluation. The former is useful for fragment position and MRI for subtle osseous changes or radial nerve injury. Complex open fractures (Gustilo and Anderson type IIIC) with vascular injury may require angiography to clarify the extent and location of vessel disruption or compression.
humerus (see Fig. 10-5). The shoulder and elbow need to be included on the images. Depending on the presence of other injuries, it is better to rotate the patient instead of turning the arm to obtain the two different views. Complex fractures (OTA type C) may require computed tomography (CT) or magnetic resonance imaging (MRI) for further evaluation. The former is useful for fragment position and MRI for subtle osseous changes or radial nerve injury. Complex open fractures (Gustilo and Anderson type IIIC) with vascular injury may require angiography to clarify the extent and location of vessel disruption or compression.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree